Research Article
Volume 2 Issue 1 - 2017
Evaluation of the Nutritional Status of Hemodialysate Patients
National Institute of Nutrition and Food Technology of Tunis (Tunisia), Department A
*Corresponding Author: Nadia Ben Amor, National Institute of Nutrition and Food Technology of Tunis (Tunisia), Department A. Tunisia.
Received: October 09, 2017; Published: October 25, 2017
Abstract
Introduction: Chronic hemodialysis is often malnourished which can impair the effectiveness of dialysis and increase morbidity and mortality. Evaluation of the nutritional status of these patients is difficult and requires the simultaneous use of several parameters.
Patients and methods: This cross-sectional study involved 30 patients under the age of 65, followed by the nephrology department of Rabta Hospital in Tunis. These patients were recruited during a month from January to February 2017. The assessment of nutritional status was based on: a food survey, anthropometric measurements (dry weight, height, Body Mass Index, percentage of weight loss within six months, brachial circumference), biological assays (hemogram, C-reactive protein, albuminemia, blood cholesterol) and the Nutritional Risk Index.
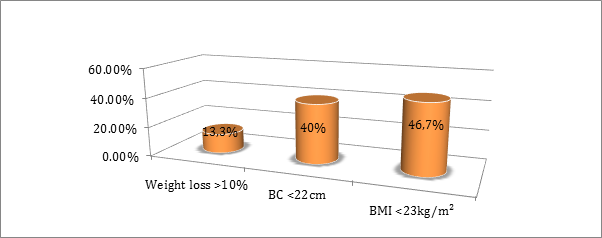
Results: More than half of our patients had an average daily energy intake < 25 kcal/kg/d. Only 6.7% of our patients had satisfactory average daily protein rations. Dietary micronutrient evaluation revealed that our population had insufficient intakes of calcium, iron, vitamins B1 and B9. The frequency of malnutrition varied according to the anthropometric parameter used: 13.3% had a weight loss of more than 10% in the last 6 months, 46.7% had a Body Mass Index < 23 kg/m² and 40% had a brachial circumference < 22 cm. The albuminemia was < 35g/l in 36.6% of cases.
Conclusions: The management of chronic hemodialysis patients must be multidisciplinary: nephrologist, nutritionist and dietician.
Keywords: Hemodialysis; Nutritional intakes; Anthropometry; Albuminemia; Malnutrition
Abbreviations: BMI: Body Mass Index; CRP: C-reactive protein; BC: brachial circumference; NRI: Nutritional Risk Index
Introduction
With increasing life expectancy and the development of certain diseases such as diabetes or high blood pressure, kidney disease affects an increasing share of the population. More than one million people worldwide are being treated with dialysis [1]. In Tunisia, the number of patients with renal insufficiency has increased from 4,200 cases in 2000 to 9,500 cases in 2016. In addition, 600 dialysis patients per million Tunisian residents are registered [2].
Patients with chronic terminal renal insufficiency are often malnourished due to an imbalance between inadequate nutritional intake and catabolism and increased needs [3]. Early diagnosis and management of undernutrition in hemodialysis can reduce the incidence of co-morbidities and improve the efficiency of dialysis, thus providing a better quality of life [4]. As in the general population, evaluation of nutritional status requires the simultaneous use of several clinical, biological and biophysical markers [7].
In our study, it is proposed to evaluate the nutritional status of a group of 30 chronic hemodialysis patients followed regularly in a hemodialysis unit at the Rabta hospital in Tunis.
Patients and Methods
This cross-sectional study involved 30 patients under the age of 65, followed by the nephrology department of Rabta Hospital in Tunis. These patients were recruited during one month from January to February 2017.
- Inclusion criteria: Introduction in hemodialysis for more than 6 months.
- Exclusion criteria: Excluded from this study were all patients with:
- A deterioration in the physical or mental state that does not allow for a coherent response to the interrogation.
- Difficulties to stand on a person scale.
- Hemodynamic instability not allowing to determine the dry weight.
The Assessment of Nutritional status was based on
A food survey
We used the "food history" method of three days: one day of dialysis, one day without dialysis and one day of weekend. For the analysis of foods and their translation into nutrients, we used the Tunisian Food Composition Table (2007 Edition) of the National Institute of Nutrition and Food Technology and that of Regal (CIQUAL 2016), as well as the computer software "BILNUT". In order to determine the nutritional requirements, we referred to the recommendations of the European Best Practice Guidelines [5]. The average energy ration was calculated by comparing the average energy intake to the dry weight of the patient.
A food survey
We used the "food history" method of three days: one day of dialysis, one day without dialysis and one day of weekend. For the analysis of foods and their translation into nutrients, we used the Tunisian Food Composition Table (2007 Edition) of the National Institute of Nutrition and Food Technology and that of Regal (CIQUAL 2016), as well as the computer software "BILNUT". In order to determine the nutritional requirements, we referred to the recommendations of the European Best Practice Guidelines [5]. The average energy ration was calculated by comparing the average energy intake to the dry weight of the patient.
Anthropometric measurements
- The size measured with a rod and the dry weight using a personal scale (performed at the end of the hemodialysis session to limit the artifacts associated with changes in the state of hydration).
- The percentage of weight loss (ΔP (%)) calculated in relation to the previous weight of 6 months. Weight loss greater than 10% in 6 months indicates undernutrition [6]. ΔP (%) = [(usual weight - current weight)/usual weight] x 100
- Body mass index (BMI) defined as the ratio of weight to squared and expressed in kg/m2 (measured from dry weight). A value below 23 kg/m² is an indicator of malnutrition [6].
- The brachial circumference (BC) measured by a tape measure. A value of less than 22 cm is in favor of a significant decrease in muscle mass [6].
Biological measurements
The biological check-up was performed prior to the hemodialysis session, including: blood glucose, serum creatinine, cholesterol, hemogram, albuminemia (assayed by immunophlemetry), CRP. Malnutrition has been defined [] if: albuminemia < 35 g/l [6] (albuminemia was interpreted after CRP verification) and cholesterol levels < 1 g/l [6].
The biological check-up was performed prior to the hemodialysis session, including: blood glucose, serum creatinine, cholesterol, hemogram, albuminemia (assayed by immunophlemetry), CRP. Malnutrition has been defined [] if: albuminemia < 35 g/l [6] (albuminemia was interpreted after CRP verification) and cholesterol levels < 1 g/l [6].
Nutritionnal Risk Index (NRI)
NRI = 1.519 × albuminemia + 0.417 × (current weight/usual weight) × 100 [7].
The NRI allows the individualization of three sub-groups:
- Absence of undernutrition: > 97.5
- Moderate undernutrition: 83.5–97.5
- Severe malnutrition: < 83.5
NRI = 1.519 × albuminemia + 0.417 × (current weight/usual weight) × 100 [7].
The NRI allows the individualization of three sub-groups:
- Absence of undernutrition: > 97.5
- Moderate undernutrition: 83.5–97.5
- Severe malnutrition: < 83.5
The statistical analysis of the data was done using SPSS software version 20.0. The data was entered on EpiData 3.1. In all comparisons, the significance level was set to 0.05 (p < 0.05).
Results
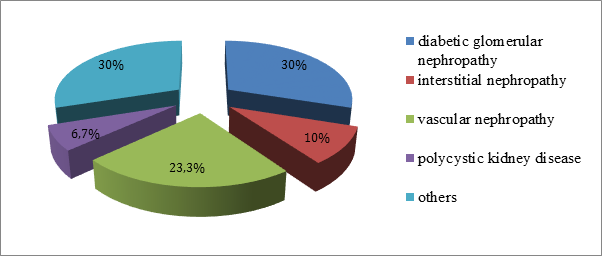
The average age of the patients was 48.5 ± 15.3 years with extremes ranging from 22 to 64 years with a sex ratio of 1. The mean age of hemodialysis was 3 ± 2.0 years with a minimum of 6 months and a maximum of 8 years. Diabetic glomerular nephropathy was the major cause of kidney disease (30%) (Figure 1).
Our patients had anorexia in 63.3% and complained of nausea and vomiting in 20 and 53.3%, respectively. More than half of the patients (56.7%) had an average daily energy intake < 20 kcal/kg/d. We noted that 93.3% of our population had insufficient average daily protein rations. The ratio of animal protein to vegetable protein is greater than 1 in 76.7% of the population. Micronutrient spontaneous intakes are shown in Table 1.
| Micronutrients | Average | Standard deviation |
| Sodium (mg/j) | 1037,8 | 443,7 |
| Potassium (mg/j) | 1884,1 | 954,1 |
| Phosphorus (mg/j) | 701,2 | 220,6 |
| Calcium (mg/j) | 506,3 | 456,9 |
| Magnesium (mg/j) | 192,3 | 63,9 |
| Iron (mg/j) | 5,0 | 1,7 |
| Vitamin B1 (mg/j) | 0,6 | 0,3 |
| Vitamin C (mg/j) | 91,4 | 94,7 |
| Vitamin B9 (µg/j) | 151 | 92,8 |
Table 1: Micronutrient intakes (minerals, trace elements and vitamins).
The frequency of undernutrition according to the different anthropometric parameters is shown in Figure 2. Hemoglobin averaged 9 ± 2.9 g/dl with extremes ranging from 8.1 to 14 g/dl. Mean CRP and cholesterol were 15.1 ± 6.3 mg/l and 0.9 ± 0.2 g/l, respectively. Albuminemia < 35 g/l was present in 36.6% of our population.
According to the NRI test, 60% of patients had a score < 97.5 of which 16.7% with a score < 83.5. Subsequently, we evaluated the spontaneous dietary intakes of the food survey according to the following parameters: age, sex, BMI, CB, albuminemia and CRP. The difference was statistically significant only for age, albuminemia and NRI (Tables 2, 3 and 4).
| Age (years) | [20-40] | [40-65] | P |
| Energy intake (kcal/d) | 1366,8 ± 442,1 | 1653,9 ± 473,1 | 0,131 |
| Energy ration (kcal/kg/d) | 21,12 ± 6,7 | 25,9 ± 9,2 | 0,178 |
| Protein ration (g/kg/d) | 0,5 ± 0,2 | 0,9 ± 0,4 | 0,01 |
| Protein intake (%) | 10,8 ± 3,8 | 13,1 ± 2,8 | 0,231 |
Table 2: Distribution of food survey data by age.
| Albuminemia (g/l) | < 30 | [30-35] | ≥ 35 | P |
| Energy intake (kcal/d) | 1481,3 ± 684,9 | 1502,3 ± 423,1 | 1588,3 ± 240,5 | 0,912 |
| Energy ration (kcal/kg/d) | 20,7 ± 6 | 27 ± 6,4 | 27,9 ± 15 | 0,322 |
| Protein ration (g/kg/d) | 0,7 ± 0,3 | 0,8 ± 0,3 | 1 ± 0,3 | 0,014 |
| Protein intake (%) | 9,8 ± 3,5 | 12,3 ± 2,2 | 13,3 ± 3,2 | 0,101 |
Table 3: Distribution of food survey data by albuminemia.
| NRI | < 83,5 | [83,5-97,5] | > 97,5 | P |
| Energy intake (kcal/d) | 1443,6 ± 538 | 1470 ± 369,4 | 1771,8 ± 460,2 | 0,391 |
| Energy ration (kcal/kg/j) | 19,2 ± 5,4 | 23,3 ± 7,5 | 32,8 ± 14 | 0,015 |
| Protein ration (g/kg/d) | 0,7 ± 0,3 | 0,7 ± 0,3 | 0,9 ± 0,6 | 0,665 |
| Protein intake (%) | 10,5 ± 3,4 | 12,3 ± 2,9 | 13,7 ± 3 | 0,152 |
Table 4: Distribution of food survey data by NRI.
Discussion
Malnutrition, in particular protein-energy malnutrition, is reported in 20-50% of patients treated with hemodialysis according to the diagnostic method used [8], hence the value of evaluating the nutritional status of these patients. As in the general population, evaluation of nutritional status requires the simultaneous use of several clinical, biological and technical markers. There is no single marker that provides a complete and reliable assessment of nutritional status. Assessment of nutritional status in chronic hemodialysis is difficult due to changes in hydration status and protein and carbohydrate metabolism secondary to renal insufficiency [9].
Food surveys are essential tools in nutrition assessment. It is currently recommended to calculate the ingesta absorbed by the patient for 3 days, which includes one day of dialysis, one day of non-dialysis and one day of weekend [10]. This is what was done in our study. More than half of our patients had an average daily energy intake < 20 kcal/kg/d. Similar results have been reported by other authors [11,12] with mean energy rations varying between 20 and 25 kcal/kg/d. As for the proteins, only 6.7% of our patients had satisfactory average daily protein rations. This is consistent with the multicenter study in Marrakech in 2012 [13], where chronic hemodialysis had an average protein intake of 0.9 ± 0.3 g/kg/day. Furthermore, we noted that the protein ration increases significantly (p = 0.01) with age: it is higher in the age groups of 40-65 years (0.8 ± 0.4 g/kg/day) compared to younger subjects (0.5 ± 0.2 g/kg/day). Dietary micronutrient evaluation revealed that our population had insufficient intakes of calcium, iron, vitamins B1 and B9, indicating the need for drug supplementation. These results are similar to those of Cano [12].
In addition to the food survey, it is also interesting to evaluate the appetite of chronic hemodialysis. Anorexia was noted in 63.3% of our patients. According to a Mauritanian study carried out in 2016 [14], anorexia was found in 59.4% of cases.
The anthropometric parameters are also valid and useful for evaluating the measurement of protein and energy status in dialysed patients. In order to limit artifacts associated with changes in moisture state, measurements should be collected at the end of the dialysis session [10]. In our series, the frequency of malnutrition varied according to the parameter used: 13.3% had a weight loss of more than 10% in the last 6 months, 46.7% had a BMI < 23 kg/m² and 40% had a BC < 22 cm. These results were similar to those of Belarbi., et al. [15], as well as Lemrabott., et al. [14].
The biological analysis in our patients had revealed 36.6% of undernutrition taking into account an albuminemia < 35 g/l, assayed by immunophlemetry. This is observed in most studies [13-15]. Moreover, the analytical study of our results noted that the mean protein ration decreases significantly (p = 0.014) with the decrease in albuminemia. However, the latter is influenced by inflammation, hydrosodic retention, proteinuria and hepatic disturbances. Pre-albuminemia has a short half-life of 2 days and is indicative of recent nutritional intakes. It is a biological marker of choice for the monitoring of renutrition, requiring a weekly dosage [16]. Currently, we do not have the dosage of pre-albuminemia within our hospitals.
Finally, the last criterion used for the nutritional evaluation of our chronic hemodialysis patients was NRI, which showed moderate undernutrition in 43.3% and severe malnutrition in 16.7%. Furthermore, we noted in our work that the mean energy ration increases significantly (p = 0.015) with the NRI score. Kobayashi., et al. [17] in 2010, found similar results to our results and also showed that NRI < 90 in hemodialysis patients was predictive of mortality.
All of these clinico-biological measures used in our study revealed that the frequency of undernutrition varied according to the parameter. In fact, the International Society of Nutrition and Metabolism in Renal Diseases [6] classifies protein energy depletion criteria into four groups: plasma biology, anthropometry, muscle mass and nutritional intakes. The Society defines undernutrition if at least one criterion is present on 3 groups. In the study by Pasian., et al. (2014) [18], for example, the rate of undernutrition was 69% in patients with chronic renal failure using the recommended criteria but without pre-albuminemia. In our work, it is not possible to group the criteria since there is a lack of an important measure which is the muscular mass. This emphasizes the importance of providing impedancemetrics in nephrology services to better assess the nutritional status of patients with renal insufficiency.
Conclusion
Our work emphasizes the need for multidisciplinary management of chronic hemodialysis patients: nephrologist, nutritionist and dietician. The diagnosis of undernutrition integrates the combination of several criteria: anthropometry, body composition, plasma biology and ingesta. Only one isolated parameter does not allow diagnosis.
References
- http://www.fondation-du-rein.org/assets/sites
- http://www.stn-nephro.org
- Pasian C., et al. “Dénutrition au cours des maladies rénales chroniques : techniques de renutrition et pratique de la nutrition artificielle". Néphrologie & Thérapeutique 12.7 (2016) 496-502.
- Chauveau P and Trolonge S. “Prise en charge nutritionnelle de l’insuffisance rénale". EMC - Endocrinologie-Nutrition 10.1 (2013): 1-6.
- Fouque D., et al. “EBPG guideline on nutrition". Nephrol Dial Transplant 22.2 (2007): 45-87.
- Fouque D., et al. “A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease". Kidney International 73.4 (2008): 391-398.
- Melchior JC. “Évaluation de l’état nutritionnel". EMC (Elsevier Masson SAS, Paris), Endocrinologie-Nutrition 10-379-A-10, (2009).
- Ministère de la Santé et des Sports, Société francophone nutrition clinique et métabolisme (SFNEP). Programme national Nutrition santé (PNNS). Dénutrition, une pathologie méconnue en société d’abondance; (2010).
- Nelson EE., et al. “Anthropometric norms for the dialysis population". American Journal of Kidney Diseases 16.1 (1990): 32-37.
- Azar R., et al. “Évaluation et suivi nutritionnels des patients hémodialysés". Néphrologie & Thérapeutique 5.5 (2009) : S317-S322.
- Sebbani M. “L’évaluation de l’état nutritionnel chez le dialysé chronique : A propos de 65 cas". Thèse de doctorat en médecine Fes (2011).
- Noel JM Cano. “French intradialytic evaluation study". Néphrologie & Thérapeutique 4.3 (2008):149-152.
- En-Nasria S., et al. “Apport des paramètres cliniques anthropométriques et l’enquête diététique dans l’évaluation de l’état nutritionnel des hémodialysés chroniques : étude multicentrique". Néphrologie & Thérapeutique 8 (2012) : 296-337.
- Lemrabott AT., et al. “Évaluation de l’état nutritionnel des hémodialysés chroniques du centre hospitalier national de Nouakchott". Néphrologie & Thérapeutique 12.5 (2016): 288-332.
- Belarbi M., et al. “Appétit et état nutritionnel des hémodialysés chroniques". Néphrologie & Thérapeutique 8 (2012): 296-337.
- Chertow GM., et al. “Prealbumin is as important as albumin in the nutritional assessment of hemodialysis patients". Kidney International - Journal 58.6 (2000): 2512-2517.
- Kobayashi I., et al. “Geriatric Nutritional Risk Index, a simplified nutritional screening index, is a significant predictor of mortality in chronic dialysis patients". Nephrol Dial Transplant 25.10 (2010): 3361-3365.
- Pasian C., et al. “Soin nutritionnel et amélioration clinique dans un service de néphrologie : une approche pilote multidisciplinaire". Néphrologie & Thérapeutique 10.4 (2014): 236-244.
Citation:
Nadia Ben Amor., et al. “Evaluation of the Nutritional Status of Hemodialysate Patients”. Nutrition and Food Toxicology 2.1
(2017): 255-261.
Copyright: © 2017 Nadia Ben Amor., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.