Case Report
Volume 2 Issue 2 - 2018
Hemicorea and Changes in Resonance Imaging in Hyperglycemic State Not Cetocico.
1Clinical neurologist, Medellin clinic of Colombia
2Corporacion Universiaria Rafael Núñez, Bolivar, Medical interna, Colombia
2Corporacion Universiaria Rafael Núñez, Bolivar, Medical interna, Colombia
*Corresponding Author: Wolfang Rubio Rodríguez, Corporacion Universiaria Rafael Núñez, Bolivar, Medical internal, Colombia.
Received: July 14, 2018; Published: July 24, 2018
Abstract
Defined as Korea to involuntary, that is of short duration, irregular, non-rhythmic movement, it takes place without any purpose that
migrates from one part of the body to another randomly; in usual conditions occurs at rest, they exacerbate with distracting maneuvers,
transferred with the dream and its most notorious motor manifestation describes a pattern of “form of dance” reason why it was
called that way; Sometimes the coreicos movements can be deleted temporarily in a partial manner, even the patient can camouflage
them by incorporating them within their regular movements, (paraquinesia); Chorea may be the manifestation of a primary disorder
or may be the manifestation of or systemic complications, toxic or other entities, each one of these cases allows evidence in images of
neuro diagnostic changes at the level of the nuclei of the base that are permanently and that are in many cases evidence of the causes
of the origin of this disorder, however on some occasions the lesion evidenced can have a transitional character and be related to
metabolic instability in the which one time is resolved, disappearing symptoms; This review will be informed in an adult patient of
66 years laco enter to the emergency room by a picture of subacute development of abnormal movements consisting of choreiform
movements of the hemibody origin, which is why a neuro image is taken in the which is a lesion right gangliobasal in context of patient
with history of diabetes mellitus not controlled known in medical literature as C.H.B.G (Korea/hyperglycemia/basal ganglia),
the hemicorea slowly improved during the course of hospitalization with glycemic control.
Key word: Ketosis; Korea; Basal ganglion; Hyperglycemia; Hyperintensity
Abbreviations: C.H.B.G: Korea/hyperglycemia/basal ganglia, HB-HC; Hemiballismus hemicorea, CT; Computed tomography of brain:
RMI; Magnetic resonance imaging, SHNC: Syndrome Hyperglycemic hyperosmolar Nonketotic coma; PET: Positron emission tomography
Introduction
The clinical phenomenon of Chorea has been recognized for many centuries being attributed to many causes, the term derives from the Greek word χορει'α that describes a type of traditional dance; involuntary movements were described for the first time as Dance by the physician and Alchemist Paracelsus in the 16th century referring as "St. Vitus dance" danse de St. Guy (the French name of San Vito). In the 17th century, the English physician Thomas Sydenham said the development of Chorea children, this childhood disorder was also known as Chorea minor, to distinguish it from the epidemic and acute forms of adult, the connection with rheumatism, fever and the use of the eponymous "Sydenham Chorea" was made later by Charcot in 1887, finally the clarification as to the existence of different forms of Korea hereditary and acquired was made by William Osler in 1894.
Today it is known that you Chorea may result from a variety of clinical conditions that give characteristics to the type of progression, causes including is including strokes, metabolic, neurodegenerative, infectious, toxic, immune disorders, Wilson disease, thyrotoxicosis (1) the State Hyperglycemic Nonketotic coma. The term Hemiballismus hemicorea (HB-HC) is commonly used to describe dysfunction basal ganglion in elderly patient with State Hyperglycemic non cetocico, an unusual clinical entity characterized by continuous involuntary movements proximal and distal with Neuroradiological findings in cerebral (CT) and magnetic resonance imaging (MRI). In the study show the clinical picture of one adult female patient with metabolic instability given by hyperglycaemic State not cetocico that induces HB-HC. Paraclinical studies of the patient includes ketones in urine positive (see table 1) as well as a CT, MRI, which had particular hyper density in the contralateral knurled area next to HB-HC in the TC, and high signal intensity in the putamen in image weighs in MRI T1.
Materials and Methods
66-year-old female patient who attends the service concerned a unit of basic care (AUB); talking about picture of course sub-acute of 5 days of evolution at the time of entry, consisting of occasional movements of low frequency and high amplitude involving predominantly the right upper limb and subsequently in a span of 72 hours agrees of ipsilateral lower limb; concomitant picture with general symptoms of fatigue, weakness, polydipsia, polyuria and hiporexia; vital signs at the time of the entry demonstrate stability and neurological examination shows as only positive finding choreiform movements of the right hemibody origin.
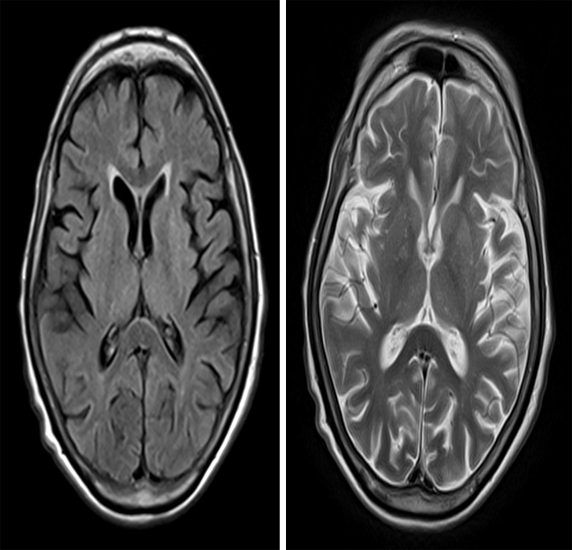
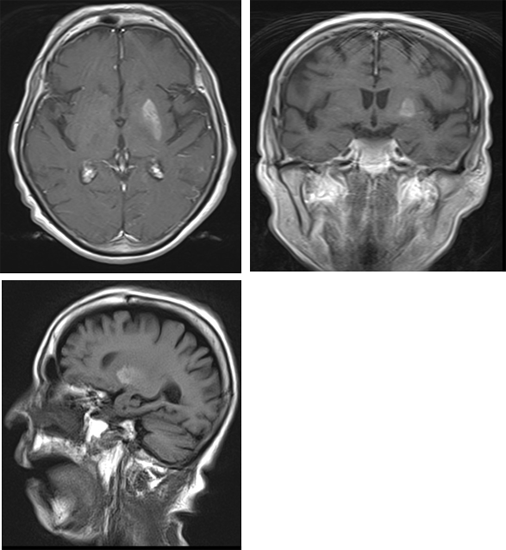
At the time of admission is decided to leave in hospitalization in neurology service with diagnosis of abnormal movements syndrome by possible compromise gangliobasal and determine etiology and onset of management for control of given metabolic instability by been Hyperglycemic non cetocico; (besides Imaging (MRI) of control, reported: [1] Lesion in the left putamen with atrophy that for his hiperintenso behavior in T1, the radiological evolution and the history of Decompensated diabetes could be related to hemicorea Hyperglycemic Nonketotic: However there is no restriction on the dissemination or alteration in spectroscopy being reported in these cases. A possible diagnosis serious difference multiple systemic atrophy with parkinsonian manifestations. [2] Lacunar infarctions subacute at the construction right, occipital right and periatrial left Center suggesting etiology thromboembolic. [3] Evolutional changes relating to the age of the patient with microangiopathic leukoencephalopathy. [4] Chronic sinusitis etmoidoesfenomaxilar with in the right maxillary sinus mucous retention cysts and signs of fungal super infection in the left maxillary sinus without changes from the previous study. (See images). To achieve metabolic control scheme of insulin’s patient gradually improved abnormal movements until total normal 7 days of metabolic control in the same way disappeared general symptoms described at the moment income.
Results and Discussion
The hemicorea consists of series of contractions involuntary, followed, quick and sudden, affecting a part of the body. [2] Unilateral choreiform movements, are often approximately 0.7% of all disorders of the movement and, usually, coexisting with a structural disease, such as contralateral vascular injury. [3] Its most important complication is called Hemiballismus. Result of a lesion in the putamen contralateral. [2] There are multiple causes of injury putaminal. The most common is the vascular, secondary to ischemic stroke in the sub thalamic area, although it may also occur after injuries in other areas such as thalamus, striatum or cortico-subcortical areas. In order of frequency follows syndrome Hyperglycemic hyperosmolar Nonketotic coma (SHNC), [4] which is a clinical syndrome of severe hyperglycemia, hyperosmolarity and intracellular dehydration without Ketoacidosis. This syndrome is associated with various neurological disorders, including movement disorders and is the second most frequent cause of HB-HC. [2]
The diabetic HC-HB has been reported as a benign syndrome, which predominantly is associated in postmenopausal women with diabetes mellitus non-insulin; [5] with improvement completed within the 10 months in 76% of patients; [6] the striatal lesion is hyperintense T1 explained as Petechial hemorrhage (7) or ischemia [8], usually disappears after clinical recovery; in some cases with persistent or recurrent HC-HB, can obey the variations of blood glucose levels, including also the recurrent hypoglycemia [9] or the rapid correction of hyperglycemia (1) have been demonstrated in the phase acute to chronic, the possibility of vascular anomaly has been suggested by lesions in contrasting images on T1-weighted in the area of the striated striated. [10] They can account for pathophysiological vascular Obliterative disease with prominent vascular proliferation, as similarly in proliferative retinopathy. [11] Taking into account the recurrence after the rapid correction of blood sugar and the persistence of hyperintensity in the images you ponderas in T2 similar to diabetic retinopathy.
The results of the neuroradiologica image are characteristic in patients with CH BG , occur characteristically in cases reported in the literature and are defined as: computed tomography (CT) with hiperatenuacion in the striated contralateral to the affected side; magnetic resonance imaging (MRI) shows Hiperintensidades weighted in T1 in the striatum [12] and globus pallidus, with restricted diffusion; spectroscopy may show low levels at the peak of N-acetyl aspartate in relation to creatinine peak and peak of high hill with respect to creatinine associated lactate peak, on the other hand the (PET) Positron Emission Tomography has demonstrated a decrease in the metabolism of glucose in the basal ganglia. The basal ganglia are a group of nuclei in the base of the cerebral hemispheres. They consist of the striatum (caudate and putamen), the balloons pallidus, sub thalamic nucleus and substantia nigra. These, along with the motor thalamus, cerebellum and frontal cortex, constitute a complex system that works in a comprehensive way to ensure the Organization and execution of normal patterns of movement. [2] The pathophysiology that hyperglycemia causes basal ganglia lesion is not clear. A first hypothesis is a Petechial hemorrhage in the area of the artery lenticulostriate that irrigates the spline kernel, although the putamen biopsy does not show hemosiderin. A second theory would be hypofunction, with decreased blood flow and metabolic activity, the putamen contralateral.
It is postulated a third theory, a vascular mechanism by hyperglycemia-induced hyperviscosity. [4] CH BG , occur characteristically in cases reported in the literature and are defined as: computed tomography (CT) with hiperatenuacion in the striated contralateral to the affected side; magnetic resonance imaging (MRI) shows Hiperintensidades weighted in T1 in the striatum [12] and globus pallidus, with restricted diffusion; spectroscopy may show low levels at the peak of N-acetylaspartate in relation to creatinine peak and peak of high hill with respect to creatinine associated lactate peak, on the other hand the (PET) Positron Emission Tomography has demonstrated a decrease in the metabolism of glucose in the basal ganglia. The basal ganglia are a group of nuclei in the base of the cerebral hemispheres.
They consist of the striatum (caudate and putamen), the balloons pallidus, subthalamic nucleus and substantia nigra. These, along with the motor thalamus, cerebellum and frontal cortex, constitute a complex system that works in a comprehensive way to ensure the Organization and execution of normal patterns of movement. [2] The pathophysiology that hyperglycemia causes basal ganglia lesion is not clear. A first hypothesis is a Petechial hemorrhage in the area of the artery lenticulostriate that irrigates the spline kernel, although the putamen biopsy does not show hemosiderin. A second theory would be hypofunction, with decreased blood flow and metabolic activity, the putamen contralateral. It is postulated a third theory, a vascular mechanism by hyperglycemia-induced hyperviscosity. [4]
The pathogenesis of the syndrome ch - BG is has failed to elucidate fully, however there are several mechanisms involved in the development of it, means, mechanism mediated by Hyperglycemia is the noxa that prevents the brain, causing self-regulation hypoperfusion and the activation of the anaerobic metabolism and depletion of the acid range amino butyric acid (GABA) in the neurons of the basal ganglia. [13,14] GABA is inhibitory neurotransmitter main basal ganglia this neurotransmitter and acetate are quickly depleted in hyperglycemia not cetocica, causing a reduction in the synthesis of acetylcholine [1]; Hyperglycemia-induced hyperviscosity causes a disruption of the blood-brain barrier and transient ischemia of striatal neurons; [15] the synergistic effects of hyperglycaemia and vascular failure cause a failure and temporary dysfunction of the striatum. This is reinforced by the histological finding in patients with syndrome ch - BG which reported neuronal loss, gliosis and reactive astrocytes, without evidence of haemorrhage or infarction in grooved areas. [16]
| Blood count | Leukocytes | 11,500 - n: 70% |
| Hemoglobin | 10 mg/dl | |
| Hematocrit | 37% | |
| Platelets | 320.00/mm3 | |
| Blood sugar | 378 mg/dl | |
| Azoados | BUN | 16 mg/dl |
| Creatinine | 0.8 mg/dl | |
| Ionogram | NA+ | 137 mmol/l |
| K+ | 4.3 mmol/l | |
| CL-- | 100 mmol/l | |
| PCR | 5.5 mg/dl | |
| Tests of liver injury | TGO | 14 U/L |
| TGP | 14 U/L | |
| Uroanalisis | No evidence bacteriuria or pyuria ketones negative | |
| TSH | 2.74 mlU / L | |
| FT4 | 0.91 mlU/L | |
| Extended peripheral blood | without alterations | |
| VDRL AND HIV | Non-reactive | |
| Arterial blood gas | without alterations | |
Table 1: Paraclinical at the time of the entry.
Nuclear magnetic resonance
Conclusion
Chorea is a movement disorder commonly seen in the areas of neurological care that can arise from a multiplicity of causes and with a wide variety of mechanisms of their appearance; many of them are determined to an irreversible and, this may even make taking management behaviors that may be unnecessary or even increase the morbidity and mortality of the patient; This is why details, medical history, completeness in the neurological examination and the proper interpretation of a neuroimaging guarantee the socket of conduct with greater assertiveness diagnosed and better management of patient scheduling; Some studies have suggested increased frequency of appearance between the seventh to ninth decade of life, without preference of gender and characteristics in racial groups, with symptoms uni or bilateral and times of evolution of diabetes not discriminated against recent long data of the symptoms or diagnosis. [17] is for this reason that apart from understanding the pathophysiology of the disease, which focuses mainly on the neurobiochemical and circuit functionality caudate-putamen, the proper interpretation of the findings should be hyperintensity in the basal ganglia on T1-weighted images) and reversible character at one time estimated between 6 and 11 months, to perform consistent x-ray clinical diagnosis that increases the precision in search of the genesis of the movements involuntary and not be limited to empirical observations.
Conflict of interest
The authors manifest do not have conflicts of interest in this study.
The authors manifest do not have conflicts of interest in this study.
References
- Hernandez GT., et al. “Chorea, Hyperglycemia, Basal Ganglia Syndrome (ch - BG) in an uncontrolled diabetic patient with normal glucose levels on presentation”. American Journal of Case Reports 15 (2014): 143-146.
- García Fernández E., et al. “Secondary to decompensation Hyperglycemic hyperosmolar Hemiballismus”. Endocrinology and nutrition 55.7 (2008): 308-310.
- Espinoza Lopez DA., et al. “Malformation cerebral cavernomatosa in women presenting with hemicorea: response to haloperidol”. Neurología 32.8 (2017): 554-556.
- Gallego-Galiana J., et al. “Diabetes and motor impairment”. Neurology 32.5 (2017): 332-334.
- Rodriguez Gijón LF., et al. “Hemicorea-Hemiballismus as a debut of type 2 diabetes mellitus: computed tomography and magnetic resonance findings”. Revista Argentina de Radiology 80.4 (2016): 289-292.
- JJ Lin. “Ipsilateral putamen hyperintensity on T1-weighted MRI in non-ketotic hyperglycemia with hemiballism-hemichorea: a case report”. Parkinsonism & Related Disorders 7.4 (2001): 319-321.
- Chang MH., et al. “Putaminal petechial haemorrhage as the cause of chorea: a neuroimaging study”. Journal of Neurology, Neurosurgery, and Psychiatry 63.3 (1997): 300-303.
- Oh SH., et al. “Chorea associated with non-ketotic hyperglycemia and basal ganglia lesion on T1-weighted hyperintensity brain MRI study: a meta-analysis of 53 cases including four present cases”. Journal of the Neurological Sciences 200. (1-2) (2002): 57-62.
- H Hefter., et al. “Persistent chorea after recurrent hypoglycemia”. European Neurology 33.3 (1993): 244-247.
- C Battisti., et al. “Two cases of hemichorea-hemiballism with nonketotic hyperglycemia: a new point of view”. Neurological Sciences 30.3 (2009): 179-183.
- Abe Y., et al. “Diabetic striatal disease: clinical presentation, neuroimaging, and pathology”. Internal Medicine 48.13 9 (2009): 1135-1141.
- Wang L and Song C. “Chorea associated with nonketotic hyperglycemia: An uncommon patient with bilateral movements”. Journal of Clinical Neuroscience 22.6 (2015): 1068-1069.
- Nath J., et al. “Radiological and pathological changes in hemiballism-hemichorea with striatal hyperintensity”. Journal of Magnetic Resonance Imaging 23.4 (2006): 564-568.
- Cheema H., et al. “Hemichorea-hemiballismus in non-ketotic hyperglycaemia”. Journal of Clinical Neuroscience 18.2 (2011): 293-294.
- Slabu H Savedia-Cayabyab., et al. “Permanent haemichorea associated with transient hyperglycemia”. BMJ Case Reports (2011).
- Mittal P. “Hemichorea hemiballism syndrome: the first presentation of type 2 diabetes mellitus as a rare cause of chorea”. Iranian Journal of Radiology 8.1 (2011): 47-49.
- Al - Quliti K and Assaedi E. “Hemichorea unilateral with MRI hyperintensity in Saudi striatal patient with diabetes”. Neurosciences 21.1 (2016): 56-59.
Citation:
Wolfang Rubio Rodríguez and Nicanor Arturo Beleño Ramirez. “Hemicorea and Changes in Resonance Imaging in Hyperglycemic
State Not Cetocico.”. Medical Research and Clinical Case Reports 2.2 (2018): 178-183.
Copyright: © 2018 Wolfang Rubio Rodríguez and Nicanor Arturo Beleño Ramirez. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.