Research Article
Volume 1 Issue 1 - 2017
Prevalence and surgical outcome of congenital lacrimal fistulas in Guatemala
1Ophthalmology surgeon, Rodolfo Robles Valverde Hospital, Guatemala, Guatemala.
2Rodolfo Robles Valverde Hospital, Guatemala, Guatemala.
3Rodolfo Robles Valverde Hospital.
2Rodolfo Robles Valverde Hospital, Guatemala, Guatemala.
3Rodolfo Robles Valverde Hospital.
*Corresponding Author: León-Nieto L, Ophthalmology surgeon, Rodolfo Robles Valverde Hospital, Guatemala, Guatemala, Mexico.
Received: March 21, 2017; Published: April 03, 2017
Abstract
Background: The purpose of this study was to review the prevalence, surgical techniques and outcome of congenital lacrimal fistulas performed over a 10-year period in Rodolfo Robles hospital, in Guatemala.
Method: The medical records of all patients presenting congenital lacrimal fistulas between December 2006 and November 2016 were collected and analyzed. Recorded data included demographic features, associated abnormalities of the lacrimal outflow pathway, type of surgical intervention, outcome and complications. Patients with acquired lacrimal fistulas were excluded.
Results: Twenty-nine eyes out of twenty-eight patients that underwent surgical treatment for correcting symptomatic congenital lacrimal fistulas were identified. Sixteen patients (57%) were males and twelve patients (43%) were females. The predominant symptom was epiphora. The most common site of the fistulas was the inferior medial canthal area. This area was connected to the lacrimal sac in 90% of the cases and to the common canaliculus in 10%. The functional success rate was 96.5% after surgical treatment.
Conclusion: Congenital lacrimal fistulas may be successfully treated excising the anomalous tissue (fistulectomy) and managing the lacrimal pathway according to the age of the patient and the presence or absence of obstruction.
Keywords: Congenital lacrimal; fistula; prevalence; surgical outcome
Introduction
The normal development of the nasolacrimal system begins around day 32 of gestation as a thickening of the ectoderm at the level of the naso-optic fistula, between the maxillary and nasal bones. The excretory system begins its development in the 7 mm embryo, when a depression termed the naso-optic fissure starts to develop bordered superiorly by the lateral nasal process and inferiorly by the maxillary process. The naso-optic fissure gradually shallows as the structures bordering it grow and coalesce. A solid strand of surface epithelium thickens along the floor of the rudimentary fissure extending from the orbit to the nose. The thickened cord of epithelium becomes buried to form a rod connected to the surface epithelium at only the orbital and nasal ends. The superior end of the rod enlarges to form the lacrimal sac, and gives off two columns of cells that grow into the eyelid margins to become the canaliculi. The superior membrane at the puncta is usually completely canalized when the eyelids separate at 7 months of gestation, and therefore is normally patent by birth. [1, 2, 3, 4]
Since tear production does not begin until a week after birth, epiphora may not be present at birth even in cases of nasolacrimal duct obstruction. [6] Persistent epiphora is considered pathological three months after birth. Both lacrimal points are located 5-6 mm laterally from the inner edge of the palpebral border. Each tear point opens to a lacrimal canaliculus which, after a vertical course of 2mm, becomes horizontal, with a path of 7-8 mm which, in 90% of cases, flows into the common canaliculus. [5, 12]
Congenital sac fistulas are estimated to occur in 1 per 2000 births. It consists of an epithelial fistulous tract that goes from the lacrimal sac or common canaliculus and opens at the skin located inferonasal to the medial cantal angle. The patients may be asymptomatic and overlooked for some time after birth, or may demonstrate tearing from the fistula, the eye, or both. [4]
Most of the time it is unilateral (94% of cases) and may be associated with other malformations of the lacrimal apparatus, such as canalicular agenesis, absence of the superior lacrimal punctum or absence of the entire lacrimal system. [4,7,11]
Fistulas require correction if they are associated with epiphora, recurrent conjunctivitis or dacryocystitis. Treatment involves excision of the epithelial tract and its closure. In cases where there is obstruction of the associated lacrimal duct, excision of the fistula is combined with a procedure to resolve such obstruction according to the age of the patient. There are some authors who suggest performing this procedure in conjunction with a dacryocystorhinostomy at any time. [8, 9, 10, 13]
Congenital lacrimal fistula is a rare developmental abnormality and the available information concerning the epidemiology and prevalence in Central America is scarce. We present the first series of patients with congenital lacrimal fistula in Guatemala. The results of the surgical techniques and outcome are presented and discussed.
Design
Retrospective descriptive study.
Methods
The study was carried out in the Oculoplastic Clinic of Rodolfo Robles Valverde Hospital in Guatemala, between December 2006 and November 2016. The information was extracted from the clinical records of all patients that underwent surgical intervention for congenital lacrimal fistula in one or both eyes, of any gender, race, age, and who had never been treated before. Patients with secondary or acquired fistulas were excluded. Recorded data included demographic features, associated abnormalities of the lacrimal outflow pathway, the type of surgical intervention and outcome. The study was conducted on a single center and was approved by the local institutional review board.
All patients underwent a routine ophthalmologic examination for diagnosis. Because all of the twenty-eight patients were children, surgery was done under general anesthesia and trans-operatory syringing of the lacrimal pathway for diagnosis was performed to evaluate the patency of the drainage system. Ten patients had nasolacrimal duct obstruction.
The treatment was simple fistula excision (closed fistula excision) in nineteen cases with patent nasolacrimal canal; fistula excision with nasolacrimal duct intubation in six children younger than five years of age; and fistula excision with dacryocystorhinostomy in four patients older than five years with nasolacrimal duct obstruction.
The closed fistula excision was done in nineteen cases. The fistula tract was dissected entirely by an incision surrounding the fistula and excised out. The root of the fistula in the lacrimal sac was sutured with a 6-0 Vicryl suture. After closure of subcutaneous and cutaneous tissues, probing and irrigation were done to ensure the nasolacrimal passage was patent.
The dacryocystorhinostomy incision was made vertically 8-12 mm medially to the medial canthus surrounding the inferior orbital rim. The periosteum was separated from the lacrimal bone and an 8 x 8 mm osteotomy, including the anterior lacrimal crest, was opened with a Kerrison rongeurs. A Bowman probe was inserted from the fistula and passed through the lacrimal sac to establish the origin of the lacrimal fistula. The fistula tract was then dissected from the surrounding tissues under the guidance of the lacrimal probe within the tract. In seventeen patients the origin of the fistula was connected to the lacrimal sac and we closed with a 6-0 Vicryl suture and excised the stump. In two cases the fistula opened to the common canaliculi. The medial wall of the lacrimal sac was incised to form the anterior flap. The posterior nasal mucosal flap was also formed by a horizontal incision. After dilatation of both puncti a silicone tube was passed through the lacrimal sac and its ends were tied together and left in the nose cavity. Then the flaps were sutured to each other and anastomosed. Subcutaneous and cutaneous tissues were closed in the usual fashion.
Results
Demographic Profile
The information from the clinical records of twenty-eight patients that underwent twenty-nine surgical procedures for congenital lacrimal fistulas (one case of bilateral fistula) and who fulfill the inclusion / exclusion criteria, was summarized and analyzed.
The information from the clinical records of twenty-eight patients that underwent twenty-nine surgical procedures for congenital lacrimal fistulas (one case of bilateral fistula) and who fulfill the inclusion / exclusion criteria, was summarized and analyzed.
Eleven of these patients presented the symptoms since birth (39%). Parents referred epiphora or tearing through the opening of the fistula. Patients were between 1 and 12 years old (mean 5.4) at the time of surgery and none of the patients were asymptomatic at presentation, although symptoms were not always directly attributable to the fistula itself. No family history of lacrimal abnormalities was reported amongst the patients.
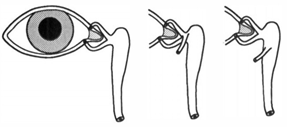
Sixteen patients (57%) were male and twelve (43%) were female. The fistula was on the right side in thirteen cases, on the left in fourteen and one was bilateral. The description of the origin and path of the fistula was described only in 65.5% of the surgical records. Of these, seventeen (89.47%) came from the sac and two (10.52%) from the common canaliculus (Figure.1).
Figure 1: Diagramatic representation of normal anatomy (left), fistula arising from the common canaliculus (center) and from the lacrimal sac (right).
Some of the patients had associated lacrimal anomalies. One case had superior lacrimal punctum agenesis. Ten patients presented partial or complete nasolacrimal obstruction on the same side of the fistula.
The selection of the type of surgery was based on the age of the patient and the presence or absence of obstruction in the nasolacrimal system. The clinical features and type of surgical treatment are shown in Table 1.
| Case No. | Sex | Age | Eye | Syringing | Surgical procedure | Origin |
| 1 | F | 6 | Left | Open | Isolated excision of the fistula | - |
| 2 | M | 3 | Left | - | Isolated excision of the fistula | - |
| 3 | F | 8 | Left | - | Isolated excision of the fistula | Lacrimal sac |
| 4 | F | 8 | Right | - | Isolated excision of the fistula | Lacrimal sac |
| 5 | M | 11 | Right | - | Isolated excision of the fistula | - |
| 6 | F | 1 | Left | - | Isolated excision of the fistula | Lacrimal sac |
| 7 | M | 7 | Left | Open | Isolated excision of the fistula | Lacrimal sac |
| 8 | M | 2 | Right | Duct obstruction | Fistula excision and DCR | Lacrimal sac |
| 9 | F | 4 | Right | Duct obstruction | Fistula excision and DCR | - |
| 4 | Left | Duct obstruction | Fistula excision and DCR | Lacrimal sac | ||
| 10 | F | 12 | Left | - | Isolated excision of the fistula | |
| 11 | M | 12 | Right | Open | Isolated excision of the fistula | Lacrimal sac |
| 12 | M | 1 | Right | - | Isolated excision of the fistula | Lacrimal sac |
| 13 | F | 2 | Right | - | Isolated excision of the fistula | Lacrimal sac |
| 14 | F | 3 | Left | Duct obstruction | Fistula excision with nasolacrimal intubation | Lacrimal sac |
| 15 | M | 5 | Left | - | Isolated excision of the fistula | Common canaliculi |
| 16 | M | 5 | Left | - | Isolated excision of the fistula | Common canaliculi |
| 17 | M | 2 | Right | - | Isolated excision of the fistula | - |
| 18 | M | 4 | Left | Open | Isolated excision of the fistula | - |
| 19 | F | 4 | Right | Duct obstruction | Fistula excision with nasolacrimal intubation | Lacrimal sac |
| 20 | M | 5 | Right | Duct obstruction | Fistula excision and DCR | - |
| 21 | F | 11 | Right | - | Isolated excision of the fistula | - |
| 22 | M | 12 | Left | Duct obstruction | Fistula excision with nasolacrimal intubation | Lacrimal sac |
| 23 | F | 11 | Left | - | Isolated excision of the fistula | Lacrimal sac |
| 24 | M | 1 | Left | Duct obstruction | Fistula excision with nasolacrimal intubation | Lacrimal sac |
| 25 | M | 5 | Right | - | Isolated excision of the fistula | - |
| 26 | M | 3 | Right | - | Isolated excision of the fistula | Lacrimal sac |
| 27 | M | 4 | Left | Duct obstruction | Fistula excision with nasolacrimal intubation | Lacrimal sac |
| 28 | F | 4 | Right | Duct obstruction | Fistula excision with nasolacrimal intubation | Lacrimal sac |
Percentages are row percentage.
Table 1: Clinical findings and surgical treatment of the patients with congenital lacrimal fistula
Table 1: Clinical findings and surgical treatment of the patients with congenital lacrimal fistula
An isolated fistulectomy technique, as indicated by the literature, was performed in nineteen patients (65.5%) who presented adequate permeability of the lacrimal duct. The success rate of closing the fistula at the first attempt was 100%.
Six patients under 5 years old, who presented obstruction of the lacrimal pathway, underwent excision of the fistula with nasolacrimal intubation for six months. Two months after surgery, one of these patients had recurrence of the fistula with tearing and mucous discharge through the fistulous opening.
Four patients older than 5 years old with congenital fistula and associated lacrimal obstruction, had fistula excision and dacryocystothinostomy. The functional success rate was 100%.
The postoperative complications include recurrence of the fistula in one case, and extrusion of the silicone tube in another patient, before it was removed by the surgeon four months after surgery.
Surgical outcomes are summarized in Table 2.
| Procedure | Eyes treated | % Success rate |
| Isolated excision of the fistula | 19 | 100 |
| Fistula excision with nasolacrimal intubation | 6 | 83.33 |
| Fistula excision and DCR | 4 | 100 |
Table 2: Surgical success rate.
Discussion
Congenital lacrimal sac fistulas are uncommon developmental anomalies. Its incidence is reported to be 1 in 2000 births [15], but the limited number of reports suggests an even lower incidence. Embryologically, the nasolacrimal system arrives from a cord of the surface ectoderm. Invagination occurs between the maxillary and frontonasal processes, forming the nasolacrimal system. Canalization of the buried ectodermal cord occurs along the length of the lacrimal system and, if incomplete separation occurs, supernumerary punctae and canaliculi can occur. The exact etiopathogenesis is unknown but mostly believed to be an accessory out-budding from the lacrimal drainage system during embryogenesis. [16,17]
As indicated by literature, our study evidence that there is no sex predominance, that most of the cases are unilateral and that the origin of the fistula comes mainly from the sac in almost 90%. [22] There is no agreement on the treatment for congenital lacrimal fistula. Cauterization and simple skin closure have not been successful. On the other hand, the closed excision in which only the fistula is repaired, DCR with fistula excision, and fistula excision with nasolacrimal intubation are reported to be successful. [18,19,20,21] In our study, all the cases received surgical treatment and the success rate for functional resolution after the first surgical attempt was 96.5%.
To avoid complications, some authors consider that fistula excision with DCR facilitates surgical dissection and removal of the fistula from its origin, minimizing the risk of damaging the common canaliculus. Others favor a fistulectomy accompanied by nasolacrimal intubation because it is safer. [19,21] In our experience, only one patient had a recurrence two months after being operated by fistula excision with nasolacrimal intubation and needed a second procedure. Another patient extruded the tube before being withdrawn at the clinic by the surgeon.
Some malformations of the lacrimal apparatus have been reported to be associated with lacrimal fistula. [4,7,11] One of our patients showed agenesis of the superior lacrimal punctum.
Conclusion
The overall functional success rate after surgery was 96.5%. We believe that congenital lacrimal fistulas can be treated with simple excision alone in most cases. Adjunctive DCR or nasolacrimal intubation must be reserved for those associated with obstruction of the lacrimal pathway.
Acknowledgements
Special thanks to Dr. Mario Cahueque for his unconditional support in the realization of this article
Special thanks to Dr. Mario Cahueque for his unconditional support in the realization of this article
References
- Cassady JV. “Developmental anatomy of nasolacrimal duct”. Archives of ophthalmology 47 (1952) 141-158.
- Francois J and Bacskulin J. “External congenital fistulae of the lacrimal sac”. Ophtalmologica 159.4 (1969): 249-261.
- AJ Cohen. “The Lacrimal System: Diagnosis, Management, and Surgery, Second Edition, Springer International Publishing Switzerland 2015.
- Muruku-del-Castillo. “Developmental of the lacrimal apparatus. In Milden B Weil B (Eds). The lacrimal system”. Appleton-Century-Crofts, Norwalks, Conneticut (1983): 9-22.
- Barceló A and Hueso J R. “Actualización en cirugía oftálmica pediátrica 2009, cap 05. Patología lagrimal en la infancia (2009): 84-95.
- Nelson LB. “Disorders of lacrimal apparatus in infancy and childhood”. Harley Pediatric Ophthalmology 4th Edition (1998): 345-352.
- Bowling BS and Chandna A. “Superior lacrimal canalicular atresia and nasolacrimal duct obstruction in the CHARGE association”. Journal of Pediatric Ophthalmology and Strabismus 31.5 (1994): 336-337.
- Ugurbas SH and Zilelioglu G. “Congenital lacrimal fistula”. European Journal of Ophthalmology 10.1 (2000): 22-26.
- Welham RA and Hughes SM. “Lacrimal surgery in children”. American Journal of Ophthalmology 99.1 (1985): 27-34.
- Paul TO and Shepherd R. “Congenital nasolacrimal duct obstruction: natural history and the timing of optimal intervention”. Journal of Pediatric Ophthalmology and Strabismus 31.6 (1994): 362-367.
- Lyons CJ., et al. “The management of punctal agenesis”. Ophthalmology100.12 (1993): 1851-1855.
- Busse H. “Connatal dacryostenoses. Clinical picture and treatment”. Ophthalmologe101.9 (2004): 945-956.
- Mrugacz M., et al. “Treatment of nasolacrimal duct obstruction with probing in children younger than 4 years”. Klin Oczna 112.7-9 (2010): 221-222.
- Komínek P., et al. “Monocanalicular versus bicanalicular intubation in the treatment of congenital nasolacrimal duct obstruction”. Graefe's Archive for Clinical and Experimental Ophthalmology 249.11 (2011): 1729-1733.
- Lim CS., et al. “Nasolacrimal duct obstruction in children: outcome of intubation”. Journal of AAPOS 8.5 (2004): 466-472.
- Buerger DG., et al. “Congenital lacrimal disorders. In: Nesi FA, Lisman RD, Levine MR, eds. Smith's” Ophthalmic Plastic and Reconstructive Surgery. 2nd ed. St Louis: Mosby; 1998
- Zhuang L., et al. “Bilateral congenital lacrimal fistulae: a case report and review of the literature”. Laryngoscope120 suppl 4 (2010): S230.
- Welham RAN., et al. “Congenital lacrimal fistula”. Eye 10.1 (1992): 211-214.
- Sullivan TJ., et al. “The surgical management of congenital lacrimal fistulae”. Australian and New Zealand Journal of Ophthalmology 20.2 (1992): 109-114.
- Erdem E., et al. “Doğumsal nazolakrimal kanal tıkanıklığında sondalama zamanı”. T Oft Gaz 38 (2008): 180-184.
- Birchansky LD., et al. “Management of congenital lacrimal sac fistula”. Archives of ophthalmology 98.10 (1990): 388-390.
- Jia Quan Chaung., et al. “Congenital lacrimal fistula: A major review. Orbit35.4 (2016): 212-220.
Citation:
León-Nieto L. “Prevalence and surgical outcome of congenital lacrimal fistulas in Guatemala”. Ophthalmology and Vision Science 1.1 (2017): 17-23.
Copyright: © 2017 León-Nieto L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.