Mini Review
Volume 2 Issue 5 - 2018
Ghanem’s new discoveries in Medicine, Physiology, Urology and Nephrology?
Consultant Urological Surgeon, No 1, Jasmine Tower, President Mubarak Street, Mansoura 35511, Egypt
*Corresponding Author: Ahmed N Ghanem, Consultant Urological Surgeon, No 1, Jasmine Tower, President Mubarak Street, Mansoura 35511, Egypt.
Received: June 15, 2018; Published: August 24, 2018
The last 32 years of my career life were spent in investigating and reporting these articles. [1-4] The articles recognises 2 new types of socks and its treatment, proves that Starling’s law for the capillary interstitial fluid transfer is wrong and provides an alternative mechanism; the hydrodynamics of a porous orifice (G) Tube. These discoveries resolve the puzzle of 3 clinical syndromes discovering its patho-etiology and new successful treatment; namely the transurethral resection of the prostate (TURP) syndrome and acute dilution hyponatraemia, the adult respiratory distress syndrome (ARDS) and the loin pain haematuria syndrome (LPHS). The two new types of vascular shocks are volumetric overload shocks defined here.
Volumetric Overload Shock (VOS) is a condition caused by massive fluid infusions in a short time and is of two types; Type one (VOS1) and Type two (VOS2). VOS1 is induced by sodium-free fluid gain of 3.5-5 litres in one hour such as Glycine, Glucose, Mannitol and Sorbitol. It is known as the TURP syndrome [5] or hyponatraemic shock. VOS2 is induced by massive infusion of sodium-based fluids such as normal saline, Ringer, Hartmann, plasma and plasma substitutes that may complicate the therapy of VOS1. VOS2 also complicates fluid therapy in critically ill patients suffering from other known shocks such as hypovolaemic, haemorrhagic and septicaemic shocks and presents with the adult acute respiratory distress syndrome (ARDS) [6]. VOS2 is induced by the gain of 12-14 litres of sodium-based fluids when reported in ARDS. The occurrence of massive interstitial tissue oedema with congestion of vital organs, pleural and peritoneal effusions, in the presence of hypotension shock, casted doubt on Starling’s law! These issues were investigated at the clinical and physiological/physical fronts.
Two clinical studies aiming to understand the TURP syndrome and recognising VOS were done. A prospective clinical study on 100 consecutive TURP patients of whom the condition of TURP syndrome affected 10 patients with severe hypotension and bradycardia and severe acute dilution hyponatraemia of < 120 mmol/l. Volumetric overload was the only significant factor in causing the condition. The second clinical study involved a case series of 23 cases of the TURP syndrome manifesting as VOS1. The first 3 cases died as they were diagnosed and treated erroneously as one of the recognised shocks and treated with further volume expansion. The remaining 20 patients were correctly diagnosed as VOS and treated with hypertonic 5% sodium chloride or 8.4% Sodium Bicarbonate. Each patient passed 4-5 litres of urine followed by recovery from shock and coma. This treatment was successful in curing all patients bringing them back from dead.
The physical investigation involved studies of the hydrodynamics of the porous orifice (G) tube comparing it to that of Poiseuille’s tube. Thousands of experimental measurements of pressures at various parts of a circulatory system incorporating the G tube in a chamber to mimic the capillary-interstitial fluid compartment. The effect of changing the proximal (arterial), the distal (venous) pressures and the diameter of the inlet on side pressure of the G tube and chamber pressure as well as the dynamic magnetic field like fluid circulation around the G tube. It is quite remarkable how this circulatory model mimic the circulatory system in heath and disease. This dynamic magnetic field like fluid circulation around the G tube and surrounding chamber provide adequate replacement for Starling’s law. The physiological equivalent of this physical study was done on the hind limbs of sheep. It demonstrated that arterial pressure causes suction not filtration due to the effect of pre- capillary sphincter. Venous pressure augmented filtration and oedema formation.
Shock is a disturbance at the capillary cellular level impairing the capillary-interstitial fluid transfer; hindering delivery of oxygen and removal of waste products. The process is governed by Starling’s law [7]. In this law the arterial pressure is considered the force causing capillary filtration! If this is true, how come that arterial hypertension though common never causes oedema? Starling based his hypothesis on Poiseuille work on strait uniform brass tubes. Latter evidence however demonstrated that the capillary is a porous narrow orifice (G) tube as it has a pre-capillary sphincter [8] and pores that allow the passage of plasma proteins. [9] As the capillary pores allow the passage of plasma molecules, nullifying the osmotic pressure of plasma proteins i.e. oncotic pressure does not exist, a call for reconsideration of Starling’s hypothesis was previously made but there was no alternative at that time [10]. This replacement came to light when the hydrodynamics of the G tube were discovered.
The hydrodynamics of the G tube [1,11] (Figure 1) demonstrated that the proximal (arterial) pressure induces a negative side pressure gradient on the wall of the G tube causing suction most prominent over the proximal half and turns into positive pressure over the distal half. Incorporating the G tube in a chamber (C), representing the interstitial space surrounding a capillary, demonstrated a rapid dynamic magnetic field-like fluid circulation between the C and G tube lumen. This is a mixing engine between C and G effecting rapid irrigation under negative pressure i.e. without flooding or oedema. Incorporating the G tube and C in a circulatory model driven by electric pump inducing proximal pressure similar to arterial pressure; causing suction from C into the lumen of G tube. The distal (venous) pressure augments filtration. This proves that the arterial pressure causes suction not filtration at the capillary interstitial fluid circulation, and hence Starling’s law is wrong. The reported hydrodynamics of the G tube provide an adequate mechanism for the capillary interstitial fluid circulation. This illustrates how 2 new types of vascular shocks and a replacement of Starling’s law were discovered.
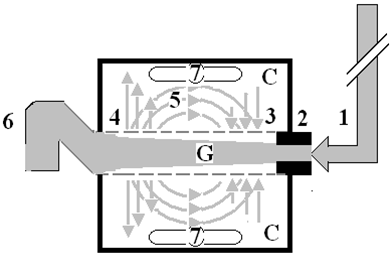
Figure 1: Shows Diagram of the porous orifice (G) tube enclosed in chamber (C) based on several photographs demonstrating the magnetic field-like G-C circulation phenomenon. The proximal inflow (arterial) pressure (1) pushes fluid through the orifice (2) creating fluid jet in the lumen of the G tube. The fluid jet creates negative side pressure gradient causing suction maximal over the proximal half of the G tube near the inlet (3) that sucks fluid into lumen. The side pressure gradient turns positive pushing fluid out of lumen over the distal half maximally near the outlet (4). Thus the fluid around G tube inside C moves in magnetic field-like fluid circulation (5) taking an opposite direction to lumen flow of G. tube.
The inflow (arterial) pressure (1) and orifice (2) induce the negative side pressure energy creating the dynamic G-C circulation phenomenon that is rapid, autonomous and efficient in moving fluid out from the G tube lumen at (4), irrigating C at (5), then sucking it back again at (3), maintaining net negative energy pressure (7) inside C. The distal outflow (venous) pressure (6) enhances outflow at (4) and its elevation may turn the negative energy pressure (7) inside C into positive, increasing volume and pressure inside C chamber.
On another subject, this article [12] reports the overlooked link of Loin Pain Hematuria Syndrome Complicating Symptomatic Nephroptosis and the Results of a new curative surgery;Renal Sympathetic Denervation and Nephropexy Surgery. Two new signs namely; the IVU 7 sign (Figure 2) and tube stretch hypothesis were reported demonstrating that renal pedicle stretch causing ischaemia and neuropathy.This was based on a prospective study of 190 patients with symptomatic nephroptosis (SN) shown on erect IVU-E film, 182 were females and 8 males. The mean age was 28.8, duration of symptoms 15.7 and hospital follow up 6.6 years.
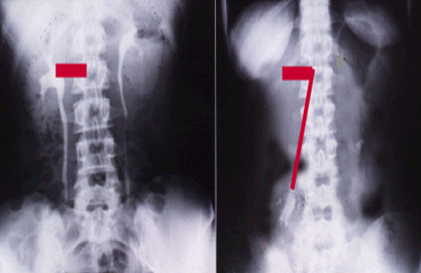
Figure 2: Shows renal pedicle mapped on a supine IVU film (Horizontal) and erect film (Vertical) limbs of 7 where the renal pedicle is stretched to 3 times its normal length, causing stenosis and ischemia.
Patients showed no abnormality on IVU or ancillary imaging when supine. All patients showed renal drop of > 1.5 vertebrae (> 5 cm) on erect IVU film. Other demonstrable pathology on erect IVP film included: pelviuretric junction kink affecting the right kidney in 116 (61.1%) and bilateral in 19 (10%) of patients. Stretch/rotation of renal pedicle causing neuro-ischaemic pain of LPHS was demonstrable on the right side in 72 (37.9%) and bilaterally in 7 patients.
Complications of SN on IVU-E film included both obstructive and neuro-ischaemic: obstructive complication included ballooned renal pelvis, hydronephrosis and upper pole diverticulum. Neuro-ischaemic complications induced by pedicle stretch and rotation/twist were haematuria of the LPHS affecting 36 (18.9%), auto nephropexy affecting 12 right kidneys, upper pole calyctiasis with extra-vasation affecting 28 (15.8%) right kidney and 2 bilateral that are best shown on RGP. Renal atrophy affected 4 right kidneys. Upper pole infarction affected 2 right kidneys. Retrograde pyelography (RGP) also demonstrated upper pole calyctiasis with extra-vasation. Surgical treatment was used in 28 patients; 10 had simple nephropexy and 18 had Renal Sympathetic Denervation and Nephropexy Surgery (RSD&N) for severe LPHS. Four of patients treated with simple nephropexy had recurrence of LPHS while those who had RSD&N were all cured.
References
- Ghanem AN and Ghanem SA. “Volumetric Overload Shocks: Why Is Starling’s Law for Capillary Interstitial Fluid Transfer Wrong? The Hydrodynamics of a Porous Orifice Tube as Alternative”. Surgical Science 7 (2016): 245-249.
- Pindoria N., et al. “Volumetric overload shocks in the patho-etiology of the transurethral resection prostatectomy syndrome and acute dilution hyponatraemia”. Integrative Molecular Medicine (2017).
- Ghanem KA and Ghanem AN. “The proof and reasons that Starling’s law for the capillary-interstitial fluid transfer is wrong, advancing the hydrodynamics of a porous orifice (G) tube as the real mechanism”. Blood, Heart and Circulation 1.7 (2017): 1-7
- Ghanem KA and Ghanem AN. “Volumetric overload shocks in the patho-etiology of the transurethral resection prostatectomy syndrome and acute dilution hyponatraemia: The clinical evidence based on 23 case series”. Basic Research Journal of Medicine and Clinical Sciences 6.4.
- Ghanem AN and Ward JP. “Osmotic and metabolic sequelae of volumetric overload in relation to the TURP syndrome.” British Journal of Urology 66 (1990): 71-78.
- Ashbaugh DG., et al. “Acute respiratory distress in adults”. Lancet 2(7511) (1967): 319-323.
- Starling EH. “Factors involved in the causation of dropsy”. Lancet (1886): 1330-1334.
- Rhodin JA. “The ultra-structure of mammalian arterioles and precapillary sphincters”. J Ultrastructure Research 18 (1967): 181-222.
- Karnovesky MJ. “The ultra-structural basis of capillary permeability studied with peroxidase as a tracer”. The Journal of Cell Biology 35 (1967): 213-236.
- Renkin EM. “Some consequences of capillary permeability to macromolecules: Starling’s hypothesis reconsidered”. American Journal of Physiology 250.19 (1986): H706–H710.
- Ghanem AN. “Magnetic field-like fluid circulation of a porous orifice tube and relevance to the capillary-interstitial fluid circulation: Preliminary report”. Medical Hypotheses 56.3 (2001): 325-334.
- Ghanem AN. “Prospective Observational Study on Loin Pain Hematuria Syndrome Complicating Symptomatic Nephroptosis and the Results of Renal Sympathetic Denervation and Nephropexy Surgery”. Journal of Nephrology and Urology 3.1 (2016): 024.
Citation:
Ahmed N Ghanem. “Ghanem’s new discoveries in Medicine, Physiology, Urology and Nephrology?” Chronicle of Medicine and
Surgery 2.5 (2018): 256-259.
Copyright: © 2018 Ahmed N Ghanem. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.