Research Article
Volume 1 Issue 1 - 2017
The Importance of the Family Approach in General Medicine: An Induction and Review of Concepts from a Case of Hereditary Renal Disease
Specialist in Family and Community Medicine. Health Center Santa Maria de Benquerencia. Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain
*Corresponding Author: Jose Luis Turabian, Health Center Santa Maria de Benquerencia Toledo, Spain.
Received: November 22, 2017; Published: November 30, 2017
Abstract
Under the generic terms of Hereditary Renal Disease or Hereditary nephropathy there are vast spectrums of many different diseases that are transmitted by autosomal dominant or recessive inheritance, or linked to the X chromosome; they have in common two characteristics: the evolution towards the Renal Insufficiency and the capacity to be transmitted from parents to children. Family-oriented care is a "theoretical" trait inherent in general medicine, although there is great variability in practice among these professionals. In this context, a case report of 3 patients in a family is described, to illustrate the condition of hereditary kidney diseases and to reflect and deepen in the induction of the concepts of family care in general medicine.
GPs often meet with patients with suspected or proven hereditary diseases and predispositions, and have to face these diseases that present a greater complexity of management than others, since they must make early diagnosis and genetic counselling, that must be especially careful with the ethical aspects. This determines the need for a wide range of knowledge and skills of GPs for recognizing patients who have relatives with hereditary kidney disease by using a "family history" as surrogate marker for risk of future nephropathy.
Obtaining a thorough family history and records of affected family members by means of a family tree or genogram is especially helpful to allow GPs to see hereditary family diseases and they tools can be use as scientific devices for nosographical classification of hereditary diseases. In these diseases, GPs must bear in mind that their social impact is enormous, because of their potentially recurrent nature in the same family and because of the high socio-sanitary cost derived from the enormous burden of care which requires. Finally, also GPs must take into account that patients' beliefs about symptoms are especially important in hereditary diseases because of the cultural conception of these as "family blemish".
Keywords: Family Medical History; Medical History Taking; Family Health; Family Relationship; General Systems Theory; Genogram; Family Medicine; General Practitioner; Health Risk Assessment; Diseases with a Genetic Nature, Chronic Kidney Disease
Introduction
The importance of the family in the health and illness of its members is not discussed, neither theoretically or conceptually, but most of the work of the general practitioners (GPs) occurs with individuals; in everyday medical practice the family is a frequently forgotten or only partially considered element. Thus, when thinking about assistance or health care, there is a tendency to conceive it as an individual situation. But, of course, this is only a simplification of the importance of the factors that surround the individual [1]. On the other hand, while family history collection is a core responsibility of primary care providers, and family-oriented care is an inherent trait of general practice, GPs offer great variability in their practice regarding family counselling and few details about this practice is known, as well as about the importance of family stories, or intergenerational narratives, and their health benefits across the lifespan [2-7]. Thus, in actual practice, it is common to understand the consultation and approach the patient as an isolated individual who presents a health problem.
However, the family has a lasting impact on the development of the personality; the family forms the personality, attitudes, behaviours and beliefs of the child. The family can be seen as a system in which the total is greater than the sum of its parts. Each person contributes as a unique part to the system, but is also affected by the relationships with the other members. The family unit plays an important role in providing "care" to all its members.
The disease that affects an individual can seriously affect the family unit, and on the contrary, the family unit influences the health of the individual members. An individual's problems are usually best understood when placed in the context of the family. Problems are often shared by more than one individual in the family, and the family itself may hold the key to successful solutions [8-11]. GPs provide care for patients of all ages, from newborns to the elderly. In addition to its wide scope of practice, Family Medicine/General Practice is characterized by its emphasis on understanding of the whole person, its partnership approach with patients over many years, contemplates human life cycle continuously and its command of medical complexity [12-15].
What is traditionally called individual, family and community care are elements of the same reality and can not be separated. All health problems are also individual, group and community at the same time. A basic premise of the Bio-psycho-social model is that the impact on a subsystem - biological, individual, family, and community- affects the rest, both in health and in disease. When greater is the complexity of the problem to be addressed, the greater the need to work with the family group. Even when the patient presents himself only during the visit, with him, virtually, enters his network of relationships that has given rise to his context and beliefs; and the main network of relationships of the person is the family.
The doctor-patient relationship is actually triangular: doctor-patient-family. We must count on the family as a primary element for treatment (hygienic measures, diets, taking drugs, exercise, rest ...). Family is two or more people related or connected biologically, emotionally or legally. The family is the principal of human systems, and it is more than the sum of its individual parts. The family system is composed of subsystems: conjugal (the couple), parental or filial (parents and children), and fraternal (brothers). These subsystems form dyads and triangulations. Systemic family theory emphasizes interaction and context; individuals are seen within the family context, and are interrelated, thus, the causality is circular rather than linear [13].
Families play an essential role in the health and illness of people, to the point that family support can affect the health outcomes of the individual, and sometimes the disease arises in times of family crisis. It is common for the GPs to be consulted by the family about the diagnosis and treatment plans of a member of the family, and therefore must have knowledge and skills to work with families: the systemic theory applied to the family, the life cycle family, maps or diagrams that evaluate family relationships -the genogram-, interview or advice with families. The holistic conception of human phenomena is fundamental for GPs. [16].
Hereditary diseases are those that are transmitted from parents to children through genes, so they can occur in several members of the same family. The risk of recurrence in a direct relative depends on the pattern or form of inheritance that pathology has. In the patients registry of each GP can be found patients whose diseases are with a genetic nature.
This determines the need for a wide range of knowledge and skills of the GPs in the field of medical genetics, which will help them to early detection and diagnosis of these patients. The knowledge of medical genetics is important for today's health care practitioners because genetic diseases make up a large proportion of the total disease burden in both the paediatric and adult populations. In many cases this knowledge can lead to the actual prevention and more effective disease treatment [17]. Hereditary kidney disease comprises approximately 10% of adults and nearly all children who require renal replacement therapy. Technologic advances have improved our ability to perform genetic diagnosis and so enhanced our understanding of renal diseases [18].
In this context, a case report of 3 patients in a family is described, to illustrate the condition of hereditary kidney diseases and to reflect and deepen in the induction of the concepts of family care in general medicine. That is, it is intended that the clinical presentation allows going, from the particular of a family case, to the general family care. Clinical case reports must be seen as the first link in the chain of evidence. Although this type of research is traditionally considered to be relatively weak scientific evidence, case reports are of scientific value. A great deal of information can be conveyed in a case report that would be lost in a clinical trial or survey. In addition, the case report can be immediately understandable by clinicians; the clarity of its elements allows inducing concepts. It is about presenting a situation that may seem unusual, and yet it is a very ordinary (family care), and draw conclusions that can be applied to the generality of consultations in general medicine [19].
Clinical Observation: Study of 3 Cases
(Each case is attended by a different general practitioner)
(Each case is attended by a different general practitioner)
Case 1 (Attended by the doctor 1)
BH, is a 36-year-old woman, who had presented several episodes of isolated microscopic haematuria, with normal abdominal ultrasound, and without other analytical alterations, remaining stable and asymptomatic.
BH, is a 36-year-old woman, who had presented several episodes of isolated microscopic haematuria, with normal abdominal ultrasound, and without other analytical alterations, remaining stable and asymptomatic.
Personal history: Chronic anxious-depressive disorder with somatizations in recurrent treatment with psychotropic drugs. No diagnosis was reached
Case 2 (Attended by the Doctor 2)
SB, is 56-year-old male, worker on a crane. Personal history: Arterial Hypertension known for years, with pharmacological treatment. Cholelithiasis and cholecystectomy. He refers that in childhood had "loss of sugar in the urine" (without clear reports). Doubtful hearing loss detected a few years ago in labour examination. He was smoker of 5 or 6 cigarettes a day. No alcohol intake; no other toxic habits.
SB, is 56-year-old male, worker on a crane. Personal history: Arterial Hypertension known for years, with pharmacological treatment. Cholelithiasis and cholecystectomy. He refers that in childhood had "loss of sugar in the urine" (without clear reports). Doubtful hearing loss detected a few years ago in labour examination. He was smoker of 5 or 6 cigarettes a day. No alcohol intake; no other toxic habits.
18 years ago was detected in a routine analytical, microscopic haematuria. An abdominal ultrasound was normal. Urinalysis was repeated several years, being normal. 8 years ago in occupational medical examination an increase in Urea was detected. The patient reports that in other previous examinations this alteration was also found. Three years ago he presented urea of 62 mg/dl, creatinine of 1.2 mg/dl, K of 5.55 mEq/l, negative albumin/creatinine ratio, and urine sediment with 10-15 erythrocytes per field. Your BP is 140/90 mmHg.
Current illness: subjectively good. He is asymptomatic. Do not oedema in lower limbs. Good rhythm of diuresis. Nocturnal 1-3 times. No micturition syndrome or haematuria. No renal colic or urinary infection. Acceptable BP control, cough with the ACEI and treated with ARA II. Mild hyperkalaemia after onset of ARA II.
Evolution: the diagnosis of stage I kidney disease was made, with microhematuria and minimal proteinuria. There was stable renal function with good control of proteinuria, normal glomerular function, which presents with microhematuria and hypertension.
Main Diagnosis: Chronic Kidney Disease stage 1, possible chronic Glomerulonephritis.
Case 3 (Attended by the doctor 3)
RB, is a 32-year-old man, currently working as a delivery boy, completely asymptomatic, with the Personal Background of nocturnal enuresis until 6 years of age, acne in adolescence, hiatus hernia, some episode of swelling of the hands, which was blamed to intense manual work. Perianal eczema. Thalassemic trait in blood count. Elevated ferritin. There was some episode of violent behaviour, with alleged abuse of his ex-partner. Treatment with omeprazole.
RB, is a 32-year-old man, currently working as a delivery boy, completely asymptomatic, with the Personal Background of nocturnal enuresis until 6 years of age, acne in adolescence, hiatus hernia, some episode of swelling of the hands, which was blamed to intense manual work. Perianal eczema. Thalassemic trait in blood count. Elevated ferritin. There was some episode of violent behaviour, with alleged abuse of his ex-partner. Treatment with omeprazole.
At 22 years of age, a 1.4 mg / dl of creatinine, and proteinuria were found in a medical examination. But a new analytical was normal. Although it is recommended to repeat in a few months, it was not done.
Currently another test analytic, shows Creatinine of 1.45 mg/dl, which means a CCr calculated with formula of 63 ml/min. It was repeat a month after: Creatinine 1.4 mg/dL (calculated CCr = 78 ml/min). BP normal.
The patient says: "Same as my father and my sister". Then the family history is investigated: Chronic Renal Failure not identified in his father (SH; CASE 2) and sister (Bh; Case 1) with Benign Familial Hematuria possible. The patient does not report edema. A urinary tract infection episode 5 years ago treated with ant biotherapy. No renal colic or episodes of microscopic hematuria. Nocturia of 1-2 times.
Evolution: Patient with Renal Insufficiency already detected 10 years ago, with normal urinary sediment, and with a family history, impresses with familial interstitial nephropathy. Currently stable. The study of glomerular pathology begins.
Diagnosis: Chronic Renal Insufficiency with possible family origin
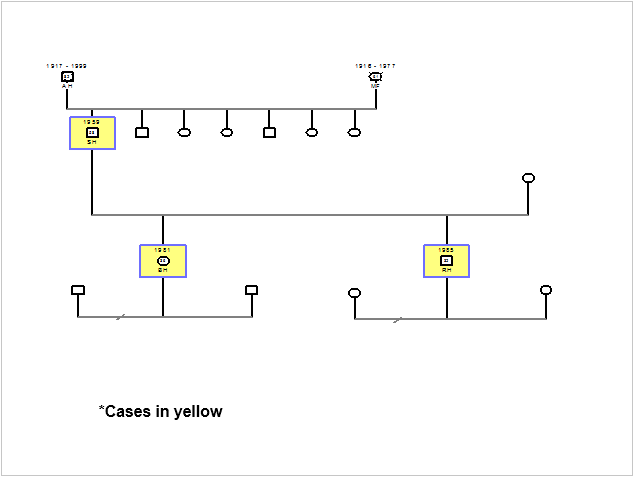
Family Approach of the 3 Cases (Figure 1)
From Case 3 (RH), CASE 1 (BH) is retaken, and a diagnosis can be made: This situation, together with the family data, points to hereditary Basal Membrane Disease.
Case 2 (SH) is re-evaluated and its diagnosis is directed towards hereditary kidney disease. It arises that the patient has 6 siblings who have not been studied for microscopic hematuria.
Discussion
Medical professionals have long known that common diseases (such as heart disease, cancer, or diabetes) and rare diseases (such as haemophilia, cystic fibrosis, or sickle cell anaemia) can be passed on from generation to generation. For example, if a family generation has high blood pressure, it would not be unusual for the next generation to have the same or something similar. Family history represents a powerful screening tool and, in general, is considered the best "genetic test". Family history should be updated at each visit and patients should know how important they are to their health.
Family history contains important information about the past and the future in a person's life. This background can be used as a diagnostic tool and contribute to decisions about genetic testing that a patient and all family members at risk must undergo. If a family is affected by an illness, it is important to reconstruct the precise family history to determine the pattern of transmission. The timely identification of a higher risk allows the patient and the medical professional to take measures to reduce the risk by implementing lifestyle changes, performing medical interventions or increasing the monitoring of the disease. While it is possible for health care professionals to be familiar with the genetic diseases that occur in childhood, it is important to note that there are also many complex genetic diseases that appear during adulthood and are hereditary [20].
There are 5 important topics in relation to hereditary diseases and especially hereditary renal diseases in general medicine:
- The family focus
- The clinical interview, communication and doctor-patient-family relationship, beliefs, psychosocial and cultural factors in hereditary diseases
- The greater clinical complexity of hereditary renal diseases in relation to their diagnosis and treatment
- The lack of knowledge or epidemiological data
- The role of the general practitioner in hereditary chronic kidney diseases
The family focus
The low frequency of a family approach in health care is striking, which leads to a low incidence of the collection of family history in the clinical history of individual patients. This fact can be observed in our case, where none of the three doctors initially collected family history. However, from the beginning of the life cycle to death, the family affects, and is affected, by the health of its members in many ways:
The low frequency of a family approach in health care is striking, which leads to a low incidence of the collection of family history in the clinical history of individual patients. This fact can be observed in our case, where none of the three doctors initially collected family history. However, from the beginning of the life cycle to death, the family affects, and is affected, by the health of its members in many ways:
- Genetic transmission
- Transmission of life habits and values
- Family events
- The social interaction
- The effects on the family of the patient and his treatment
- The effects of the health/disease in the family relationship
Why an "approach" to the family? Because an individual's problems are usually best understood when placed in the context of the family; the problems are often shared by more than one individual in the family; and the family itself can hold the key to successful solutions [1]. Consequently, the GPs must have the knowledge and skills to work with families and include the family and its context in the care process. The family group must be identified as a possible patient or client. This approach implies conceiving the family as a system in which a special, close and lasting interaction takes place between the components. Table 1 shows the different methods of family characterization and evaluation that can be carried out in the family medicine clinic. Within the Diagrams or Maps, one of the most useful is the genogram [21-23].
- Observation
- Interview
- Questionnaires
- Diagrams or maps
Table 1: Methods of Family Characterization and Evaluation.
Thus, family history can be recorded in several ways: you can create tables, checklists, forms or drawings of a family tree. Many times, the family tree or genogram is the chosen way to record the family history of a patient because drawing it is easier than writing the information and transmission patterns can be detected as the drawing is made (20). The genogram is a schematic model of the structure and processes of a family. The genogram is an instrument that allows us to easily incorporate and retrieve information about the family in which the patient is immersed, as well as to analyze and better understand that information in order to achieve a better resolution of their problems. There are several conventional signs that represent the various structures, functions, etc. (Figure 1). The genograms are formats to draw a family tree and thus have information about it quickly and clearly [23-26]. Genogram may reflect: 1) Family structure; 2) Life cycle in which that family is; 3) Important vital events; 4) Family resources; and 5) Relational family patterns [27-32].
The genogram gives rise to work hypotheses: hypotheses about patients' risks for family related illnesses or stressors, such as diabetes, hypertension, coronary heart disease, substance abuse, depression, or hereditary disease as kidney diseases; a family history of these problems often allows a GPs to generate a hypothesis about a patient's presenting complaint quickly and then develop questions that help in coming to a diagnosis and management plan [33-36]. "Family trees" that allow GPs to see hereditary family diseases. Family trees became popular among neurologists during the late 19th century. However, social scientists have devoted only scant attention to the historical and social processes through which, before the rediscovery of Mendelian laws, medical practitioners came to use family trees as scientific devices for nosographical classification of hereditary diseases [37]. In our case, if from the first patient, a family approach had been made, drawing the genogram of the family and collecting their family history, the diagnosis of hereditary kidney disease would have appeared, for the doctor, immediately.
The contributions of the genogram and its interpretation will depend on the type of clinical decision that we should take in the following three levels [20, 38, 39]:
- In prevention it can help us find out diseases, both known genetic transmission (hereditary kidney diseases, diabetes mellitus, and thalassemia), infectious transmission, and psychosocial disorders (alcoholism, depression) which have a tendency to repeat in the family. Having this in mind can facilitate prevention, early diagnosis and adjust the advice to the stage of individual or family development in which the patient or family is located.
- In the diagnosis, so we can assess how family history may be influencing your current illness and what health beliefs the patient and family may have.
- In the treatment it will guide us in those family factors that will facilitate or complicate a particular treatment and the family support that will have at the time of doing it. Table 2 exposes the signs and indicators that should alert the GPs about the need for family evaluation [40-43].
- Nonspecific symptoms in a patient who frequently visits doctor office
- Frequent visits by different members of the family
- Difficulties in the treatment of chronic diseases
- Emotional and behavioral problems
- Problems that affect two people or more
- Triangulation
- Diseases related to lifestyle and environment
- Hereditary diseases
- Preventive activities and health promotion in the family
- Anxiety caused by the anticipation of frequent problems associated with the phases of the family life cycle
- Significant losses
Table 2: Signs Indicating the Need for Family Assessment.
The clinical interview, communication and doctor-patient-family relationship, beliefs, psychosocial and cultural factors in hereditary diseases
In hereditary diseases, in addition to the significant degree of disability they generate, we must bear in mind that their social impact is enormous, because of their potentially recurrent nature in the same family and because of the high socio-sanitary cost derived from the enormous burden of care which requires [44].
In hereditary diseases, in addition to the significant degree of disability they generate, we must bear in mind that their social impact is enormous, because of their potentially recurrent nature in the same family and because of the high socio-sanitary cost derived from the enormous burden of care which requires [44].
The disease should not be taken solely as a biological disorder, but as a psychological and social perception of the individual. Necessarily, every human being has psychological characteristics that distinguish him from his peers. After deciphering these characteristics of the patient, it is useful to know how they are structured, taking into account that their personality is the result of the interactions of the individual with their environment, with factors that act since childhood, and among which we can highlight: 1) hereditary factors, where the genetic characteristics that predispose and increase the risk to certain pathologies acquire importance; 2) somatic factors, which take into account the physiological structure of the individual; and 3) experiences, especially in childhood, since they become the point of reference for evaluating later events in life, and social and cultural influence, which impose behaviour patterns and categorize what is and is not normal, or health and disease [45,46].
Patients' beliefs about symptoms are major influences on consultation and its consequences. However, little information is available about the beliefs of patients when they consult their GPs [47,48]. A fact still frequent in many places is a biased and ancestral cultural conception of the hereditary disease as "family blemish or stain", and so the tendency is to hide the disease frequently, in a vain attempt to refuse an evident reality, creating important confusions, which in many cases prevent early recognition of the affected people with the consequent damage to them. On the other hand, the family presentation of many kidney diseases is in the public domain. The popular observation, before that the modern sciences of Epidemiology and Statistics, came to establish this relationship in a scientific way, it is had already established in the knowledge of the people that many people had "stone sickness" like their predecessors, or they died of "urea", as it had happened to several members of their family. However, unlike the purely medical research done in hereditary diseases, little work has been done on the psychosocial aspects of the disease (stressful influences and the consequences of that stress on the family network) [49]. Thus, the identification and management of the physical signs and symptoms of diseases has improved, but the psychosocial burden is often not recognized and neglected [50].
In the genogram, alternatively, it could be "invented", on individually based, a system of simple signs that, to a specific general practitioner, allow him to know data that he considers that could have special importance at the time of knowing causes of health and disease in the family of his patient and to use that data for him later benefit; for example, to collect non-habitual categories such as health beliefs in that family, level of family self-esteem, relational capital of the members of that family, material resources, knowledge, coping strategies, social supports, cultural stability, religion, and genetic and constitutional factors, among others [51]. It is not uncommon for a family interview to originate spontaneously in the primary care office: the child is accompanied by the parents; the mother is accompanied by the husband and the children, etc. And, when can family interview be appropriate? The Table 3 shows these indications.
- Pregnancy in adolescence
- Family single parent
- Terminal patient
- Duel situation
- Important psycho-physical impairment of a family member
- Care of an old person
- A similar problem that affects more than one family member
- A hereditary or congenital disease
Table 3: When can a family interview be adequate?
The greater clinical complexity of hereditary diseases (and hereditary renal diseases) in relation to diagnosis and treatment
The GPs have to face these diseases that present a greater complexity of management than others, given that in hereditary pathology it must also assess, as a congenital condition, the early diagnosis, and as a fact of undoubted transcendence, both family and social, the genetic counselling.
The GPs have to face these diseases that present a greater complexity of management than others, given that in hereditary pathology it must also assess, as a congenital condition, the early diagnosis, and as a fact of undoubted transcendence, both family and social, the genetic counselling.
The diagnosis of hereditary diseases has very significant differentiating characteristics since the result of a genetic diagnosis has not only effects on the patient but also on all related individuals. Therefore, the unit of study in the genetic diagnosis is the family and every diagnostic process involves a family investigation. Another aspect that distinguishes genetic diagnosis is the ethical-social dimension. In addition, it must be taken into account that not always the conclusion obtained in the genetic diagnosis is decisive and frequently having a probabilistic component. Therefore, the results obtained and the type of information provided to the patient and his family should be qualified in this regard [44].
Hereditary nephropathy is a kidney disease that is transmitted by autosomal dominant or recessive inheritance, or linked to the X chromosome (mutations in various genes that code for podocyte proteins, mutations in genes that encode chains of collagen IV.); It can affect the glomerulus (for example, Alport syndrome, familial benign hematuria, Fabry disease, nail-patella syndrome, congenital nephrotic syndrome, etc.) or the tubule or tubulopathies (polycystic kidney disease in adults and children, nephron phthisis, Fanconi syndrome, renal glycosuria, cystinosis, renal tubular acidosis, etc.). As diseases progress, the rest of the structures are affected as glomeruli, tubules, interstitium and kidney vessels. Some of them evolve to terminal renal failure (e.g., Alport syndrome and adult polycystic kidney disease). Some authors consider that certain entities are variants of others (52-55). In any case, obtaining a thorough family history and records of affected family members is especially helpful [56].
Lack of knowledge or epidemiological data
Under the generic term of Hereditary Renal Disease a group of diseases can be grouped that have in common two characteristics: the evolution towards the Renal Insufficiency and the capacity to be transmitted from parents to children, that is to say, to be hereditary. The general absence of an epidemiological census that accurately determines the number of people affected by these diseases is striking, but it is thought that especially the Alport Syndrome represents a significant number of undetected cases [57]. A no negligible proportion of diseases in the field of nephrology are hereditary. In the last years, genetic studies have allowed identification of causative mutations in a wide variety of rare Mendelian renal disorders [58]. Despite this, its exact prevalence in the population has not been established in epidemiological studies.
Under the generic term of Hereditary Renal Disease a group of diseases can be grouped that have in common two characteristics: the evolution towards the Renal Insufficiency and the capacity to be transmitted from parents to children, that is to say, to be hereditary. The general absence of an epidemiological census that accurately determines the number of people affected by these diseases is striking, but it is thought that especially the Alport Syndrome represents a significant number of undetected cases [57]. A no negligible proportion of diseases in the field of nephrology are hereditary. In the last years, genetic studies have allowed identification of causative mutations in a wide variety of rare Mendelian renal disorders [58]. Despite this, its exact prevalence in the population has not been established in epidemiological studies.
It is admitted that about 10 to 15 percent of kidney diseases are inherited or related to genetic factors (59). The incidence of thin membrane nephropathy (thin basement membrane syndrome, benign familial haematuria) in the general population lies between 5.2% and 9.2% [60]. And up to 20% of cases of Chronic Kidney Disease (CKD) are thought to be due to genetic forms of renal disease. This approximates to population prevalence with Genetic Renal Disease (GRD) of 32,000/million aged ≥ 25 years or 3.2% of the population ≥ 25 years. Other authors have reported a population prevalence of CKD due to GRD of 138 cases per million population 18 years or over. These patients are younger with higher levels of renal function and are more likely to be female. But it is unclear however whether CKD due to various forms of GRD carries the same risks as that associated with other CKD aetiologies. This requires longitudinal studies and further clarification. The GRD spectrum is vast, encompassing many different diseases and disease groupings.
In any case, the finding of a significant and identifiable minority of patients with CKD having GRD confirms this group as a priority target for optimised future service planning within the emerging paradigm of personalised medicine and healthcare. This also allows the early identification and management of at risk family members, prior to them developing significant renal dysfunction [61], since hereditary kidney disease comprises approximately 10% of adults and nearly all children who require renal replacement therapy [18, 62].
The role of the GPs in hereditary chronic kidney diseases
GPs often meet with patients with suspected or proven hereditary diseases and predispositions, as monogenic diseases, congenital anomalies, socially significant multifactorial diseases and others. This determines the need for a wide range of knowledge and skills of GPs in the field of medical genetics, which will help them to early detection, accurate diagnosis and adequate treatment of these patients [17].
GPs often meet with patients with suspected or proven hereditary diseases and predispositions, as monogenic diseases, congenital anomalies, socially significant multifactorial diseases and others. This determines the need for a wide range of knowledge and skills of GPs in the field of medical genetics, which will help them to early detection, accurate diagnosis and adequate treatment of these patients [17].
GPs can recognize that individuals have relatives with hereditary kidney disease, and it is reasonable to use a "family history" as a surrogate marker for risk of future nephropathy [63].
The GPs play a fundamental role, since they are the first recipient of cases in the community, and in turn knows the patient's environment. In this way, you can take into account an individuals with a high risk category for a particular disease, as well as your family history or the clinical symptoms it presents to refer you to the Clinical Genetics specialist. In general medicine consultations there are multiple opportunities to detect and even prevent diseases with a hereditary component, however, in most cases it will be necessary to refer the patient or family to the specialized level to carry out the necessary tests and the application of genetic counselling. In addition to the technical and methodological components, there are many personal aspects that require you to be especially careful with the ethical aspects in the application of genetic counselling: confidentiality, right to own or third party information, legal, psychological, social or labour consequences, etc. [64].
The traditional division of individual, family and community care has nothing to do with the real GPs: they always work with individuals, families and communities, at the same time. The division of these concepts acts against working in a comprehensive manner. The Table 4 shows the information that GPs need on the family group. Only an Integrated approach with the active participation of GPs in consultation with nephrologists can successfully stem the incidence of CKD [65].
- Family profile: type of family, composition, ages, sexes, status, occupations, characteristics of the home, stage of the family life cycle, predominant relationships in the family group, values and beliefs, social and cultural orientation, network of social support, leisure, general characteristics of the community context.
- Health and diseases characteristics: pathological history, current consequences of health problems, opinion of members regarding their health problems, previous experiences of uses of services.
- Self-care, care for dependents: self-care routines, who usually performs them, how the family is mobilized in response to a need for care of one of its members.
- Resources and limitations for self-care: external material resources: economic, housing, health services available, etc., personal resources: skills, energy, knowledge, motivation, capacity, etc., family/group resources: intrafamilial communication, relationships, collaboration, social support network, etc.
In summary and conclusion
Under the generic terms of Hereditary Renal Disease or Hereditary nephropathy there are vast spectrums of many different diseases that are transmitted by autosomal dominant or recessive inheritance, or linked to the X chromosome; they have in common two characteristics: the evolution towards the Renal Insufficiency and the capacity to be transmitted from parents to children. Further, the general absence of an epidemiological census that accurately determines the number of people affected by these diseases is striking.
Family Care, as an academic discipline with a broadly structured conceptual base and its own technology, has the capacity to respond and provide solutions to bio psychosocial problems. Family Care is a tactical and strategic change in the practice of the family doctor that focuses on transferring the attention from the traditional individual framework to the group of people that make up the family. That is, move from the individual problem to that of the family, without distancing ourselves from the social context, the community, where the family group is immersed [66]. So, the problems of an individual are usually better understood when placed in the context of the family, the problems are often shared by more than one individual in the family, and the family itself can hold the key to successful solutions.
In this context of Family Care, the role of GPs about hereditary (kidney) diseases is basic in finding of a significant and identifiable minority of these patients, and allows the early identification and management of at risk family members, prior to them developing significant renal dysfunction. GPs often meet with patients with suspected or proven hereditary diseases and predispositions, as monogenic diseases, congenital anomalies, socially significant multifactorial diseases and others. This determines the need for a wide range of knowledge and skills of GPs in the field of medical genetics, which will help them to early detection, accurate diagnosis and adequate treatment of these patients.
GPs can recognize individuals have relatives with hereditary kidney disease by using a "family history" as a surrogate marker for risk of future nephropathy. Family history can be recorded in several ways: tables, checklists, forms or drawings. Obtaining a thorough family history and records of affected family members by the family tree or genogram is especially helpful to allow GPs to see hereditary family diseases and they can be use as scientific devices for nosographical classification of hereditary diseases. In hereditary diseases, in addition to the significant degree of disability they generate, we must bear in mind that their social impact is enormous, because of their potentially recurrent nature in the same family and because of the high socio-sanitary cost derived from the enormous burden of care which requires. Patients' beliefs about symptoms are especially important in hereditary diseases because cultural conception as "family blemish ", and so the tendency is to hide the disease frequently. The GPs have to face these diseases that present a greater complexity of management than others, given that in hereditary pathology it must also assess, as a congenital condition, the early diagnosis, and as a fact of undoubted transcendence, both family and social, the genetic counselling, where GPs must be especially careful with the ethical aspects.
References
- Williams PR Family problems. Oxford: Oxford University Press (1989).
- Sayers SL., et al. “Family involvement in the care of healthy medical outpatients”. Family Practice 23.3 (2006): 317-324.
- Medalie JH and Cole-Kelly K. “The Clinical Importance of Defining Family”. American Family Physician 65.7 (2002): 1277-1280.
- Medalie JH., et al. “The family in family practice: is it a reality?” The Journal of Family Practice 46.5 (1998): 390-396.
- Medalie JH., et al. “Two physician styles of focusing on the family”. The Journal of Family Practice 49.3 (2000): 209-215.
- Tarini BA., et al. “Family History Collection Practices: National Survey of Pediatric Primary Care Providers”. Clinical Pediatrics (2017).
- Driessnack M. “Who Are You From?” The Importance of Family Stories”. Journal of Family Nursing (2017).
- Stewart M., et al. “Patient-centered medicine”. Transforming the clinical method. London: SAGE Publications (1995).
- Cogswell BE and Sussman MB (Editors) Family Medicine: A new approach to health care. New York: The Haworth Press (1982).
- Christie-Seely J. Working with the family in primary care. A system approach to health and illness. New York: Praeger. (1984).
- Sloane PD and Slatt LM Curtis P (Editors) Essentials of Family Medicine. Baltimore, Maryland, USA: Williams Wilkins. (1988).
- Calman NS., et al. “Family medicine: a specialty for all ages”. Mount Sinai Journal of Medicine 79.5 (2012): 3-9.
- Turabian JL. “Cuadernos de Medicina de Familia y Comunitaria. Una introducción a los principios de Medicina de Familia”. Madrid: Díaz de Santos (1995).
- Turabian JL and Perez-Franco B. “The Family Doctors: Images and Metaphors of the Family Doctor to Learn Family Medicine”. New York. Nova Publishers (2016).
- Rolland JS. Families, illness, and disability. An integrative treatment model. New York: Basic Books (1994).
- Turabian JL and Perez Franco B. Modelos de atención centrada en el “acompañante” del paciente. La familia y el contexto: en el borde de la relación médico-paciente en medicina de familia. Saarbrücken, Deutschland/Germany: Editorial Académica Española (2015).
- Petrova-Tacheva V., et al. “Study of frequency of patients with hereditary diseases in general medical practice”. Trakia Journal of Sciences 13(Suppl. 2) (2015): 260-262.
- Mehta L and Jim B. “Hereditary Renal Diseases”. Seminars in Nephrology 374 (2017): 354-361.
- Jenicek M. “Clinical case reporting in Evidence-based Medicine”. London: Arnold (2001).
- Genetic Alliance; The New York-Mid-Atlantic Consortium for Genetic and Newborn Screening Services Cómo entender la genética: Una guía para pacientes y profesionales médicos en la región de Nueva York y el Atlántico Medio. Capítulo 3. Reconstrucción del árbol genealógico y de los antecedentes familiares. ). Washington (DC): Genetic Alliance (2009).
- Greenwald JL., et al. “The Genogram Scale as a predictor of high utilization in a family practice”. Families, Systems, & Health 16.4 (1998): 375-391.
- Jolly W., et al. “The genogram”. The Journal of Family Practice 10.2 (1980): 251-255.
- Visscher EM and Clore ER. “The genogram: a strategy for assessment”. Journal of Pediatric Health Care 6.6 (1992): 361-367.
- McLaughlin E. Laying out a pedigree. A McLaughlin Guide. Birmingham: Federation of Family History Societies. (1988).
- DeMaria R, Weeks G, Hof L. Focused Genograms: Intergenerational Assessment of Individuals, Couples and Families. Philadelphia: Brunner/Mazel. (1999).
- Magnuson S. “The Professional Genogram: Enhancing Professional Identity and Clarity”. Family Journal 8.4 (2000): 399-401.
- Marchetti-Mercer MC and Cleaver G “Genograms and Family Sculpting: An Aid to Cross-Cultural Understanding in the Training of Psychology Students in South Africa”. The Counseling Psychologist 28.1 (2000): 61-80.
- Estrada AU and Haney P. “Genograms in a Multicultural Perspective”. Journal of Family Psychotherapy 9.2 (1998): 55-62.
- Watts C and Shrader E. “How to do (or not to do)… The genogram: a new research tool to document patterns of decision-making, conflict and vulnerability within households”. Health Insurance Plan13.4 (1998): 459-464.
- De la Revilla Ahumada L. El genograma en la practica clinica.
- Báez Montiel B and Turabián Fernández JL Un genograma “Ufff y Mmmm”. AMF Joven; 1.3 (2012).
- McIlvain H., et al. “Using practice genograms to understand and describe practice configurations”. Family Medicine 30.7 (1998):490-496.
- Like RC., et al. “Reading and interpreting genograms: a systematic approach”. The Journal of Family Practice 26.4 (1988): 407-412.
- Berg A. “Genograms, Generalizability, Quantities and Qualities”. The Journal of the American Board of Family Medicine 4 (1991): 468-469.
- Erlanger M A. “Using the Genogram with the Older Client”. Journal of Mental Health Counseling 12.3 (1990): 321-331.
- Fink AH., et al. “More on genograms: Modifications to a model”. Journal of Child and Adolescent Group Therapy 3.4 (1993): 203-206.
- Nugaka Y. “The use of family trees and the notion of heredity: a case study of hereditary chorea”. Kagakushi Kenkyu 43.231 (2004): 150-560.
- Turabian JL. “Family genogram in general medicine: a soft technology that can be strong. An update”. Research in Medical & Engineering Sciences (2017).
- Bagchi S., et al. “Targeted screening of adult first-degree relatives for chronic kidney disease and its risk factors”. Nephron Clinical Practice 116.2 (2010): c128-136.
- Stewart M., et al. Patient-centered medicina. Transforming the clinical method. London: SAGE Publications; (1995).
- Gutiérrez-Islas E., et al. “Patients with adverse drug reactions have a higher prevalence of emotional disorders”. Aten Primaria 44 (2012): 720-726.
- Turabian JL and Perez Franco B. “The presence of a companion in the primary care consultation”. Semergen 41.4 (2015): 206-213.
- Turabian JL., et al. “The Patient Companion in the Consultation of Family Medical Practice is an Indicator of Hidden Family Problems”. Family Medicine Journal 1 (2016): 01.
- González-Lamuño D and García Fuentes M. “Genetically based diseases ”. Anales Sis San Navarra 31(supl.2) (2008).
- Campo-Cabal G., et al. “A therapeutic perspective of the medical interview”. Revista Colombiana de Psiquiatría 35.4 (2006).
- Turabian JL and Pérez Franco B. “The Effect of Seeing the Sea for the First Time. An Attempt at Defining the Family Medicine Law”. The Interview is Clinical Medicine 40.11 (2008): 565-566.
- Woloshynowych M., et al. “General practice patients' beliefs about their symptoms”. British Journal of General Practice 48.426 (1998): 885-889.
- Turabian Jl and Perez-Franco B. “Journey to what is essentially invisible: Pysochosocial aspects of disease”. Semergen 40.2 (2014): 65-72.
- Cleiren MP., et al. “Living with a hereditary form of cancer: experiences and needs of MEN 2 patients and their families”. Henry Ford Hospital Medical Journal 37.3-4 (1989):164-166.
- Turner J and Kelly B. “Emotional dimensions of chronic disease”. Western journal of medicine 172.2 (2000): 124-128.
- Wachtel EF. “The family psyche over three generations: the genogram revisited”. Journal of Marital and Family Therapy 8.3 (1982): 335-343.
- Kashtan CE., et al., “Alport Syndrome and Thin Basement Membrane Nephropathy”. Synonyms: Alport Syndrome and Benign Familial Hematuria, Alport Syndrome and Thin Basement Membrane Disease. Seattle (WA): University of Washington, Seattle; 1993-2017. (2015).
- Leung JC. “Inherited renal diseases”. Current Pediatric Reviews 10.2 (2014): 95-100.
- Perkoff GT. “The Hereditary Renal Diseases. The New England Journal of Medicine 277 (1967): 129-138.
- Levy NT., et al. “Hereditary interstitial nephritis without basement membrane changes”. Nephron 69.4 (1995): 418-423.
- Bleyer AJ. “Improving the recognition of hereditary interstitial kidney disease. American Society of Nephrology; 20.1 (2009): 11-13.Liébanas Cañada A., et al. “Enfermedades renales hereditarias: Estudio de las nefropatías hereditarias en la provincia de Jaén”.
- Benoit G., et al. “Hereditary kidney diseases: highlighting the importance of classical Mendelian phenotypes”. Annals of the New York Academy of Sciences 1214 (2010): 83-98.
- Zhang YQ., et al. “[Hereditary kidney diseases in children]”. Beijing Da Xue Xue Bao 45.2 (2013): 182-185.
- Dische FE., et al. “Incidence of thin membrane nephropathy: morphometric investigation of a population sample”. Journal of Clinical Pathology 43.6 (1990): 457-460.
- Mallett A., et al. “The prevalence and epidemiology of genetic renal disease amongst adults with chronic kidney disease in Australia”. Orphanet Journal of Rare Diseases 9 (2014): 98.
- Hildebrandt F. “Genetic kidney diseases”. Lancet 375.9722 (2010): 1287-1295.
- Satko SG., et al. “Familial clustering of chronic kidney disease”. Seminars in Dialysis 20.3 (2007): 229-236.
- Alonso Gordo JM., et al. “The possibilities of genetic counselling in primary healthcare”. Rev Clin Med Fam 7.2 (2014).
- Bhowmik D., et al. “Role of the family physician in controlling the epidemic of chronic kidney disease”. Journal of the Indian Medical Association 110.1 (2012): 40-42.
- Montoro R and Fernández Ruiz JS. “Family care, a necessary and relevant change strategy”. Semergen 32.5 (2006): 203-204.
Citation:
Jose Luis Turabian. “The Importance of the Family Approach in General Medicine: An Induction and Review of Concepts
from a Case of Hereditary Renal Disease”. Chronicle of Medicine and Surgery 1.1 (2017): 18-30.
Copyright: © 2017 Jose Luis Turabian. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.