Research Article
Volume 2 Issue 3 - 2018
Role of Laparoscopy in Gallbladder Perforation: Our Experience at a Medical College in Rural area of Northern India
Department of surgery, MMIMSR, Mullana, Ambala, Haryana 133207, India
*Corresponding Author: Muzzafar Zaman, Department of surgery, MMIMSR, Mullana, Ambala, Haryana 133207, India.
Received: June 14, 2018; Published: June 29, 2018
Abstract
Background: Gallbladder perforation is a rare entity and is associated with high morbidity and mortality. Early recognition and surgical treatment provides the best chance of cure.
Objectives: We will be discussing the role of laparoscopic management of gallbladder perforation in our patients in a medical college set up.
Methods: Patients diagnosed as gallbladder perforation type 1, 2 on Neimer’s classification were included in the study.
Results: 12 patients (2 males, 10 females) with an average age of 55 ± 5 years had Gall bladder perforation. Patients with Gall bladder perforation type 1, 2 were 4 and 8. All patients were subjected to surgery via laparoscopic approach with conversion to open in 2 cases. Subtotal cholecystectomy was done in 3 cases (2 laparoscopically and 1 lap to open) due to dense adhesion at calot’s triangle. Gallbladder perforation was located on the fundus in 8 cases and body in 4 cases. The average duration of stay in patients with laparoscopic surgery was 4 days while it was 7-9 days in case of open surgery. The overall mortality rate was 16% (2 cases). Complications included wound infection in 4 cases (2 laparoscopic and 2 lap to open). Pelvic abscess developed in 1 case that was managed by ultrasound guided percutaneous drainage. No recurrent cholecystitis attack was seen in patients with subtotal cholecystectomy in the 1 year follow up so far.
Conclusion: Laparoscopic surgical approach is a safe and effective modality in such patient decreasing the morbidity and is gradually becoming the gold standard approach.
Keyword: Laparoscopy; Gallbladder Perforation; Biliary Peritonitis; Acute cholecystitis
Introduction
Gall bladder stone disease is one of the commonest hepatobiliary disease encountered in any general surgical outdoor worldwide especially in fertile females who are obese and in their 4th or 5th decade of life. Apart from cholecystitis and malignancy one of the complications can be gall bladder perforation, although can be a sequel to acalcular cholecystitis patients also presenting in emergency. Gall bladder perforation is a rare entity and is associated with high morbidity and mortality. The incidence ranges from 2% to 11% [1,2]. Early recognition and surgical treatment provides the best chance of cure [3].
In the present study we will be discussing our experience in a medical college set up in a rural area of northern India about the role of minimal access surgery in the management of gallbladder perforation patients presenting to our emergency department with localised or generalised peritonitis.
Methods
This was a prospective randomised study carried out in the department of general surgery of MMIMSR mullana ambala India for a period of 2 years in a single surgical unit .A total of 12 patients who presented with clinical and radiological features of gall bladder perforation in emergency department were included in this study. These patients were selected randomly. The study was carried out after proper clearance given by the concerned ethical committee and informed consent of the patients.
Patients diagnosed as gallbladder perforation type 1, 2 on Neimer’s classification were included in the study. Patients with type 3 perforations were excluded. All the patients were admitted and detailed history and clinical examination done. All the cases were aggressively resuscitated and relevant investigations done and prepared for surgery. In all the cases, initial diagnostic laparoscopy was done through infraumblical 10mm trocar followed by adequate management done in form of subtotal or complete cholecystectomy via laparoscopy or conversion to open and peritoneal cavity was irrigated with warm normal saline till the returns were clear. Postoperatively all patients received antibiotics initially empirically then according to the culture sensitivity reports of the peritoneal fluid. No Human and Animal Rights have been violated in the present study.
Results
12 patients (2 males, 10 females) with an average age of 55 ± 5 years had Gall bladder perforation. Patients with type I and II perforations were 4 and 8 respectively. All patients were subjected to surgery via laparoscopic approach with conversion to open via Kocher’s incision in 2 cases. Subtotal cholecystectomy was done in 3 cases (2 laparoscopically and 1 lap to open) due to dense adhesion at calot’s triangle. Gallbladder perforation was located on the fundus in 8 cases and body in 4 cases. The overall mortality rate was 16% (2cases) because being sepsis leading to multiorgan failure. Complications included wound infection in 4 cases (2 laparoscopic and 2 lap to open). In the lap group port used for gallbladder extraction got infected that was managed with regular dressing. Pelvic abscess developed in 1 case (lap to open) that was managed by ultrasound guided percutaneous drainage. The average duration of stay in patients with laparoscopic surgery was 4 days while it was 7-9 days in case of open surgery No recurrent cholecystitis attack was seen in patients with subtotal cholecystectomy in the 1 year follow up so far.
Laparoscopy in gallbladder perforation: Our experience
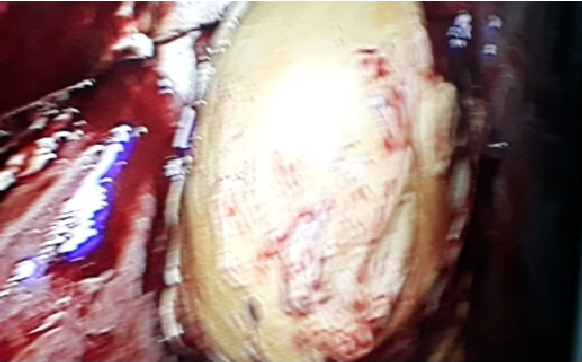
Figure 3: Showing Laparoscopic view of Gangrenous gallbladder with perforation at body with bile spillage.

Figure 4: Showing Laparoscopic to open case of Gallbladder perforation at fundus with dense adhesion at Calot's triangle. Subtotal cholecystectomy was done.
Discussion
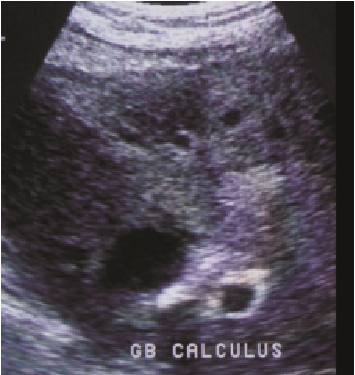
Gall Bladder Perforation is a rare but serious complication of acute cholecystitis [4]. The incidence ranges from 2% to 11% [2]. The fundus is the most common site of perforation followed by the body, and this may be due to poor blood supply in the fundus [5]. In 1934, Niemeier classified Gall bladder perforations into three types: type I (acute) that was associated with generalized biliary peritonitis; type II (subacute) that consisted of the localized collection of fluid at the site of perforation and type III (chronic) that represented the formation of internal or external fistulae [6]. Investigation aiding the diagnosis is ultrasonography and contrast enhanced computer tomography of the abdomen and same were followed in our cases also. Stood., et al. concluded that ultrasound (US) detected perforation in 61% cases and computed tomography (CT) detected it in 78% [7]. Preoperative diagnosis is challenging and many cases may be diagnosed during surgery [8]. Treatment options are an urgent laparotomy or laparoscopy.
Our study is emphasing on the laparoscopic management of gallbladder perforation. In our study total 12 cases were operated with gallbladder perforation, being more common in female patients belonging to older age group which is contrast with the other studies in which male had more gallbladder perforation [4]. The most propable reason being the geographical and socioeconomic spectra of our region in which poverty and illiteracy dominates and female patients ignore most of their early symptoms of disease and turn up to hospital when disease progresses. Our study also highlights proven fact that gallbladder perforation type 2 being more common than type 1 and gallbladder fundus perforation is more common [4]. Also in our study in 3 cases subtotal cholecystectomy was done due to dense adhesion at calots triangle with no complication in post operative period pertaining to bile leak and recurrent cholecystitis supporting the claim of proceeding with subtotal cholecystectomy in difficult calots in reducing common bile duct injuries [9]. Overall mortality rate was 16% which is comparable with our study cause being sepsis and multiorgan dysfunction because of late presentation to hospital, type 1 Gallbladder perforation highlighting the fact that early diagnosis of GBP and immediate surgical intervention is of crucial importance in decreasing mortality [4]. The limitation of our study was that the sample size was small as a result of rarity of the disease.
Conclusion
Surgery is the cornerstone of treatment for gallbladder perforation. Laparoscopic approach is a safe and effective modality in such patient decreasing the morbidity and is slowly becoming the gold standard approach. Subtotal cholecystectomy is at par with total cholecystectomy in terms of recovery and reccurance of cholecystitis with advantage of decreasing the common bile duct injuries.
Surgery is the cornerstone of treatment for gallbladder perforation. Laparoscopic approach is a safe and effective modality in such patient decreasing the morbidity and is slowly becoming the gold standard approach. Subtotal cholecystectomy is at par with total cholecystectomy in terms of recovery and reccurance of cholecystitis with advantage of decreasing the common bile duct injuries.
Conflict of interest: The authors have no conflict of interest to be disclosed.
Funding: None
Acknowledgement: None
References
- Dikshit V., et al. “Conservative management of type 2 gallbladder perforation in a child”. World Journal of Clinical Cases 3.7 (2015): 671.
- Derici H., et al. “Diagnosis and treatment of gallbladder perforation”. World Journal of Gastroenterology 12 (2006): 7832-7836.
- Alvi AR., et al. “Acute free perforation of gall bladder encountered at initial presentation in a 51 years old man: a case report”. Cases Journal 2 (2009): 166.
- Sahbaz NA., et al. “Single center experience in laparoscopic treatment of gallbladder perforation”. Wideochir Inne Tech Maloinwazyjne 12.4 (2017): 372-377.
- Wuji., et al. “Role of laparoscopic subtotal cholecystectomy in treatment of complicated cholecystitis”. Hepatobiliary & Pancreatic Diseases International5.4 (2006): 584-89.
- Gunasekaran G., et al. “Gallbladder perforation: a single center experience of 32 cases”. Korean Journal of Hepato-Biliary-Pancreatic Surgery 19.1 (2015): 6-10.
- Sood BP., et al. “Role of sonography in the diagnosis of gallbladder perforation”. Journal of Clinical Ultrasound 30.5 (2002): 270-274.
- Teefey SA and Wechter DG. “Sonographic evaluation of pericholecystic abscess with intrahepatic extension”. Journal of Ultrasound in Medicine 6 (1987): 659-662.
- Ong CL., et al. “Acute gall bladder perforation–a dilemma in early diagnosis”. Gut 32 (1991): 956-958.
Citation:
Muzzafar Zaman., et al. “Role of Laparoscopy in Gallbladder Perforation: Our Experience at a Medical College in Rural area of
Northern India”. Chronicle of Medicine and Surgery 2.3 (2018): 157-161.
Copyright: © 2018 Muzzafar Zaman., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.