Research Article
Volume 1 Issue 3 - 2018
Nodular Hypertrophy of Prostate in Digital Rectal Examination: Confrontation Ultrasonography-Pathology
1Department of Radiology and Imaging of the Mother University Hospital Elizabeth Domitien (Chumed), Central African Republic)
2Department of Urology and Andrology of the Hospital of Friendship (Central African Republic)
3Department of Radiology and Imaging at the Bangui Community Hospital, Central African Republic
4Head of Department of Radiology and Imaging of the Hospital of Friendship (Central African Republic)
2Department of Urology and Andrology of the Hospital of Friendship (Central African Republic)
3Department of Radiology and Imaging at the Bangui Community Hospital, Central African Republic
4Head of Department of Radiology and Imaging of the Hospital of Friendship (Central African Republic)
*Corresponding Author: Kouandongui Bangue Songrou Francky, Department of Radiology and Imaging of the Mother University Hospital Elizabeth Domitien (Chumed), Central African Republic).
Received: June 11, 2018; Published: June 14, 2018
Summary
Objective: The objective of this work is to compare the performance of ultrasound to that of pathology in the detection of prostate cancer in patients with nodular hypertrophy of the prostate in the digital rectal examination.
Patients and Methods: This was a cross-sectional study conducted between the periods of 2nd, January 2016 to 2nd, January 2017 (12 months) in the Department of Radiology and Imaging, at the Hospital of Friendship in Bangui, Central African Republic. Included in this study were all records of patients who had nodular hypertrophy from the prostate to digital rectal examination, who had performed an ultrasound of the prostate and had surgery. The results of the ultrasound were compare to those of the pathological examination.
Results: 91 prostate ultrasound were performed in total. 69 cases or 75.8% were in favor of benign prostatic hypertrophy. A representation of 24.2% or 22 cases of prostate compatible with cancer were detected. The comparison between ultrasound and pathological examination in terms of detection of prostate cancer revealed 07 true positives, 15 false positives, 63 true negatives and 06 false negatives. Ultrasound did not detect all prostate cancers, and some benign prostatic hypertrophies were consider cancers of the prostate. The sensitivity of ultrasound in the detection of prostate cancer was 53.8% and its specificity was 80.8%.
Conclusion: The ultrasound of the prostate finds its place in the realization of echo-guided biopsies of the abnormal zones. The recommended techniques for the detection of prostate cancer are the assay of PSA combined with digital rectal examination. Only the pathological examination remains the confirmation examination of prostate cancer.
Keywords: Prostate; Hypertrophy; Ultrasound; Biopsy; Cancer
Introduction
Prostatic pathologies are common and occupy a central stage in the subjects of urology practice for more than 40 years [1]. Of all these pathologies, prostate cancer is the second leading cause of death after lung cancer. Several diagnostic strategies have been introduced in recent years. Prostate-specific antigen (PSA) and digital rectal examination are recognized as best procedures [2,3]. Prostate ultrasound is the least expensive and commonly performed imaging method [4]. The aim of this work is to compare the performance of ultrasound to that of pathology in detecting prostate cancer in patients with nodular hypertrophy from the prostate to the digital rectal examination.
Patient and Methods: This was a cross-sectional study conducted within the periods of January 2nd, 2016 to January 2nd, 2017 (12 months), in the Department of Radiology and Imaging unit at the Hospital of Friendship in Bangui, Central African Republic. Included in this study were all records of patients who had nodular hypertrophy of the prostate in the digital rectal examination, who had performed an ultrasound of the prostate for this purpose, who had undergone surgery (adenomectomy) and whose operative specimen had been analysed.
The ultrasound examinations were divided into two groups (prostates compatible with benign prostatic hypertrophy and prostates compatible with prostate cancer). The results of the ultrasound were compared with those of the pathological examination. The criteria for prostate malignancy on ultrasound were; rounded area, irregular contours, hypoechoic, generally developed in the peripheral zone; visualization of a hypo-echoic nodule, vascularized of the peripheral zone, rupture of the prostatic capsule. In favour of benign hypertrophy, any hypertrophy of the cranial prostate realizing a variable nodular appearance, maybe accompanied by small cystic formation or calcification, which repressed and laminated the peripheral prostate. This hyperplasia could lift the bladder floor. The contours of the prostate remained regular [5,6].
Results
Characteristics of the population
From January 02, 2016 to January 02, 2017, 91 files met our inclusion criteria. The average age was 67.7 years old, with the extremes of 52 and 93 years old. The most represented age group was 60 to 69 years old.
From January 02, 2016 to January 02, 2017, 91 files met our inclusion criteria. The average age was 67.7 years old, with the extremes of 52 and 93 years old. The most represented age group was 60 to 69 years old.
Ultrasound data
A total of 91 ultrasounds of the prostate were performed endo-rectally. 69 cases or 75.8% were in favor of benign prostatic hypertrophy and were distributed as follows: 31 homogeneous prostates with no focus of color Doppler vascularization (34.1%), 13 prostates with hypoechoic nodules non-vascularized (14.3%) and 25 prostates were the site of non-vascularized echogenic nodules (27.5%). Prostates compatible with cancer were represented at 24.2% or 22 cases. 7 cases (7.7%) corresponded to homogeneous prostates with a focus of Doppler color vascularization, 4.4% of prostate (4 cases) included non-vascularized hypoechoic nodules, with fuzzy contours, 9 prostates (9.9%) had vascularized hypoechoic nodules and 2 cases or 2.2% had vascularized echogenic nodules.
A total of 91 ultrasounds of the prostate were performed endo-rectally. 69 cases or 75.8% were in favor of benign prostatic hypertrophy and were distributed as follows: 31 homogeneous prostates with no focus of color Doppler vascularization (34.1%), 13 prostates with hypoechoic nodules non-vascularized (14.3%) and 25 prostates were the site of non-vascularized echogenic nodules (27.5%). Prostates compatible with cancer were represented at 24.2% or 22 cases. 7 cases (7.7%) corresponded to homogeneous prostates with a focus of Doppler color vascularization, 4.4% of prostate (4 cases) included non-vascularized hypoechoic nodules, with fuzzy contours, 9 prostates (9.9%) had vascularized hypoechoic nodules and 2 cases or 2.2% had vascularized echogenic nodules.
Pathological findings
The analysis of the 91 surgical specimens revealed 13 cases of prostate cancer and 78 cases of benign prostatic hypertrophy.
The analysis of the 91 surgical specimens revealed 13 cases of prostate cancer and 78 cases of benign prostatic hypertrophy.
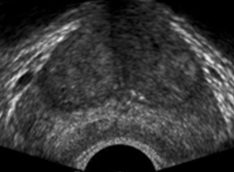
Figure 1: (True positive case of adenoma) Homogeneous prostate in favour
of adenoma in ultrasounds, it has been confirmed in pathology.
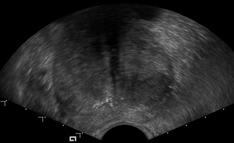
Figure 2: (True positive case of cancer) hypo echoic nodule compatible with
cancer, anatomopathological examination showed prostate cancer.
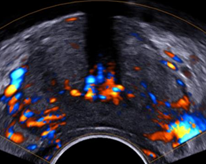
Figure 3: Detection of a color-coding in prostate compatible
with cancer, anatomopathological examination showed adenoma
(false positive case of cancer in ultrasound diagnosis.
| Prostate in favor of HB | Prostate for cancer | |||
| Number | Frequency | Number | Frequency | |
| Homogeneous without color Doppler vascularity focus | 31 | 34,1% | 00 | 00 |
| Homogeneous with color Doppler vascularity focus | 00 | 00 | 07 | 07,7% |
| Non-vascularized hypoechoic nodule | 13 | 14,3% | 04 | 04,4% |
| Nodule hypoechoic vascularized | 00 | 00 | 09 | 09,9% |
| Vascularized echogenic nodule | 00 | 00 | 02 | 02,2% |
| Non-vascularized echogenic nodule | 25 | 27,5% | 00 | 00 |
| Total | 69 | 75,8% | 22 | 24,2% |
Table 1: Ultrasound results.
| Prostate Cancer | Prostate Adenoma | Total | |
| Prostate compatible with cancer | True positives | False positives | |
| 07 | 15 | 22 | |
| Prostate compatible with an adenoma | False negatives | True negatives | |
| 06 | 63 | 69 | |
| Total | 13 | 78 | 91 |
Table 2: Comparison between ultrasound and pathological treatment expressed as true positive, true negative, false positive and false negative.
Expressed as true positives, true negatives, false positives and false negatives
Comparison in terms of false positives and true positives
The comparison between ultrasound and pathological examination in terms of detection of prostate cancer revealed 07 true positives, 15 false positives, 63 true negatives and 06 false negatives. Ultrasound did not detect all prostate cancers, and some benign prostatic hypertrophies were considered cancers of the prostate. The sensitivity of ultrasound in the detection of prostate cancer was 53.8% and its specificity was 80.8%.
Comparison in terms of false positives and true positives
The comparison between ultrasound and pathological examination in terms of detection of prostate cancer revealed 07 true positives, 15 false positives, 63 true negatives and 06 false negatives. Ultrasound did not detect all prostate cancers, and some benign prostatic hypertrophies were considered cancers of the prostate. The sensitivity of ultrasound in the detection of prostate cancer was 53.8% and its specificity was 80.8%.
Discussion
Benign prostatic pathologies are frequent and dominate the prostatic pathologies subject for more than 40 years [7,8]. In our series, they represent 85.7%, equal to the 86.3% of Traore., CB., et al. 2006 [9] and above the 57.5% of Costa P., et al. 2004 [10]. Ultrasound-pathology comparison reveals that ultrasound is not sensitive in the detection of prostate cancer. Its sensitivity is 53.8% and its specificity is 80.8%. Stamey., et al. 1989 [11] in their series reported 52% sensitivity. In the detection of cancer, several prostate cancers escape ultrasound. Despite all the improvements of ultrasound (mode B, Doppler mode), this technique cannot be considered as a screening and detection technique for prostate cancer.
It does not detect non-palpable cancer in half of the cases [12]. There is no specific aspect of prostate cancer on ultrasound, even endo-rectally. Normal ultrasound does not rule out prostate cancer [13]. According to Descotes JL [14], the role of endo-rectal ultrasonography in the diagnosis of prostate cancer remains limited, apart from the indispensable help it provides for the randomization of biopsies. In the field of early diagnosis, the limits of imaging are link to the multi-focal function of prostate cancer in 85% of cases, to the non-specific nature of prostatic ultrasound anomalies, to the great variability of the ultrasound images of these tumours that can present themselves in the form of hypo echoic nodules, hyper echoic or iso-echogenic difficult to distinguish benign tissue. The proposed prostate cancer screening tests are the prostate specific antigen (PSA) assay coupled to the digital rectal examination [2,15,16]. Nevertheless, it has been shown that hypo echogenic lesions are twice as cancerous at biopsy as ischemic lesions [17,18].
The echography-anatomopathologie comparison of prostates with a focus of color Doppler hyper-vascularization showed that 3 times out of 4, the results of the ultrasound were consistent with those of the anatomopathological examination on the cancerous nature of the prostate. According to Master., et al. 2006 [13] the detection of a color-coding (hyper vascularized nodule) within a nodule or hypoechoic area significantly increases the risk of this lesion being cancer.
Sauvain., et al. 2000 [19] obtained the same results, the color Doppler according to them, improves the positive predictive value of ultrasound diagnosis of prostatic cancers in cases of hypoechoic nodules or a hypoechoic area within the prostate.
The discrepancy of results between ultrasound and pathology shows that ultrasound has its limits. This diagnostic means remains primarily an orientation test. Certainly, a diagnostic tool can detect non-palpable adenocarcinoma. However, also and above all a technical element allows biopsy hypo echoic nodules and ideally position the biopsy needle. Confirmation of the benign or malignant character of hypertrophy is the result of anatomopathological examination [17,18,20].
Conclusion
Prostate ultrasound finds its place in performing echo-guided biopsies of the abnormal areas it has previously allowed to highlight. The recommended techniques for the detection of prostate cancer are the assay of PSA combined with digital rectal examination. Only the pathological examination remains the confirmation examination of prostate cancer.
References
- Elezra E., et al. "Evolution de la prise en charge chirurgicale des cancers de la prostate: analyse nationale du codage”. Progrès en urologie 22.12 (2012): 711-717.
- Yousra S., et al. ”Apport du PSA et de sa densité dans le diagnostic et le dépistage du cancer de la prostate”. Annales De Biologie Clinique 68.5 (2010): 585-593.
- Villers A., et al. ”Dépistage du cancer de la prostate”. Progrès en Urologie 13 (2003): 209-214.
- Crozier F., et al. ”Echographie prostatique en pratique radiologique quotidienne : enquête auprès de 122 radiologues”. Progrès en Urologie 9 (1999): 95-100.
- Seguin G, Giuria A, Convard J P. Pelvis masculine. In: Echographie. Ed by Legmann P, Bonnin-Fayet P, Convard J P, Seguin G. Paris: Masson 2008: 144-147.
- Rifkin M., et al. “Prostate: techniques, results and potential applications of colour Doppler US scanning”. Radiology 186.2 (1993): 509-513.
- Fourcade RO., et al. “Prévalence des troubles du bas appareil urinaire et de l’incontinence chez les adultes auxerrois”. Presse Medicale 31 (2002): 202-210.
- Girman CJ. “Population-based studies of the epidemiology of benign prostatic hyperplasia”. British Journal of Urology 82 (1998): 34-43.
- Traore CB., et al. “Aspects anatomopathologiques, cliniques et radiologiques des tumeurs bénignes de la prostate au Mali, à propos de 759 cas“. Mali médical 4 (2006): 32-34.
- Costa P., et al. “Hyperplasie Bénigne de la Prostate (HBP): prévalence en médecine générale et attitude pratique des médecins généralistes français. Résultats d’une étude réalisée auprès de 17.953 patients ». Progrès en Urologie 14 (2004): 33-39.
- Stamey TA and Kabalin JN. “PSA in the diagnosis and treatment of adenocarcinoma of the prostate. I: untreated patients”. Journal of Urology 141.5 (1989): 1070-1075.
- Latorzeff I and Gamé X. “Le cancer de la prostate“. Bulletin infirmier du cancer 11.2 (2011): 43-53.
- Lemaître L., et al. “Échographie et biopsies de prostate“. Journal de Radiologie 87.21 (2006): 201-209.
- Descotes JL., et al. “Apport de l'imagerie dans le cancer de prostate“. Progres En Urologie 13 (2003): 843-884.
- Villers A., et al. “Dépistage du cancer de la prostate". Progrès en Urologie 13 (2003): 209-214.
- Villers A and Gros Claude P. “Épidémiologie du cancer de la prostate: Article de revue Epidemiology of prostate cancer“. Médecine Nucléaire 32.1 (2008) : 2-4.
- Barry M., et al. “Aspects diagnostics des tumeurs prostatiques au service d’urologie du CHU de Conakry“. Médecine d’Afrique Noire 57.1 (2010): 32-36.
- Akpo CE., et al. “Apport du toucher rectal, du dosage du PSA, de l’échographie et de la biopsie dans le diagnostic des tumeurs prostatiques au CNHU de cotonou. A propos de 64 cas en deux ans : 1994 et 1995“. Médecine d'Afrique Noire 46.5 (1999) : 271-275.
- Sauvain JL., et al. “Vascularisation intra prostatique en imagerie Doppler puissance et vasculaire 3D : critères d’analyse et intérêt dans l’établissement du diagnostic et du stade évolutif des cancers“. Progrès en Urologie 10 (2000): 237-245.
- Lechevallier E. “La ponction biopsie de prostate“. Progrès en Urologie 6 (1996): 507-518.
Citation:
Kouandongui Bangue Songrou Francky., et al. “Nodular Hypertrophy of Prostate in Digital Rectal Examination: Confrontation
Ultrasonography-Pathology”. Archives of Endocrinology and Diabetes Care 1.3 (2018): 107-112.
Copyright: © 2018 Kouandongui Bangue Songrou Francky., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.