Editorial
Volume 2 Issue 1 - 2018
Endometriosis an Enigma- Review Article
1Professor, Department of Obstetrics & Gynaecology ESICMCPGIMSR Rajajinagar, Bangalore, Karnataka, India
2Junior Resident, Department of Obstetrics & Gynaecology ESICMCPGIMSR Rajajinagar, Bangalore, Karnataka, India
3Assistant Professor, Department of Obstetrics & Gynaecology ESICMCPGIMSR Rajajinagar, Bangalore, Karnataka, India
2Junior Resident, Department of Obstetrics & Gynaecology ESICMCPGIMSR Rajajinagar, Bangalore, Karnataka, India
3Assistant Professor, Department of Obstetrics & Gynaecology ESICMCPGIMSR Rajajinagar, Bangalore, Karnataka, India
*Corresponding Author: Dr. Sreelatha S, Professor, Department of Obstetrics & Gynaecology ESICMCPGIMSR Rajajinagar, Bangalore, Karnataka, India.
Received: January 25, 2018; Published: March 13, 2018
Abstract
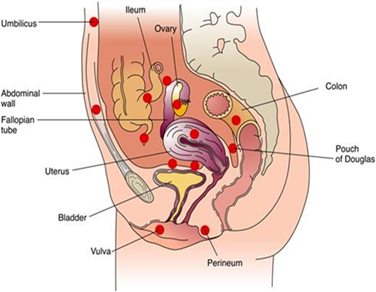
Endometriosis is the presence of tissue similar to uterine endometrium in locations other than its normal physiological location. It is considered to be a disease of 20th or 21st century due to significant increase in incidence, and affects 8-10% of women in reproductive age group. These heterotopic endometrial glands are capable of responding to endogenous as well as exogenous hormonal stimulation. These heterotopic island of tissue is most commonly seen in pelvic cavity (i.e., Ovaries, pouch of Douglas, uterosacral ligament, rectovaginal septum) but can also be seen in abdominal cavity (bowel, omentum) and outside(lungs, brain).
It can present with mild dysmenorrhoea to severe distressing symptoms like chronic pelvic pain, dyspareunia and infertility in 30% of cases. Diagnostic laparoscopy is the gold standard procedure for the confirmation of the diagnosis. The treatment revolves around the location and symptoms with which the patient presents with and ranges from hormonal suppression to total hysterectomy. This paper thus highlights the enigmatic aspect of this disease.
Keywords: Endometriosis; Infertility; Chronic pelvic pain; Diagnostic laparoscopy; Hysterectomy
Introduction
Endometriosis is a chronic and recurrent condition in which endometrium like tissue present outside the uterus. It affects 8-10% of women in reproductive age group; among whom 30% present with primary or secondary infertility [2]. It is a benign condition but occasionally accompanies endometrioid and clear cell carcinomas.
History: Although considered the disease of 20th or 21st century, the first reference of endometriosis goes back to 1500 B.C (Ebers Papyrus) in which treatment to “painful disorder of menstruation” is described. Later Knapp performed an historical review on the disease in 17th and 18th century [3]. The term “chocolate cyst” was first used by Brue in 1894.
Etiopathogenesis: Several theories have been proposed regarding the histogenesis of endometriosis. Ridley grouped them into 3 categories [4]
- Transplantation.
- Coelomic metaplasia.
- Metaplasia induced by factors released into the peritoneal cavity.
However Sampson’s transplantation and implantation (theory of retrograde menstruation) is the most widely accepted theory. Simpson., et al. also stressed the genetic and constitutional predisposition with inherited tendency for the genesis of endometriosis [5].
Other theories proposed are
- Direct implantation of endometrial cells.
- Activation of embryonic cell rests.
- Lymphatic dissemination [7].
Location of Occurrence: These heterotopic island of tissue is most commonly seen in pelvic cavity (i.e., Ovaries, pouch of Douglas, uterosacral ligament, rectovaginal septum) but can also be seen in abdominal cavity (bowel, omentum) and outside(lungs, brain).
Risk Factors:
- Early age at menarche
- Nulliparity
- Mullerian anamolies
- 1st degree relative
- Drug exposure to DES,PCB,DIOXIN
Symptoms: 6D”S
- Painful menstruation (dysmenorrhoea)
- Painful intercourse (dyspareunia)
- Painful defecation (dyschezia) that may be cyclic or semi-cyclic.
- Painful micturition (dysuria)
- Dull aching pain (chronic pelvic pain)
- Disorders of menstruation ( menorrhagia)
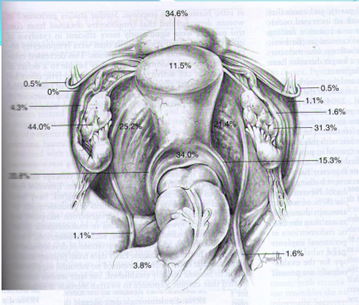
The pathology is located more on left side due to close anatomical relationship between the sigmoid colon and left fallopian tube which creates an isolated zone favouring the implantation of endometrial cell carried by the tubal reflux into the peritoneal cavity [8,9].
Infertility
Atypical presentations include cyclic leg pain or sciatica (nerve involvement), cyclic rectal bleeding or haematuria (bowel or bladder invasion), and cyclic dyspnoea secondary to cat menial pneumothorax. These presentations are indicative of a more significant disease involvement.
Atypical presentations include cyclic leg pain or sciatica (nerve involvement), cyclic rectal bleeding or haematuria (bowel or bladder invasion), and cyclic dyspnoea secondary to cat menial pneumothorax. These presentations are indicative of a more significant disease involvement.
Mechanism for Infertility:
- Mechanical interference
- Hormonal/Ovulatory
- Alteration in Peritoneal fluid (↑Pg, Cytokines, Phagocytosis of Sperm)
- Altered immune response
- Implantation failure
Diagnosis
Generally, diagnosis of endometriosis is based on the history, the symptoms and signs, physical examination and imaging techniques. Physical examinations should include an assessment to determine the position, size, and mobility of the uterus. Rectovaginal examinations are useful in determining presence of DE. Other than the examination of the pelvic region, inspection and palpation of the abdomen is also advised.
Generally, diagnosis of endometriosis is based on the history, the symptoms and signs, physical examination and imaging techniques. Physical examinations should include an assessment to determine the position, size, and mobility of the uterus. Rectovaginal examinations are useful in determining presence of DE. Other than the examination of the pelvic region, inspection and palpation of the abdomen is also advised.
USG-1st line of modality- Trans vaginal or endo rectal ultrasonography may reveal ultra sonographic features varying from simple cysts to complex cysts with internal echoes to solid masses, usually devoid of internal vascularity but shows pericystic flow with high resistance. CA-125-nonspecific marker, to exclude ovarian ca.
Laproscopy
Direct visualisation with laparoscopy and histology has been regarded as the gold standard for diagnosis. Types of lesions on laparoscopy are powder burn or black lesions, white pacified peritoneum, glandular excrescences, flame like red lesions, peritoneal pockets or windows, clear vesicles, yellow brown patches, unexplained adherence of ovary to peritoneum of ovarian fossa, encysted collection of thick chocolate coloured or tarry fluids, adhesions to posterior lip of broad ligaments or other pelvic structures. When endometriosis is thought to be of the DE variety, ancillary tests such as colonoscopy, cystoscopy, rectal ultrasonography, and MRI may be required [6,7].
Direct visualisation with laparoscopy and histology has been regarded as the gold standard for diagnosis. Types of lesions on laparoscopy are powder burn or black lesions, white pacified peritoneum, glandular excrescences, flame like red lesions, peritoneal pockets or windows, clear vesicles, yellow brown patches, unexplained adherence of ovary to peritoneum of ovarian fossa, encysted collection of thick chocolate coloured or tarry fluids, adhesions to posterior lip of broad ligaments or other pelvic structures. When endometriosis is thought to be of the DE variety, ancillary tests such as colonoscopy, cystoscopy, rectal ultrasonography, and MRI may be required [6,7].
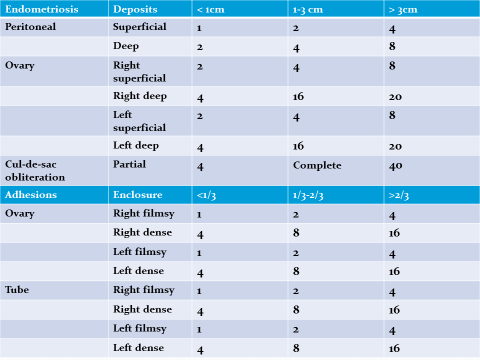
American Fertility Society Scoring System of Endometriosis
Recurrence and Malignancy Risk
Malignancy risk - 0.7–1%.
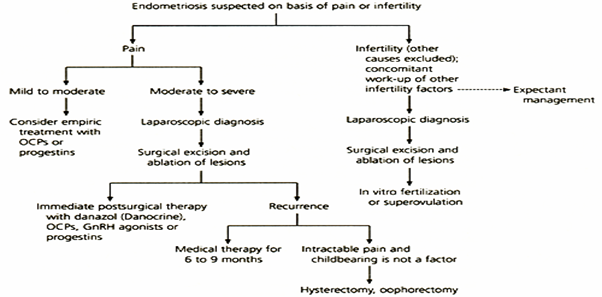
Recurrence: Medical management-pelvic pain is seen in 50% cases within 1 year, after 1 year of conservative surgery, 25-45% have pelvic pain and recurrence detected by clinical or ultrasound examination between 9-15%, combined medical + surgery- recurrence of pain in 26%, 8% in usage. Endometriosis is treated medically, surgically, or through a combination of both [7].
Malignancy risk - 0.7–1%.
Recurrence: Medical management-pelvic pain is seen in 50% cases within 1 year, after 1 year of conservative surgery, 25-45% have pelvic pain and recurrence detected by clinical or ultrasound examination between 9-15%, combined medical + surgery- recurrence of pain in 26%, 8% in usage. Endometriosis is treated medically, surgically, or through a combination of both [7].
Management: Management depends upon presenting complaint and clinical finding. No treatment is curative, only pain relief and fertility can be optimised.
Medical Management
- Pain Medication
- Hormonal Medication
Medical management includes management of pain with analgesics, as well as hormonal suppression, used to treat symptoms. It does nothing to improve fertility, treat adhesions, or resolve endometriomas.
| Debulking | Surgery |
| Estrogen reduction |
|
| Reducing inflammatory response |
|
| Endometrial atrophy |
|
| Treatment | Principles of usage |
| Surgical treatment |
|
| Medical treatment |
|
| First line medical treatment |
|
| Second line medical treatment | GnRH agonists with add back therapy, LNG-IUS |
Surgical Management:
- Definitive surgery Hysterectomy with or without removal of the ovaries is for women who do not desire fertility or for women for whom conservative surgery has failed.
- Conservative surgery Conservative surgery preserves the uterus, tubes and ovaries as much as possible and is focused on removing endometriosis and improving symptoms through endometriosis fulguration, endometriosis resection (or endometriosis excision) or resection of endometrioma [6,7].
Conclusion
Although endometriosis is a surgical diagnosis, medical management with ovarian suppression remains the mainstay of long-term management with superimposed surgical intervention when needed. The goal of surgery should be excision or ablation of all visible disease to minimize risk of recurrence and need for repeat surgeries.
References
- Pedro Acién and Irene Velasco. “Endometriosis: A Disease That Remains Enigmatic” ISRN Obstetrics and Gynecology 2013 (2013): 12.
- V. Ruiz-Velasco. Endometriosis, Intersistemas, Mexico (2004).
- V. J. Knapp. “How old is endometriosis? Late 17th- and 18th-century European descriptions of the disease”. Fertility and Sterility 72.1 (1999):10–14.
- J. H. Ridley. “The histogenesis of endometriosis: a review of facts and fancies”. Obstetrical & Gynecological Survey 23.1(1968) 1-35.
- J L Simpson., et al. “Heritable aspects of endometriosis. I. Genetic studies”. American Journal of Obstetrics and Gynecology 137.3 (1980): 327–331.
- Studd JWW and Thom MH. “Oestrogens and endometrial cancer”. In: Studd JWW, ed. Progress in obstetrics and gynaecology, vol I. Lon-don: Churchill Livingstone (1981):182-198.
- Leyland N, et al. “Endometriosis: Diagnosis and Management”. Journal of Obstetrics and Gynaecology Canada 32.7 Suppl 2 (2010): S1–S3
- Thompson JD., et al. Te Linde's operative gynecology. Philadelphia: Lippincott (1992):
- Parazzini F. “Left: Right side ratio of endometriotic implants in the pelvis”. European Journal of Obstetrics & Gynecology and Reproductive Biology 111 (2003): 65-67.
- Vercellini P., et al. “Is cystic endometriosis an asymptomatic disease?” British Journal of Obstetrics and Gynaecology 105 (1998): 1018-1021.
Citation:
Sreelatha S., et al. “Endometriosis an Enigma- Review Article”. Gynaecology and Perinatology 2.1 (2018): 212-217.
Copyright: © 2018 Sreelatha S., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.