Research Article
Volume 2 Issue 4 - 2018
Body Weight Perception among Adults Attending a Primary Care Clinic in South-South Nigeria
1Department of Family Medicine, University of Calabar Teaching Hospital Calabar
2Department of Family Medicine, Faculty of Medicine, University of Calabar, Calabar
2Department of Family Medicine, Faculty of Medicine, University of Calabar, Calabar
*Corresponding Author: Chibuike McSteve Okeke, Department of Family Medicine, University of Calabar Teaching Hospital, Calabar
Nigeria.
Received: May 25, 2018; Published: July 05, 2018
Abstract
Background: Body weight perception is an important determinant of weight-related behaviour especially in populations, where appearance determines who is rated as healthy, and affluent, beautiful or even fertile among the females. Recognition of misperception of weight is a precursor to a positive lifestyle change.
Aim: To determine the weight perception of study participants in relation to their actual weights in order to inform weight management intervention.
Setting: The study was done at General Out-patient Clinic (GOPC), Family Medicine Department of University of Calabar Teaching Hospital (UCTH), Calabar, Nigeria.
Methods: This was a cross-sectional analytic study among 377 participants who are 18 years and above. The sample size was calculated with Leslie Kish formula and systematic random sampling method was used in subject recruitment.
An interviewer-administered questionnaire was used to gather data on the socio-demographic and body weight perceptions. Weights and heights were measured to determine Body Mass Index (BMI) as a measure of subjects’ actual weight statuses. Correct and incorrect weight perceptions are when perceptions matched and unmatched with the actual weight respectively. The data were analyzed with SPSS.
Results: The subjects were mostly between the ages of 21-40 years (75.6%), Female (62.9%) and married (46.6%), while 40.8% were single. Participants who had incorrect and correct weight perceptions were 217 (57.56%) and 160 (42.44%) respectively. There were statistically significant relationships between weight perception and education (χ2 = 20.20; p = 0.002), age (χ2 = 14.14, 0.007) and marital status (χ2 = 20.68, p = 0.000).
Conclusion: There is a significant level of incorrect weight perception in the study population with many having abnormal actual weights.
Keyword: Perceptions; Obesity; Overweight; Behaviour
Abbreviations: GOPC: General Out-patient Clinic; UCTH: University of Calabar Teaching Hospital; BMI: Body Mass Index; SPSS: Statistical Package for Social Sciences; REC: Research and Ethic Committee;
Introduction
Abnormal body weight poses a great problem which is compounded when individuals who are underweight, normal, overweight or obese perceive themselves to be otherwise [1-3]. The disconnect between actual body weight and perception of body size could stem from the extent to which individuals identify with the major social and cultural standards of beauty [4-6]. Individuals may be desirous of weight gain or weight loss in order to conform to acceptable social norm. Consequently body weight perception is known to be influenced by several external factors such as cultural norm, social preferences, food habits and environment, nutritional knowledge, expectant mass media depiction of what constitutes an ideal figure in addition to lifestyle differences that affects physical activities [4]. Other factors that influence body weight perception include sex, income and education levels [2]. For instance in India, it is often believed that an overweight person is wealthier and happier and reflects social mobility to a higher status than an underweight person [4,6]. In Nigeria obesity is culturally and socially acceptable and therefore not normally recognized as a medical problem [7] rather it is thought to be associated with beauty and fertility among the females; and a sign of affluence and riches among the both sexes. This is more so among some cultures in South-South and South-East of Nigeria where obesity and corpulence is promoted especially among women practices as the ‘fattening room’ or ‘Nkoho’ practices as marriage rites. This is the reverse in some western cultures where the obese shape is widely recognized as unattractive [4,6,8,9].
Interestingly, the disparity between objective measures of body size (like BMI) and individual perception of current body size is worrisome. This suggests societal or individuals’ definitions of desirable body size that are not based on medical facts. Consequently, the implication of excessive body weight or underweight is not readily apparent due to lack of emphasis on non-communicable diseases in traditional health education and counselling at the community level. These can lead to unhealthy eating and other health habits which may result in inappropriate weight in the form of obesity, underweight or outright malnutrition.
Critical to the adoption of weight management recommendation is the motivation to lose weight or knowledge that the current weight is inappropriate. [10] Without this understanding, there will be difficulty in promoting appropriate weight management resulting to co-morbidities with increasing morbidity and mortality.
The aim of this research was to determine the body weight perception and social desirability for obesity among patents attending the General Outpatient Clinic (GOPC) of University of Calabar Teaching Hospital (UCTH) in order to form a baseline upon which weight management intervention can be designed.
Materials and Methods
This was a cross-sectional analytic study carried out at the GOPC of the University of Calabar Teaching Hospital (UCTH) from March 2016 to June 2016. The UCTH is the largest health facility in Cross River State and caters for health needs of people in and around the state. It receives referral from Akwa Ibom State, Abia State, Rivers, Benue State, part of southern Cameroun amongst others. Cross River State is known for its tourism.
In GOPC, an average of 80 patients are seen daily excluding weekends, hence 400 were seen weekly and 1200 were seen within the duration of the study. The sampling interval of 4 was used, while the first participant was selected blindly by simple random sampling. The sampling continued on each clinic day until the required sample size of 377 was achieved. Included in the study were participants 18 years and above who gave an informed written consents and excluded from the study were pregnant women because of the pregnancy changes, and patients who required urgent care were also excluded. Ethical approval was sought and obtained from Research and Ethic Committee (REC) of UCTH, Calabar.
A structured questionnaire was used for this study after it was pre-tested among 50 adult patients in the neighbouring General Hospital, Calabar which has similar study population. The results showed that the tool could be used to determine our study objectives. The questionnaire was divided into three sections; section A assessed the socio-demographic characteristics of the respondents in the study including age, gender, marital status, occupation, level of education and tribe; Section B of the questionnaire assessed weight perception, where participants were asked to select among underweight, normal, overweight and obesity in line with perception of their weights, while Section C of the questionnaire was used to record the anthropometric measurements of the participants which include weights and heights. Body mass index (BMI) was calculated as weight in kilograms divided by the square of the height in meters and these were grouped according to the WHO criteria for obesity. Participants with BMI of 30 kg/m2 and above were regarded as obese while those with BMI ≥ 25.0 to ≤ 29.9 were regarded as overweight, normal weights were BMI of 18.5–24.9, while < 18.5 was considered as underweight. Correct and incorrect weight perceptions are assessed when perceptions matched and unmatched with the actual weights respectively.
Data generated were entered and analyzed using the Statistical Package for Social Sciences (SPSS) Version 20.0. Analysis was done using mainly descriptive statistics. Frequency, proportion, mean, and standard deviation were calculated for relevant variables. Chi-square tests and Fisher’s exact were used to determine the significant association between two categorical variables. P-value was set at < 0.05 or 5%.
Results
The study participants perceived weights and the actual (BMI) weights were shown in Table 1 below. Majority perceived that their weights was normal (74.3%), while the normal weight of the same population using BMI was only found in 48.3%.
| Weight Perception | Frequency n = 377 | Percentage (%) |
| Under weight | 52 | 13.8 |
| Normal | 280 | 74.3 |
| Overweight | 39 | 10.3 |
| Obese 30–34.5 | 6 | 1.6 |
| Body Mass Index | ||
| Underweight | 24 | 6.4 |
| Normal | 182 | 48.3 |
| Overweight | 95 | 25.2 |
| Obese 30–34.5 | 56 | 14.9 |
| Morbid Obesity 35–39.9 | 19 | 5.0 |
| Super Obesity > 40 | 1 | 0.2 |
Table 1: Weight perceptions and body mass index of study participants.
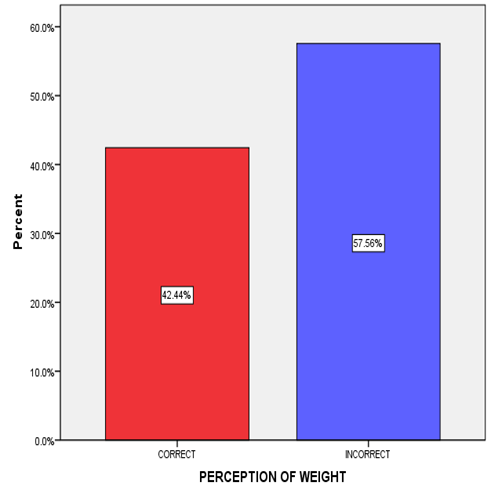
The cumulative weight perception of study participants was shown in (figure 1). Two hundred and seventeen participants (57.56%) had wrong perception of their body weight while one hundred and sixty (42.44%) had correct perception of their body weight.
The socio-demographic characteristics of the study participants as presented in (Table 2), showed that the age group most represented in the study was 20-30 years followed by those aged 31-40 years (43.0% and 32.6% respectively). Females were more than males in the study, A little above two-fifth of participants were either married or single. Majority were public servants (37.9%) followed by students (27.6%) and Trading (18.0%). A little above 60% of the subjects had tertiary education whereas about 40% had at most secondary education.
| Weight perception | Total | χ2 | p-value | ||
| Correct | Incorrect | ||||
| Age group | 14.14 | 0.007 | |||
| ≤ 20-30 | 84 (52.5%) | 78 (35.9%) | 162 (43.0%) | ||
| 31-40 | 42 (26.3%) | 81 (37.3%) | 123 (32.6%) | ||
| 41-50 | 25 (15.6%) | 31 (14.3%) | 56 (14.9%) | ||
| ≥ 51 | 9 (5.6%) | 27 (12.5%) | 36 (9.5%) | ||
| Tribe | |||||
| Qua | 40 (25.0%) | 51 (23.5%) | 91 (24.1%) | 5.75 | 0.22 |
| Efut | 24 (15.0%) | 54 (24.9%) | 78 (20.7%) | ||
| Ibibio | 34 (21.3%) | 38 (17.5%) | 72 (19.1%) | ||
| Annang | 37 (23.1%) | 46 (21.2%) | 83 (22.0%) | ||
| Others* | 25 (15.6%) | 28 (12.9%) | 53 (14.1%) | ||
| Marital status | |||||
| Single | 86 (53.8%) | 68 (31.3%) | 154 (40.8%) | 20.68 | 0.000 |
| Married | 61 (38.1%) | 114 (52.5%) | 175 (46.4%) | ||
| Separated | 13 (8.1%) | 35 (15.2%) | 48 (12.8%) | ||
| Occupation | |||||
| Not working | 11 (6.9%) | 22 (10.1%) | 33 (8.8%) | 12.4 | 0.067 |
| Schooling | 52 (32.5%) | 52 (24.0%) | 104(27.6%) | ||
| Public servant | 66 (41.3%) | 77 (35.5%) | 143(37.9%) | ||
| Trading | 20 (12.5%) | 48 (22.1%) | 68 (18.0%) | ||
| Others** | 11 (6.8%) | 18 (8.4%) | 19 (7.7%) | ||
| Sex | |||||
| Male | 55 (34.4%) | 85 (39.2%) | 140 (37.1%) | FET | 0.084 |
| Female | 105 (65.6%) | 132 (60.8%) | 237 (62.9%) | ||
| Educational status | |||||
| ≤ Secondary | 57 (35.6%) | 93 (42.9%) | 150 (39.8%) | 20.2 | 0.002 |
| ≥ Tertiary | 103 (64.4%) | 124 (57.1%) | 227 (60.2%) |
Table 2: Relationship between weight perception and some socio-demographic characteristics of study respondents.
Other* - Foreigners; χ2 – Chi square; FET- Fishers’ exact test
Other** - Traders, Farmers and Artisan; Separated – includes divorced and widowed
Other* - Foreigners; χ2 – Chi square; FET- Fishers’ exact test
Other** - Traders, Farmers and Artisan; Separated – includes divorced and widowed
The relationship between the pattern of perceived body weight and some socio-demographic characteristics of study participants is presented on (Table 2), illustrated that there was a statistically significant relationship between perceived body weight and age group (χ2 = 14.14, p = 0.007) marital status: (χ2 = 20.68, p = 0.000) and educational status (χ2 = 20.2, p = 0.002).
Discussions
Individuals’ body weight perception is a strong determinant of body weight control activities [1,11]. This study set out to determine the self-perception of weight by study participants who were clinic attendees of the GOPC, Calabar. It was noted that there were more female clinic attendees than male attendees. This follows a pattern noted that females have better health seeking behaviour than males [12,13]. Civil servants were more than other occupation groups and this is so noted because the study setting is in Cross River state, which is predominantly populated by civil servants as the middle class [14]. The predominant religion in the study environment is Christianity as reflected in the study. This is similar to findings of two researches done in same region by Ezedinachi et al and Erah et al that found 99.1% and 91.2% respectively as Christians [15,16].
This study found the prevalence of overweight to be 25.2% and obesity 20.1% including varying grades of obesity based on the WHO classification of BMI (table 1). This fell within the range of what was obtained in previous study in Nigeria where the prevalence was puts at 20.3-35.1% for overweight and 8.1-22.2% for obesity [3]. In Ghana a national prevalence of overweight and obesity has been placed at 25.4% and 17.1% respectively [17,18]. The prevalence of obesity in both countries and in the present study suggest a rising prevalence of obesity based on the West African prevalence which was put at 10.0% in a meta-analysis of West African studies by Abubakar., et al. [19]. This shows the increasing prevalence of obesity in many parts of the world including the West African sub-region. Many sub-Urban African cultures do not consider obesity as a problem; instead obesity and corpulence are widely viewed as a sign of good living and index of affluence, and in women an index of beauty and fertility [8,18]. This cultural view puts additional pressure on the females to desire to gain weight in an attempt to attract the males and therefore better chance of marriage which is also very important [8]. The acceptance of female corpulence especially among the people of South East and South-South Nigeria is expressed in the “fattening room” practice in which young women go through prior to marriage to make them more sexually attractive to their husband and also to learn the basic home keeping [20,21]. Other reason obesity is prevalent in the study environment may be increase in number and usage of fast food as a means of quick meals especially as the study took place in the urban centre where fast food outlets are found in abundance.
Concerning weight perception, 280 (74.3%) of the study participants perceived their weight as normal while only 48.3% had normal weights based on the calculated BMI. It was therefore obvious that there is a discrepancy between self-perceived body weight and actual weight with overall 211 (57.56%) misperceiving their body weight. Specifically, it was noticed that a good number of those who perceived their weight to be normal were either overweight or obese. This finding was similar to what was obtained among rural dwellers in Nigeria by Akinpelu., et al. where 54% of the participants misperceived their weight. [22] Wrong perception of one’s actual body size and having a personal preference for an ideal body size that is larger than the actual might reduce a person’s motivation to engage in body weight management practices that will help in maintaining healthy weight. Misperception of body weight may even be more dangerous among Underweight individuals who wrongly perceive themselves to be overweight or obese as they may try weight control measures which may lead to further loss of weight and predisposition to various health problems related to their underweight. On the other hand, perceiving oneself as normal when overweight/obese may limit their attempts at weight control leading the complications of obesity.
The study found that socio-demographic factors of an individual like education, marital status and age significantly (p < 0.05) affected their body weight perception. This is to be expected since education will enlighten the individual about appropriate weight through reading and exposure to other educational materials. On the centrally a study carried out in Korea showed that the higher the level of education the more likely an individual will misperceive his/her weight [23]. This may stem from overconfidence or wrong understanding of certain facts. Marriage on the other hand does influence weight perception through the tendency to please the marriage partner, while age through value changes and understanding of what is best or appropriate.
While factors like sex, occupation and the tribe they come from did not significantly (p > 0.05) affect how they perceived their body weight. This is contrarily to the Korean study in which it was documented that females more commonly misperceive their weight than males, even though this was not stated to be a statistically significant association [23]. This difference may be due to the difference in population and also the composition of the sample.
Because body weight perceptions held by people has important health implications on weight management behaviours, it is important that clinicians gain understanding of these perceptions. This will form the basis for providing patient-specific counselling to patients based on their perceptions and healthy weight-related behaviours. The limitations of the study are that participants are likely to give false weight perception.
Conclusions
The findings of this study can be used as a basis for promoting interventions on accurate weight understanding which will influence weight perception and consequently self-weight management practices. This will ultimately influence body size and obesity and its attendant co-morbidities.
Acknowledgement
The authors appreciated the effort of Miss P. Archibong who typed the questionnaires. The statistician’s advice from Mrs Kelechi C. Okeke was also well appreciated.
The authors appreciated the effort of Miss P. Archibong who typed the questionnaires. The statistician’s advice from Mrs Kelechi C. Okeke was also well appreciated.
References
- Dorosty AR., et al. “Perception of weight and health status among women working at health centres of Tehran”. Journal of Health, Population and Nutrition 32.1 (2014): 58-67.
- Okeke EC., et al. “Body weight perception among Igbo people in the University of Nigeria, Nsukka”. Journal of tropical agriculture, food, environment and extension 5.2 (2006): 17-24.
- Chukwuonye II., et al. “Prevalence of overweight and obesity in adult Nigerians – a systematic review”. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy 6 (2013): 43-47.
- Swaminathan S., et al. “Associations between body weight perception and weight control behaviour in South Indian children: a cross-sectional study”. BMJ Open 3.3 (2013): e002239.
- Tchicaya A., et al. “Relationship between self-reported weight change, educational status, and health-related quality of life in patients with diabetes in Luxembourg”. Health and Quality of Life Outcomes 13.1 (2015): 149
- WHO. Obesity: preventing and managing the global epidemic: a report of a WHO consultation Geneva Switzerland (2000).
- Uche G., et al. “Prevalence and family biosocial predictors of abdominal obesity among adult Nigerian Africans in a resource constrained setting of a rural hospital in Eastern Nigeria”. European Journal of Preventive Medicine 1.3 (2013): 70-78.
- Okop KJ., et al. “Perceptions of body size, obesity threat and the willingness to lose weight among black South African adults: a qualitative study”. BMC Public Health 16.1 (2016): 365.
- Al-otaibi HH., et al. “Body Shape Dissatisfaction, Weight Status and Physical Activity among a Sample University Students in Saudi Arabia”. Food and Nutrition Sciences 4 (2013): 616-625.
- Mogre V., et al. “Distorted self-perceived weight status and underestimation of weight status in diabetes mellitus type 2 patients”. PLoS One 9.4 (2014): e95165.
- Mogre V., et al. “Misperception of weight status and associated factors among undergraduate students”. Obesity Research & Clinical Practice 9.5 (2015): 466-474.
- Kayima J., et al.“Hypertension awareness, treatment and control in Africa: a systematic review”. BMC Cardiovascular Disorders 13.1 (2013): 54.
- Adat PE., et al. “Assessment of Hypertensive Patients’ Illness Experience Using Patient-centred Consultation among Patients Seen in an Urban Family-practice setting in Nigeria”. Journal of Community Health Nursing 5.1 (2017): 1-10.
- National Population Commission. Population Distribution by Sex, State, LGA & Senatorial District. (2010).
- Ezedinachi E., et al. “Factors Affecting the Uptake of Anti-Malarial Drugs by Children in Public Primary Health Facilities in Cross River State, Nigeria”. Open Journal of Epidemiology 5 (2012): 21-26.
- Erah P and Arute J. “Adherence of HIV/AIDS patients to antiretroviral therapy in a tertiary health facility in Benin City”. African Journal of Pharmacy and Pharmacology 2.7 (2008): 145-152.
- Commodore-mensah Y., et al. “Hypertension and overweight/obesity in Ghanaians and Nigerians living in West Africa and industrialized countries: A systematic review”. Journal of Hypertension 32.1 (2014).
- Ofori-asenso R., et al. “Overweight and obesity epidemic in Ghana - a systematic review and meta-analysis”. BMC Public Health 16 (2016): 1239.
- Abubakari A., et al. “Prevalence and time trends in obesity among adult West African populations: a meta-analysis”. Obesity Reviews 9.4 (2008): 297-311.
- Uche G., et al. “Predictors of Abdominal Obesity among Adult Nigerians in a Resource-poor Environment of a Rural Hospital in Eastern Nigeria”. British Journal of Medicine and Medical Research 4.12 (2014): 2369-2382.
- Iloh GU., et al. “Abdominal Obesity in Adult Nigerian Africans: Prevalence and Co-Occurrence with Cardio-Metabolic Risk Factors in a Resource Poor Setting of a Rural Hospital in Eastern Nigeria”. American Journal of Health Research 1.3 (2013): 70-78.
- Akinpelu A., et al. “Body size perceptions and weight status of adults in a Nigerian rural community”. Annals of Medical and Health Science Research 5.5 (2015): 358-364.
- Kim S and So WY. “Prevalence and sociodemographic trends of weight misperception in Korean adolescents”. BMC Public Health 14.1 (2014): 452.
Citation:
Chibuike McSteve Okeke., et al. “Body Weight Perception among Adults Attending a Primary Care Clinic in South-South Nigeria”.
Chronicle of Medicine and Surgery 2.4 (2018): 182-189.
Copyright: © 2018 Chibuike McSteve Okeke., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.