Research Article
Volume 3 Issue 2 - 2018
Fracture Resistance of a Fiber Reinforced Composite Substructure with Nanofilled Composite Overlay
1Lecturer, Conservative Dentistry & Endodontics, MGM Dental College & Hospital, Navi Mumbai, India
2MDS, Professor & Head, Department of Conservative Dentistry & Endodontics, Sinhgad Dental College & Hospital, Pune, India
2MDS, Professor & Head, Department of Conservative Dentistry & Endodontics, Sinhgad Dental College & Hospital, Pune, India
*Corresponding Author: Srinidhi Surya Raghavendra, MDS, Professor and Head, Department of Conservative Dentistry & Endodontics, Sinhgad Dental College & Hospital, Pune, India.
Received: April 24, 2018; Published: May 15, 2018
Abstract
Aim: To compare fracture resistance of a new fiber reinforced composite substructure (everX Posterior) and nanofilled composite (Solare X) when bonded to dentin substrate.
Method: Fifty extracted non restored human molars were collected and stored in thymol solution. Fifty dentin disks of 1mm thickness and 6mm diameter were prepared from these teeth. They were then subjected to decoronation and enamel from the crown was removed using diamond disks with water coolant. Bonding surfaces were ground flat within the limits of superficial dentin. Teflon cylinders of 4mm diameter and 4mm height were made for fiber reinforced composite substructure everX Posterior and a cylinder mold with diameter of 6mm and height of 6mm for the overlay of Solare X was prepared. Teflon cylinder of 6mm diameter and 6mm height was used for group I specimens to be built up with Solare X. Selected dentin disks were divided randomly in two groups:-
Group I (n=30): - 6mm x 6mm Solare X cylinders bonded to dentin disks.
Group II (n=30): - 6mm x 6mm Cylinders with everX Posterior core (4mm) and Solare X overlay bonded to dentin disks.
Group I (n=30): - 6mm x 6mm Solare X cylinders bonded to dentin disks.
Group II (n=30): - 6mm x 6mm Cylinders with everX Posterior core (4mm) and Solare X overlay bonded to dentin disks.
All the specimens were loaded until fracture with a universal testing machine using cross head speed of 1mm/min. Fracture resistance values of each group were noted. The results were tabulated and subjected to statistical analysis unpaired student t-test.
Results: Mean load and compressive strength values of Solare X was 1669.68N and 58.99 MPa and everX Posterior with overlay was 2374.51N and 89.95 MPa at p < 0.001 respectively.
Conclusion: everX Posterior and nanofilled composite creates a bilayered restoration that can withstand greater load of a restoration and holds promise for use as a core build up material in endodontically treated teeth.
Key words: Core buildup material; Fiber reinforced composite; Glass fibers; Nanofilled composite
Introduction
Restoration of extensively damaged crowns in endodontically treated teeth is a challenge [1]. These teeth are weakened by decreased or altered tooth structure which is attributed to caries and/or previous restorations, fracture or trauma, endodontic instrumentation and reduced moisture. Various treatment options for damaged posterior teeth after endodontic treatment are Amalgam restorations, Composite resin restorations, Composite resin onlay/overlay, Composite resin onlay/overlay (CAD-CAM), Ceramic onlay/overlay – lithium disilicate (pressed and CAD-CAM), Gold overlay, Metal–ceramics, Zirconia–ceramics, Monolithic zirconia crowns, Ceramic crown – lithium disilicate (pressed, layered and CAD-CAM) and Gold crowns [2].
Metal ceramic crowns cause more removal of healthy enamel and dentin as compared to partial noble metal crowns and inlays. Adhesively cemented ceramic inlays have been used as an alternative in order to minimize the removal of tooth structure. The greatest success using ceramic restorations has been limited to anterior teeth with porcelain veneers, whereas they have been used with less success for posterior teeth due to their inferior fracture resistance and abrasiveness when compared to that of gold alloys [1].
Composite resins were introduced in 1940’s to minimise the excess tooth preparation needed for other conventional restorative modalities. Various filler particles added in composites are quartz, heavy metal particles such as barium, strontium, zinc, aluminium or zirconium. Boron silicates and lithium aluminium silicates may also be added.
The filler particles used in composite resin have different chemical composition, morphology and dimensions. Dental composites popularly used for restorative purposes are hybrid and microfill types. Hybrids have intermediate esthetic properties but excellent mechanical properties due to the incorporation of fillers with different average particle sizes (15–20µm and 0.01–0.05µm). Microfilled composites were introduced to overcome the problems of poor esthetic properties, especially in anterior teeth. They have colloidal silica (around 50% in volume) with an average particle size of 0.02µm and a range of 0.01–0.05 µm. Nanocomposites are characterised by nanoparticles measuring approximately 25nm and nanoaggregates of approximately 75nm, which are made up of zirconium/silica or nanosilica particles. The aggregates are treated with silane so that they bind to the resin [3]. The distribution of the filler (aggregates and nanoparticles) gives a high load, up to 79.5% [3]. Nanocomposites are claimed to combine the good mechanical strength of hybrids3 and the superior polish of the microfills [4]. Advantages of nanocomposites apart from good mechanical strength are lesser shrinkage, cusp wall deflection, marginal leakage, colour changes, bacterial penetration and post-operative sensitivity due to lower particle size which effectively reduces the presence of microfissures in the enamel edges [5]. Solare X (GC India, Telangana, India) is an example of a nanofilled composite.
To overcome the shortcoming of reduced strength, glass fibres were added to the resin and these Fiber-reinforced composites (FRCs) were indicated for use in posterior teeth. Studies have shown FRCs to have superior physical properties. These are due to fiber volume fraction, fiber adhesion to the resin matrix, water sorption of the resin matrix and fiber orientation [6]. Hence when a FRC substructure is used under particulate filled composite, the static load-bearing capacity of the material combination could be theoretically improved [7]. Ever X Posterior contains optimally sized combination of e glass fibres and barium glass fillers inside a polymer matrix. Hence it is claimed to have higher fracture toughness than collagen reinforced dentin.
The aim of this study was to compare fracture resistance of a new fiber reinforced composite substructure (everX Posterior) and nanofilled composites (Solare X) when bonded to dentin substrate.
Materials and Method
Fifty extracted non restored human molars were collected from the Department of Oral and Maxillofacial Surgery. The inclusion criteria were that the teeth should be free of visible caries and restorations and should have been extracted due to periodontal reasons. The exclusion criteria were that the teeth should not have visible pulp exposure or cracks.
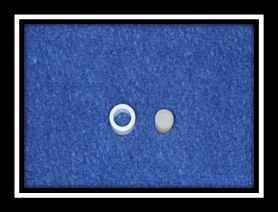
Adhering soft tissue and blood was removed under running water and teeth were stored in thymol solution. Fifty dentin disks of 1mm thickness and 6mm diameter were prepared from these teeth in the following manner. Initially, the teeth were subjected to decoronation with high speed rotary instruments. After decoronation, enamel from the crown was removed using diamond disks with water coolant. Bonding surfaces were ground flat within the limits of superficial dentin (Figure 1). Teflon cylinders of 4mm diameter and 4mm height were made for fiber reinforced composite substructure everX Posterior (GC India, Batch No: 1310011) (Figure 2a). A cylinder mold with diameter of 6mm and height of 6mm for the overlay of Solare X (GC India, Batch No: 1410313) was prepared. Teflon cylinder of 6mm diameter and 6mm height was used for group I specimens to be built up with Solare X (Figure 2b).

Figure 1b: 6mm x 6mm Cylinders with everX Posterior
core (4 mm) and Solare X overlay bonded to dentin disks.
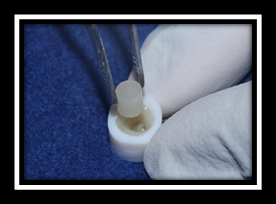
Figure 2: Composite build up done in group II with everX
as substructure and Solare X overlay in cylinders - specimen
measuring 4mm height and 4 mm diameter.
Selected dentin disks were divided randomly in two groups:-
Group I (n=30): - 6mm x 6mm Solare X cylinders bonded to dentin disks.
Group II (n=30): - 6mm x 6mm Cylinders with everX Posterior core (4mm) and Solare X overlay bonded to dentin disks.
Group I (n=30): - 6mm x 6mm Solare X cylinders bonded to dentin disks.
Group II (n=30): - 6mm x 6mm Cylinders with everX Posterior core (4mm) and Solare X overlay bonded to dentin disks.
In group I, the composite build up was done on dentin disks using Solare X. Each increment was 2mm thick. The standard adhesive technique used included acid etching which was carried out using 37% phosphoric acid followed by bonding using 5th gen single bottle adhesive system Tetric Bond (Ivoclar Vivadent, India). The cylinders thus obtained measured 6mm thickness and 6mm height.
In group II, the composite build up was done with everX Posterior as substructure. It was cured in increments, each one measuring 2mm thick. The standard adhesive technique used included acid etching which was carried out using 37% phosphoric acid followed by bonding using Tetric Bond to get composite cylinder specimens measuring 4mm height and 4mm diameter. These specimens were retrieved and placed inside cylinders measuring 6mm height and 6mm diameter on dentin disk. Solare X was used as an overlay and packed within the gap between everX specimen and Teflon molds. This arrangement was then cured for 20 seconds and retrieved (Figure 3). All the specimens were loaded until fracture with a universal testing machine using cross head speed of 1mm/min. Fracture resistance values of each group were noted. The results were tabulated and subjected to statistical analysis unpaired student t-test.
Results
Mean load values of group 1 (Nanofilled composite – Solare X) was 1669.68N. Mean load values of group II (everX + Solare X overlay) was 2374.51N. P- value was found out to p < 0.001 when confidence limit was kept as 99%, hence the results were statistically significant (Students t test – unpaired). [Table 1] Mean compressive strength values of group 1 (Nanofilled composite – Solare X) was 58.99Mpa. Mean compressive strength values of group II (everX Posterior + Solare X) was 89.95Mpa. P- value was found out to p < 0.001 when confidence limit was kept as 99%, hence the results were statistically significant (Students t test – unpaired). [Table 2]
| Group | Total No | Mean (SD) |
| Group 1 | 30 | 1669.68 (367.1) |
| Group 2 | 30 | 2374.51 (152.3) |
| t value | - | 9.713 |
| P value | - | <0.001** |
(p < 0.05 - Significant*, p < 0.001 - Highly significant**)
Table 1: Comparison of Mean (SD) values (Load) of both the groups.
Table 1: Comparison of Mean (SD) values (Load) of both the groups.
| Group | Total No | Mean (SD) |
| Group 1 | 30 | 58.99 (12.9) |
| Group 2 | 30 | 83.95 (5.4) |
| t value | - | 9.736 |
| P value | - | <0.001** |
(p < 0.05 - Significant*, p < 0.001 - Highly significant**)
Table 2: Comparison of Mean (SD) values (Compressive strength) of both the groups.
Table 2: Comparison of Mean (SD) values (Compressive strength) of both the groups.
Discussion
Filler particles are most commonly produced by grinding or milling quartz or glasses to produce particles ranging in size from 0.1–100 mm [8]. Types of fillers are Macro fillers -- 10 to 100 microns, Midi fillers -- 1 to 10 microns, Mini fillers -- 0.1 to 1 micron, Micro fillers -- 0.01 to 0.1 micron and Nano fillers -- 0.005 to 0.01 micron [8]. A newer type of classification introduces the Hybrid large particle (1-20 mm glass, 0.04 mm silica), Hybrid midifiller 0.1-10 mm glass, 0.04 mm silica) and the Hybrid minifiller/Small Particle Filled (0.1-2 mm glass, 0.04 mm silica). Also there is the Packable hybrid which is a Midifiller/minifiller, but with lower filler fraction and the Flowable hybrid which is a Midifiller hybrid, but with finer particle size distribution [9].
Filler particles vary from material to material but may be colloidal silica, barium silicate, strontium/borosilicate glass, quartz, zinc silicate, or lithium aluminum silicate. Filler size and loading are associated with three trends in composite resin performance:
- The ability to polish increases as filler particle size decreases.
- Wear resistance improves as filler particle size decreases.
- Fracture durability generally increases as the percent of inorganic filler loading by volume increases.
With the improvements in the mechanical properties of Particle Filled Composites (PFCs), their use has been widened not only to the posterior intra-coronal area, but also to extra-coronal restorations. However, further improvements are needed in order to extend the use of PFC to high stress-bearing applications such as direct posterior restorations involving cusps and indirect restoration, inlays and onlays [10]. The most common problems that occurred were various types of fractures in high stress-bearing areas [11].
During setting of the resin composites the polymerization shrinkage induces contraction stress. One of the factors responsible to reduce the magnitude of contraction stress has been filler load. Hence to increase the filler load, concept of implementation of nanoparticle technology into restorative materials came into existence. Based on definition of “nanoscale bulk technology”, new classes of dental composites, so called nanocomposites, have been developed and marketed during recent years. Nanocomposites are claimed to combine the good mechanical strength of hybrids and the superior polish of the microfills. Other positive features reported are high wear resistance, improved optical characteristics and reduced polymerization shrinkage [12]. Nanotechnology has enabled the production of nano-dimensional filler particles [13], which are added either singly or as nanoclusters into composite resins. Nanocomposites retain their smoothness for a longer time [14] and help in the generation of more esthetic restorations as the fillers have higher translucence since they are smaller than the wavelength of light. Solare X used in this study is a nanofilled PFC.
Over the past 25 years, a new class of materials designed for reinforcing dental resins has been introduced. These products are fiber-reinforcing ropes, braids, ribbons, and bundled fibers [15]. Kangasniemi., et al. in 2003 stated that out of several different types of fiber reinforcement materials, kevlar, carbon, glass, ultra-high-molecular- weight polyethylene (UHMWPE), and silane-treated glass have been used to provide fiber reinforcement [16]. Samadzadeh A., et al. in 1997 stated that the lock-stitch weave of the UHMWPE that allows the ribbon to maintain a structural integrity by minimizing weave and fabric shifting within the composite [17]. According to Karbhari., et al. [18] and Ramos., et al. [19] in 1996 it imparts a multidirectional reinforcement to restorative polymeric resins that acts in stopping crack propagation.
The endodontic treatment of pulpless teeth results in loss of moisture and loss of tooth structure which results in reduced mechanical strength [20]. Fibres in dentine give the tooth much higher fracture toughness. Enamel is predominately crystalline and densely packed and gives high strength and excess periods after surface hardness. Hence cracks within the teeth do not usually progress all the way. Modern composites and indirect materials offer perfect features for enamel replacement namely high wear resistance and aesthetics. However, they are not able to equal dentine when it comes to resistance to fracture [20].
In the present study, everX Posterior was selected as core build up material beneath conventional posterior composite to create a strong, bilayered direct restorative solution. Ever X Posterior gives maximum strength, features the optimum size and combination of e-glass fibres and barium glass fillers, within a tough polymer matrix. The short fibres used in ever X Posterior provide fracture toughness greater than collagen-reinforced dentine and almost double that of conventional composite. When everX Posterior is used as a substructure under conventional composite, not only is strength significantly improved, but also the fracture pattern under load is changed. If the restoration is loaded till failure, the path of a fracture changes and is deflected away from the roots [21].
The results in the table 4 shows mean compressive strength values of group I (Solare X) = 58.99mpa and that of group II (everX + Solare X) = 83.95mpa, the p value being <0.001 showing highly significant statistical difference. It can thus be concluded that when everX Posterior is used as a substructure followed by nanofilled composite (Solare X) as overlay, the combination required greater load to fracture as compared to Solare X alone. The possible reasons could be -
- The fibres in everX Posterior increase the adhesion to overlying composite by providing added mechanical retention.
- Fibres orient into a horizontal plane within the cavity. Due to the strong adhesion between resin and silanated fibres in everX Posterior, the direction of the fibres minimizes shrinkage in the horizontal plane after placement [22].
- Short fibres prevent fracture propagation in fillings and tooth structure [23].
- Reliable bond to any overlaying composite as well as to the tooth substance [23].
Conclusion
The synergistic effect of everX Posterior and nanofilled composite creates a bilayered restoration that can withstand greater load of a restoration made from conventional composite alone. Load bearing capacity of everX Posterior substructure with nanofilled composite overlay holds promise for use as a core build up material in endodontically treated teeth.
References
- Ilday N., et al. “Fracture resistance of molars with different direct cuspal coverage restorations”. International Journal of Current Research 5.4 (2013): 807-810.
- Kumar G and Shivrayan A. “Comparative study of mechanical properties of direct core buildup materials”. Contemporary Clinical Dentistry 6.1 (2015): 16-20.
- Suzuki T., et al. “Resistance of nanofill and nanohybrid resin composites to toothbrush abrasion with calcium carbonate slurry”. Dental Materials 28.6 (2009): 708–716.
- Banerji B and Mehta SB. “The finishing and polishing of resin composite restorations”. In Practical Procedures in Aesthetic Dentistry (eds S. Banerji, S. B. Mehta and C. C. Ho), Wiley Publishing, Noida, India, 1st ed. (2017).
- Simi B and Suprabha BS. “Evaluation of microleakage in posterior nanocomposite restorations with adhesive liners”. Journal of Conservative Dentistry 14.2 (2011): 178-181.
- Mosharraf R and Givechian P. “Effect of fiber position and orientation on flexural strength of fiber reinforced composite”. Journal of Islamic Dental Association of Iran 24.2 (2012): 21-27.
- Taher NA. “Bi-axial Flexural strength of dual-polymerizing agents cemented to human dentin after photo-activation with different light-curing systems”. Saudi Dental Journal 22.3 (2010): 107–112.
- Hambire UV and Tripathi VK. “Experimental evaluation of different fillers in dental composites in terms of mechanical properties”. ARPN Journal of Engineering and Applied Sciences (2012): 147- 151.
- Rawls HR and Esquivel- Upshaw JF. Restorative Resins. Anusavice in Phillips' Science of Dental Materials (eds Anusavice K, Shen C, Rawls RH). Missouri: Saunders; 12th ed (2012).
- Garoushi SK., et al. “Fiber-reinforced composite substructure: Load-bearing capacity of an onlay restoration”. Acta Odontol Scandinavia 64.5 (2006): 281-285.
- Nagas E., et al. “Bond strength of fiber posts and short fiber reinforced composite to root canal dentin following cyclic loading”. Journal of Adhesion Science and Technology 31.13 (2016): 1397-1407.
- Dyer SR., et al. “Effect of fiber position and orientation on fracture load of fiber-reinforced composite”. Dental Materials 20.10 (2004): 947–955.
- Yadav RD., et al. “A comparative analysis of different finishing and polishing devices on nanofilled, microfilled and hybrid composite”. International Journal of Clinical Pediatric Dentistry 9.3 (2016): 201-208.
- Yesil ZD., et al. “Evaluation of the wear resistance of new nanocomposite resin restorative materials”. Journal of Prosthetic Dentistry 99.6 (2008): 435- 443.
- Strassler HE. “Fiber-reinforcing materials for dental resins”. Inside Dentistry 4.5 (2008): 2-8.
- Kangasniemi I., et al. “Consensus statement of fiber-reinforced polymers: current status, future directions, and how they can be used to enhance dental care”. The International Journal of Prosthodontics 16.2 (2003): 209.
- Natarajan P and Thulasingam C. “The effect of glass and polyethylene fiber reinforcement on flexural strength of provisional restorative resins: an in vitro study”. Journal of Indian Prosthodontic Society 13.4 (2013): 421-427.
- Karbhari VM and Strassler HE. “Effect of fiber architecture on flexural characteristics and fracture of fiber reinforced composites”. Dental Materials 23.8 (2007): 960-968.
- Spyrides SMM., et al. “Effect of plasma and fiber position on flexural properties of a polyethylene fiber reinforced composite”. Brazilian Dental Journal 26.5 (2015): 490-496.
- Dammaschke T., et al. “Long-term survival of root canal treated teeth: a retrospective study over 10 years”. Journal of Endodontics 29.10 (2003): 638–643.
- Abouelleil H., et al. “Comparison of mechanical properties of a new fiber reinforced composite and bulk filling composites”. Restorative Dentistry & Endodontics 40.4 (2015): 262-270.
- Garoushi SK., et al. “Physical properties and depth of cure of a new short fibre reinforced composite”. Dental Materials 29.8 (2013): 835-841.
- Garoushi SK., et al. “The effect of short fiber composite base on microleakage and load bearing capacity of posterior restorations”. Acta Biomaterialia Odontologica Scandinavica 14.1-1 (2015): 6-12.
Citation:
Jimish Shah and Srinidhi Surya Raghavendra. “Fracture Resistance of a Fiber Reinforced Composite Substructure with
Nanofilled Composite Overlay”. Oral Health and Dentistry 3.2 (2018): 567-573.
Copyright: © 2018 Jimish Shah and Srinidhi Surya Raghavendra. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.