Case Report
Volume 1 Issue 1 - 2017
Four Cases Experience of Fungal Arthritis, Myositis and Mycetoma in An Orthopaedic Tertiary Hospital in Bangkok, Thailand
Department of Medicine, Lerdsin Hospital, Bangkok, Thailand
*Corresponding Author: Thitirat Tangkosakul, Department of Medicine, Lerdsin Hospital, Bangkok, Thailand.
Received: January 07, 2017; Published: January 11, 2017
Abstract
Osteomyelitis, arthritis, myositis and mycetoma may be from many infectious organisms: bacteria, virus and fungus. Myositis can also be caused by parasites. The diagnosis of the specific microbes is often suggested by signs and symptoms, a detailed review of medical record for immunosuppressive drugs, travel history and conducting specific laboratory tests like serology, histopathology and/or cultures. We report here four cases of infections in orthopaedic department caused by Histoplasma Capsulatum, Tremetosphaeria grisea and Cryptococcus neoforman. The first patient has knee arthritis and positive for interferon gamma pathway defect, the second patient have mycetoma of feet. The third and fourth patients have myositis and osteomyelitis near Sartorius muscle and between Gluteus medius and Gluteus minimus muscles. Diagnosis was made with tissue pathology with culture except in the second case in which tissue pathology with polymerase chain reaction and 18S gene sequences were used. All patients were successfully treated with intravenous amphoptericin B and oral itraconazole, fluconazole accordingly.
Keywords: Histoplasmosis; Cryptococcosis; Fungal mycetoma; Fungal osteomyelitis
Introduction
Deep soft tissue of musculoskeletal infection: arthritis, myositis and mycetoma can be caused by wide range of organisms which include bacteria, virus and fungus. Additionally myositis can be caused by parasites. These types of infections present some difficulties to the physician in diagnosing them. Our hospital is located in Bangkok and is an orthopedic-specialized tertiary hospital of The Ministry of Public Health. Thailand has a hot and humid climate. The majority of Thai population works in the agricultural sector. We encounter some difficulties in diagnosing deep soft tissue of musculoskeletal infection cases, which are referred by their primary physicians and the causative organism is fungus. To date, there are only a few reports about fungal infection of musculoskeletal system in Thai patients. The first article is about eight patients who had bone and joint infections caused by Penicillium marneffei in a tertiary hospital in northern Thailand. There was HIV infection in four and chronic alcoholism in one patient. Acute arthritis was seen in three patients, and the other five patients had arthritis and osteomyelitis [1]. The second article is about 149 HIV–infected patients and 29 HIV-uninfected patients who had infections caused by Cryptococcus neoforman. Two of HIV-uninfected patients have bone infection caused by Cryptococcus neoforman [2]. The third article is about 116 HIV infected and 34 HIV-uninfected patients infected with penicillium marneffei. HIV-uninfected patients were more likely to have bone and joint infections such as arthritis, spondylodiskitis and osteomyelitis [3]. In the current study, the author reviewed cases since 2010-2014 in an orthopedic tertiary center in Bangkok, Thailand. We retrospectively retrieved data for patients who were diagnosed of fungal infection of osteomyelitis, arthritis, myositis and mycetoma at our institute. Blood samples were processed in the Multi TOF continuous monitoring blood culture system. Cultures of clinical specimens, including tissue, bone and pus were performed on Sabouraud’s dextrose agar. Visible isolates were subcultured on potato dextrose agar and brain heart infusion agar. Polymerase chain reaction and 18S gene sequences were done at King Chulalongkorn Memorial Hospital while drug susceptibility tests such as MIC for.
Fluconazole, Amphoptericin B by E -test were processed at another institute. Data regarding gender, age, duration of disease, sites of infection and modalities of treatment were collected. Data regarding gender, age, duration of disease, sites of infection and modalities of treatment were collected.
Case series
Since 2010-2014 in an orthopedic tertiary center in Bangkok, Thailand (Table 1) there were 35, 40, 65 and 72-years old patients presented with arthritis, mycetoma, osteomyelities, myositis. One was immunocompromised patient with positive interferon gamma antibody.
| case | Sex/age | Disease | Underlying Disease | Current Medication | Treatment | Outcome |
| 1 | F/35 | Arthritis | IFNц | none | Ampho B 2 wks to itraconazole | improve |
| 2◊ | F/40 | Mycetoma | none | none | Ampho B 4 wks to itraconazole | improve |
| 3◊ | M/65 | Myositis | none | none | Ampho B 4 wks to fluconazole | improve |
| 4◊ | F/72 | Myositis Osteomyelitis |
none | none | Ampho B 2 wks to fluconazole | improve |
Surgical intervention were done in 2nd, 3rd, 4th and 5th patient.
Table 1: Demographic data of five patients in this studies, 2010-2014.
Table 1: Demographic data of five patients in this studies, 2010-2014.
Case1: A 35 year old woman, non-diabetes and HIV-seronegative, presented to our hospital with one-month arthritis at right knee, since April 2014. In September 2013, she was diagnosed with sputum negative pulmonary tuberculosis and was treated with anti-TB drug completely. After that, in January 2014, she came with symptoms of chronic pain around right hip’s area, subsequently the diagnosis of pyogenic abscess was made. The causative organism was Salmonella group B. After the diagnosis of chronic arthritis at right knee was made on April 2014, debridement was done. The tissue was sent to the laboratory, and from Gomeri’s methanamine silver stain, we found it positive for oval yeast cells which liked for Histoplasma capsulatum. Unfortunately, the culture was negative for fungus. During the course of this episode of infection, she also developed cervical lymphadenitis in which tissue culture was positive for Mycobacterium abscessus. We prescribed her with Amphotericin B 50 mg intravenously once a day for 2 weeks and then itraconazole 400 mg per day for one year. We also prescribed her with cefoxitin, azithromycin for carbapenem resistant M.abscessus and her aminoglycoside allergy accordingly. Because of history of multiple infection in this one-year period, and the causative organisms seems to make a clue to suspicions of cellular mediated immunity impairment. We decided to work up for adult immunodeficiency syndrome. Her CD4 absolute count 998 cell/mm3 (32.86%) And the result of antibody to interferon gamma pathway was positive.
Case 2: A female office worker who lived in Bangkok, came to our hospital in June 2010, with the history of minor pain of the palpable mass about 6 cm in diameter at her right ankle and right heel for 2 months without any systemic symptoms. She had no history of diabetes and was HIV-seronegative. In 2008, she had the same symptoms and went to another hospital. Since that time, mycetoma at right ankle was diagnosed. She got an operation to totally remove the mass followed by treatment of antifungal medication for 2 years but loss to follow up with the hospital after that time. At this presentation, we diagnosed mycetoma at right ankle, fulfilled the characteristic triad: tumefaction, multiple draining at sinus and presence of grains. She got debridement and the tissue pathology could be identified as black mold. Unfortunately, the tissue culture for fungus was negative. We use 18S rRNA polymerase chain reaction to detect fungal aetiology instead of culture technique. The result of DNA sequencing demonstrated this mold, Tremetosphaeria grisea. She got amphotericin B 50 mg per day intravenously, followed by itraconazole 400 mg per day for 18 months with no recurrent pain without re-imaging.
Case 3: A 65 year old man came to our hospital in April 2010, because he noticed that his left thigh became progressively swelling with palpable localized mass for three months without pain or other systemic symptoms. We decided to do magnetic resonance imaging at his left thigh, and the finding was mixed solid-cystic lesion, size measured about 15 x 9 x 6 cm. Located within Sartorius muscle. The operation was performed, we partially removed the mass as much as possible and the tissue was sent to pathology and microbiology laboratories. We also incidentally found pulmonary mass from his CXR. From computerized tomography, the mass located in the superior segment of upper lobe of right lung, measured size about 4 x 4 cm. The result of the tissue from his operation, demonstrated yeast-like organism typical for Cryptococcus species and from mucicarmine stain also positive for this type of organism. Blood for cryptococcal antigen titer was 1:1024 but Unfortunately the fungal culture result was negative. He was prescribed with Amphotericin B 502 mg intravenously daily and follow by Fluconazole 400 mg per day for 1 year.
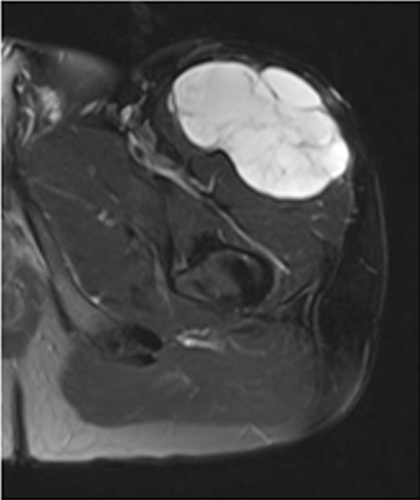
Case4: This non-diabetic, HIV-seronegative female patient admitted to our hospital since June 2010. She is a 72 year old gardener, lived in Saraburi province, located in eastern part of Thailand. She presented with symptoms of progressive chronic pain at area of right hip and weight loss for 6 months. We worked up with MRI at both hip and pelvis. MRI of pelvis showed destruction of iliac crest with abnormal marrow signal, multilobular septated cystic lesion between Gluteus Medius and Minimus muscles consistent with abscess and osteomyelitis. A complete blood count revealed hemoglobin of 11.5 g/dl with white blood cell count of 15,700 cells/mm3 (neutrophils 76%, lymphocytes 14%, monocytes 7%) and a platelet count of 373,000 cells/mm3. Her CD4 absolute count 1706.8 cell/mm3 (61.09%). We set open and drainage operation for her huge abscess. We sent the tissue for pathological study. The result of the tissue from this operation, demonstrated yeast-like organism typical for Cryptococcus species and from mucicarmine stain also positive for this type of organism. The result of fungal culture was Cryptococcus neoforman. In the course of her admission, she had alteration of consciousness and CT brain was done. The CT scan brain’s result: communicating hydrocephalus with leptomeningeal enhancement. Lumbar puncture was performed: CSF proteins 60 mg/dl, CSF sugar 25 mg/dl and blood sugar 88 mg/dl. Serum cryptococcal antigen is positive 1:1024 from patient’s blood. She got Amphotericin B 50 mg intravenous daily for 2 weeks and fluconazole 400 mg per day for one year.
Discussion
The epidemiology and clinical features of patients help in the diagnosis in fungal diseases. They can occur in immunocompetent patients in endemic areas and in patients who are at risk: diabetes, immunosuppression by anti-tumor necrosis factor drug, presence of indwelling catheter, parenteral hyperalimentation, use of broad spectrum antibiotics and HIV infection. Routes of infection are hematogenous dissemination, inoculation during implantation of prosthesis or injection of steroid which typically appear within 4 weeks of the inciting event and direct extension from nearby infected tissues [4]. Mycetoma pathogens are Acremonium falciforme, Scopulariopsis maduromycosis, Pseudallescheria boydii, Trichophyton verrucosum, Madurella mycetomatis and Aspergillusspp. Osteomyelitis and arthritis causes are Candida spp., Cryptococcus spp., and Aspergillus and endemic fungi:
Coccidioides species and Histoplasma spp [5]. Mycetoma mostly affects foot (70%) and occasionally hand, leg, knee, arm, thigh and perineum and rarely sinus, mandible, spine, bladder, brain and lung. Myositis as an infection of skeletal muscle (most commonly affected are the quadriceps, calf and gluteus muscle groups) is uncommon because musculature is relatively resistant. Myositis, osteomyelitis and arthritis may be due to Candida spp., Cryptococcus neoformans, Aspergillus fumigates, Histoplasma capsulatum, Coccidioides spp. and Fusarium spp. [6]. Presentation of fungal infection varies widely, ranging from indolent to rapid destruction; their indolent presentation may be misleading as malignant process. Examples were mentioned in a case report about a patient who had black-grain mycetoma occurring on the lower jaw and misdiagnosed as tumor but was caused by Madurella pseudomycetomatis [5]; and Coccidiomycosis infection of the patella mimicking a neoplasm [7]. Determining the causative organism is imperative to optimizing therapy.
Diagnosis of fungal infections without obtaining specimen by First: imaging is less useful when suspecting fungi - the most frequent radiographic findings are that of multiple lytic punched-out lesions with permeative or moth-eaten borders or sclerotic margin [7]. Only one report noticed that absence of new bone formation and periosteal reaction in osteomyelitic area may be from fungal pathogens [8]. Second: biochemical markers such as d-arabinitol, ß-D glucan which is Candida‘s metabolites may be found in periprosthetic infection but not always used in clinical practice [8]. Third: blood culture is not valuable such as in Candidiasis in which only half of them are positive [8]. Cryptococcal antigens are diagnosed frequently because of HIV-era and estimate of 60% positive blood culture in cryptococcal infection [9]. Fourth: Histoplasma antigen in urine of patients with progressive dissiminated histoplasmosis [10]. The Fifth method, useful for endemic fungi: serology such as coccidioides and Paracoccidioides brasiliensis by complement fixation and enzyme immunoassay method but limitations are immunosuppressive status and sustainability [10].
Identification of the fungus with accessible specimens is traditionally performed by isolation of the fungi. Biochemical test used in bacteria identification is unreliable for fungus. Fungi exhibit high phenotypic pleomorphism depending on culture conditions. Molds which have hyphae appear to be septate or sparsely septate with sporangiophores. The sporangiophore which terminates in swollen vesicles is covered by stalked sporangioles [11]. Yeast or dimorphic fungi have examples for pathognomonic: Coccidioides immitis as large thick walled spherules with endospores in H&E and Gomeri’s methanamine silver stain and Paracoccidioides brasiliensis as pilot’s wheel appearance which are multiple-budding yeast cells with well-defined refringent double walls in fresh samples by using 10% KOH and Grocott-Gomeri stain [12]. Morphologic characteristicsdo not distinguish active infection from past infection except by invasion around tissues [8].
Since the discovery of polymerase chain reaction and DNA sequencing, comparison of the gene sequences of small subunit ribosomal RNA has led to the construction of a universal phylogenetic tree classifying organisms into 3 domains of life: Bacteria, Archaea and Eucarya [13]. Especially, the systematic analyses of Internal transcribed spacer(ITS1, ITS2) and D1/D2 hypervariable regions have been proven to be effective in identifying the pathogenic molds to the species and sequevar levels, while ribosomal genes including 18S and 28S genes which are relatively conserved, provide useful phylogenetic information. Strains with > 1% sequence diversity in the D1/D2 domain or ITS region usually represent separate species [5,15]. The 25S rRNA gene sequences were mostly used for Yeasts and 18S gene sequences used for filamentous fungi [14]. Tissue of mycetoma of the second patient was tested by polymerase chain reaction and 18S gene sequences revealed Tremetosphaeria grisea.
Conclusion
Osteomyelitis, arthritis, myositis and mycetoma caused by fungus is uncommon but clinically important. Cultures of clinical specimens, including tissue, bone and pus were performed on suitable agar. Polymerase chain reaction and 18S gene sequences were additional tests that should be done in case of negative culture.
References
- Louthrenoo W., et al. “Osteoarticular penicilliosis marneffei. A report of eight cases and review of the literature”. British Journal of Rheumatology 33.12 (1994): 1145-1150.
- Jongwutiwes U., et al. “Comparison of clinical features and survival between cryptococcosis in human immunodeficiency virus (HIV)-positive and HIV-negative patients”. Japanese journal of infectious diseases 61.2 (2008): 111-115.
- Kawila R., et al. “Clinical and laboratory characteristics of penicilliosis marneffei among patients with and without HIV infection in Northern Thailand: a retrospective study”. BMC Infectious Diseases 5.13 (2013): 464.
- Nancy F. “Bacterial, Parasite, Fungal, and Viral myositis”. Clinical Microbiology Reviews 21.3 (2008): 473-494.
- Yan J., et al. “Phenotypic and Molecular characterization of Madurella pseudomycetomatis sp. Nov,, a Novel Opportunistic fungus Possibly Causing Black-grain Mycetoma”. Journal of Clinical Microbiology 48.1 (2010): 251-257.
- Horn D., et al. “Aspergillus osteomyelitis: review of 12 cases identified by the Prospective Antifungal Theraply Alliance registry”. Diagnostic Microbiology and Infectious Disease 63 (2009): 384-387.
- Li YC., et al. “Coccidiomycosis infection of the patellamimicking a neoplasm-two case reports”. BMC MED Imaging 18.14 (2014): 8.
- Jason T., et al. “Fungal osteomyelitis and Septic Arthritis”. Journal of the American Academy of Orthopaedic Surgeons 22.6 (2014): 390-401.
- Asanuma Y., et al. “Extradural cryptococcoma at the sacral spine without bone involvement in an immuno;competent patient”. Journal of Orthopaedic Science 19 (2014): 1040-1045.
- Wheat LJ. “Approach to the diagnosis of the endemic Mycoses”. Clinics in Chest Medicine 30.2 (2009): 379-389.
- Navanukroh O., et al. “Disseminated Cunninghamella bertholletiae infection with spinal epidural abscess in a kidney transplant patient: case report and literature review”. Transplant Infectious Disease 16.4 (2014): 658-665.
- von Glehn F., et al. “Carpal Tunnel Syndrome with Paracoccidioidomycosis”. Emerging Infectious Diseases 18.8 (2012): 1390-1392.
- Larsen N., et al. “The ribosomal database project”. Nucleic Acids Research 21.13 (1993): 3021-3023.
- De Rijk P., et al. “Database on the structure of large subunit ribosomal RNA”. Nucleic Acids Research 27.1 (1999): 174-178.
- Lau SK., et al. “Early diagnosis of Exophiala CAPD peritonitis by 18S ribosomal RNA gene sequencing and its clinical significance”. Diagnostic Microbiology and Infectious Disease 46.2 (2003): 95-102.
Citation:
Thitirat Tangkosakul. “Four Cases Experience of Fungal Arthritis, Myositis and Mycetoma in An Orthopaedic Tertiary Hospital
in Bangkok, Thailand”. Clinical Biotechnology and Microbiology 1.1 (2017): 16-21.
Copyright: © 2017 Thitirat Tangkosakul. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.