Research Article
Volume 1 Issue 5 - 2018
Epidemiological Profile of Patients Registered in the Brazilian Glaucoma Carrier Attention Program from A Tertiary Eye Care Reference Center
1Medicine College, Universidade Federal de Rondonia, Porto Velho, Brazil
2Glaucoma and Cataract Reference Center, Santa Casa de Belo Horizonte, Belo Horizonte, Brazil
3Department of Ophthalmology, Santa Casa de Belo Horizonte, Belo Horizonte, Brazil
2Glaucoma and Cataract Reference Center, Santa Casa de Belo Horizonte, Belo Horizonte, Brazil
3Department of Ophthalmology, Santa Casa de Belo Horizonte, Belo Horizonte, Brazil
*Corresponding Author: Hévila Rolim, Medicine College, Universidade Federal de Rondonia, Porto Velho, Brazil.
Received: January 13, 2018; Published: January 31, 2018
Abstract
Introduction: Glaucoma is a progressive and multifactorial chronic optic neuropathy. According to data from the World Health Organization, it is responsible for 13% of global blindness with 2.4 million new cases each year. In Brazil, there are few statistical studies regarding the epidemiological profile of patients enrolled in the Glaucoma Carrier Care Program with dispensing of eye drops, motivating this pilot study.
Methods: Medical records from 200 patients enrolled in the Glaucoma Patient Care Program with dispensing of eye drops at the Glaucoma and Cataract Reference Center from the Santa Casa Group of Belo Horizonte – Minas Gerais were analyzed. Demographic, clinical and therapeutic data were evaluated. Results: Patients with primary open-angle glaucoma were the majority (90%, n = 180), followed by the ocular hypertension group (5%, n = 10). The mean age of the patients was 63.8 ± 12.8 years, with 59.5% with age ≥ 60 years. The female sex prevailed (68.5%), 18.5% of the patients were black and 35.5% had a family history of glaucoma, 54.5% arterial hypertension and 19% diabetes mellitus. Regarding the use of ocular hypotensors, 42% (n = 84) were treated with monotherapy and 58% (n = 116) with drug association, with a mean of 1.7 (SD = 0.8) drug/patient, with prostaglandin analogues being the most used class (67.5%, n = 135).
Discussion and Conclusion: The prevalence, inicidence and type of glaucoma varies in different populations. The greater frequency of prostaglandin analogues in this study compared to other Brazilian reports is due to the availability of access to medication through its dispensation in our Glaucoma and Cataract Reference Center, linked to the policy of dispensing eye drops from the Brazilian State Healthcare System (SUS). Further studies are needed to help in terms of prevention glaucoma and public health policy.
Keywords: Glaucoma; Epidemiology; Ophthalmology; Treatment
Abbreviations: IBGE: Brazilian Institute of Geography and Statistics; IOP: Intraocular pressure; POAG: Primary open-angle glaucoma; OH: Ocular hypertension;
Introduction
Glaucoma is a progressive, multifactorial chronic optic neuropathy and affects over 60 million people, or 2 to 3% of the world's population, 8.4 million of whom are bilateral blind. In 2020 this number will rise to 80 million, followed by an increase to 111,8 milion in 2040. [1-4] It is a public health problem, being the second leadingcause of blindness worldwide. [2,4] Visual loss and blindness due to glaucoma are important both for its prevalence and for the financial burden it causes to the social security system. According to data from the World Health Organization (2002) glaucoma accounts for 13% of global blindness, and 2.4 million new cases emerge each year. [5] Even in developed countries, half of all glaucoma cases are undiagnosed. [1]
The only effective treatment for glaucoma is to lower intraocular pressure with eye drops, pills, laser surgery, traditional surgery or a combination of these methods. Ocular hypotensive eye drops is the most commom option to control the disease. [1] However, due to the chronicity, the cost of medication and the low-income population, adherence to treatment has been one of the main challenges experienced by people with glaucoma in developing countries.
In order to mitigate the social impact and prevent the progression of glaucoma, the Brazilian State Healthcare System (SUS) created, in 2008, ordinance No. 957/GM, which instituted the National Ophthalmology Care Policy and Administrative Rule No. 228/SAS, which through Annex IV defined the clinical protocol and the therapeutic guidelines of the Brazilian Glaucoma Carrier Attention Program and the drugs for glaucoma treatment were contemplated. [6]
In Brazil, there are few studies about the epidemiological profile of patients enrolled in this Glaucoma Patient Care Program with dispensing of eye drops, motivating this pilot study.
Methods
The study was conducted in accordance with national and international resolutions on ethics and good clinical practice (ICH Harmonized Tripartite Guidelines for Good Clinical Practice - 1996, CNS resolution 466/12, resolution CNS 251/97 and the Helsinki Declaration). All data obtained were kept confindential and only by the researchers involved in the project.
The retrospective study analyzed 200 charts of patients enrolled in the Glaucoma Patient Care Program with dispensing of eye drops at the Glaucoma and Cataract Reference Center of a Brazilian Tertiary Eye Care Center (Santa Casa de Belo Horizonte – Minas Gerais) attended during two months. Demographic data, clinical and therapeutic diagnosis of the patients were analyzed. Racial Classification was self-declared and segmented according to criteria of Brazilian Institute of Geography and Statistics (IBGE) [7].
For enrollment and inclusion in the eye drops dispensing program, patients met one of the following criteria: intraocular pressure (IOP) above 25 mmHg; IOP between 21 and 24 mmHg and presenting with 2 or more risk factors (age over 60 years, single eye, myopia, impossibility to visualize the fundus of the eye, family history of glaucoma in first degree relatives, black race, systemic hypertension or diabetes mellitus); any level of IOP with increased digging of the optic disc (cup-to-disc ratio greater than 0.6) or visual field loss compatible with glaucoma. Patients who presented acute angle-closure glaucoma or did not agree with the terms of informed consent were excluded. Patients with secondary glaucoma had the underlying cause treated and the clinical treatment was used as adjuvant.
To plot the sample, frequency tables were constructed with the number of occurrences and their respective percentages for the categorical variables and the measures of central tendency (mean and median) and variability (standard deviation) measures were calculated for the quantitative variables. Clinical data were analyzed statiscally using SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Data were analyzed: 137 (68.5%) female and 63 (31.5%) male, mean age 63.8 ± 12.8 years, with 59.5% (n = 119) patients aged 60 years or over. According to self-declared ethnicity, 80.5% (n = 161) were considered Intermediate (“pardos” in Portuguese), 18.5% (n = 37) Black and 1% (n = 2) White.
The type of glaucoma most observed in the study was primary open-angle glaucoma (POAG), corresponding to 90% (n = 180) of the cases, followed by ocular hipertension (OH) corresponding to 5% (n = 10) angle-closure glaucoma and secondary glaucoma presented a similar prevalence of 2.5% (n = 5) each.
In relation to associated diseases, 109 (54.5%) individuals had systemic arterial hypertension and 38 (19.0%) had diabetes mellitus. Family history of glaucoma was present in 71 (35.5%) patients. Among the study participants, 24 (12.0%) had unilateral blindness. Background of ocular surgeries were described in 18% (n = 36) of the patients, with a total of 54 operated eyes. In all, 17% (n = 34) eyes were submitted to intraocular lens implantation, 6.5% (n = 13) to trabeculectomy, 3% (n = 6) to combined facectomy and trabeculectomy surgery, and 0.5% (n = 1) to evisceration.
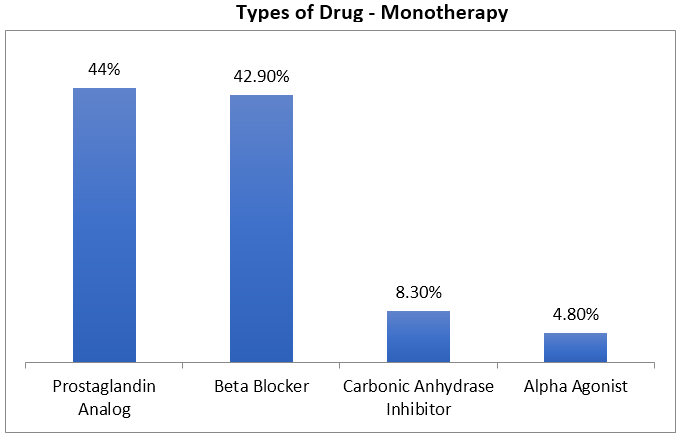
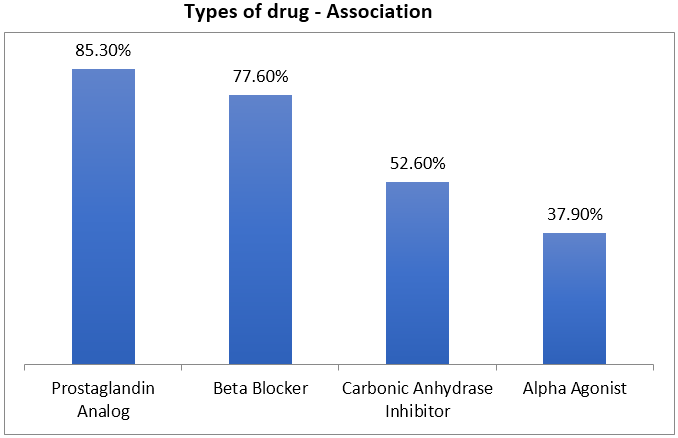
Regarding the use of eye drops, antiglaucomatous therapy was analyzed. Prescription of ocular hypotensive agents was observed in 42% (n = 84) as monotherapy and in 58% (n = 116) as combined therapy (Figures 1 and 2) with an average of 1.7 (SD = 0.8) drugs per patient. Prostaglandin analogues were used for 67.5% (n = 135) of the patients, beta-blockers for 63% (n = 128), carbonic anhydrase inhibitors by 33.5% (67) and 24% (n = 48) used alpha agonists. In all drug association, 60 (51.7%) patients used two drugs; 50 (43.1%), three drugs; and 6 (5.2%), four drugs. The most commonly used drug association (26.7%) was prostaglandin analogues with beta-blocker (Table 1). About 40% of patients with OH and 75% with glaucoma required two or more medications, prostaglandin analogues were first-line drugs, used in 67.5% of patients, followed by beta-blockers (63% ).
Figure 1: Percentage of drugs prescribed in monotherapy in 84 patients (42%) of
a pilot project of the epidemiological profile of a Brazilian Tertiary Eye Care Center
(Glaucoma and Cataract Reference Center) in the city of Belo Horizonte/MG, Brazil.
Figure 2: Percentage of drugs prescribed in association in 116 patients (58%) of a
pilot project of the epidemiological profile of a Brazilian Tertiary Eye Care Center
(Glaucoma and Cataract Reference Center) in the city of Belo Horizonte/MG, Brazil.
| Association | Number of Cases - N | Percentage (%) |
| PA+BB | 31 | 26,7% |
| PA + BB+ CAI | 24 | 20,7% |
| PA + BB + AA | 12 | 10,3% |
| PA + CAI | 9 | 7,8% |
| PA + CAI + AA | 9 | 7,8% |
| PA + AA | 8 | 6,9% |
| Others | 23 | 19,8% |
| Total | 116 | 100% |
Table 1: Drug Associations used in the therapy of 116 patients (58%) of a pilot project of the epidemiological profile of a Brazilian Tertiary Eye Care Center (Glaucoma and Cataract Reference Center) in the city of Belo Horizonte/MG, Brazil. PA = prostaglandin analog, BB = beta blocker, CAI = carbonic anhydrase inhibitor, AA = alpha agonist, n = number of cases/percentage.
Discussion
The prevalence, incidence and type of glaucoma varies in different populations and, in Brazil, there is a lack of epidemiological studies about the disease.[8] In 2007, Sakata., et al. examined 1636 individuals over 40 years and identified a prevalence of glaucoma of 3.4%, and 72% corresponded to POAG [9]. Urbano., et al. (2003) also found a lower prevalence of POAG (56.2%) in their study performed at a Brazilian tertiary eye care center in Campinas – São Paulo [10]. The reason for these discrepancies remains to be established.
Glaucoma’s prevalence increases with age, especially after 60 years.[1,11] In our study, we observed that the population over 60 years old was the most commonly affected. It was also observed a high final mean age (63.8 ± 12.8 years), corroborating previous Brazilian data. [5,8,10,12] Female gender was more affected (68.5%) which is also consistent with previous reports as Salai., et al. (2011) and Ramalho., et al. (2007) with 59% and 70% respectively. [5,13] These results differ from Tham., et al. (2014) who found that men were 36% more likely to have POAG than women [4].
Ethnic background is an important glaucoma risck factor. The frequency of Blacks found in 18.5%, was similar to Oliveira., et al. (2003) (19.9%) [14]. African descent has being associated with earlier development of glaucoma and with faster progression of the disease in American statistics. [1,15] These could explain the increased severity of the disease in this population when compared with white populations in an age-matched comparisons of elderly patients. [16]
The association of systemic arterial hypertension and diabetes are still controversial due to the age of the affected patients and the high incidence of chronic diseases in this age group. [3,5,11,17-18] Positive family history is considered one of the risk factors for the development of POAG in several populations studied [11,19], being our result of 35.5% in accordance to 35% of Ramalho., et al. (2007) and differing from the findings of Oliveira., et al. (2003) and Salai., et al. (2011) who reported 13.9% and 13%, respectively.[13,14]
The treatment of glaucoma begins, in the majority of patients, with topical hypotensive ocular drugs. There are several classes of drugs available and the choice of medication should be individualized. Monotherapy should be the first choice to achieve target IOP, but about 40% of patients with ocular hypertension and 75% of patients with glaucoma require two or more medications. [20] Prostaglandin analogues are the most effective agents for decrease IOP and have the best systemic safety profile. Therefore, they are commonly the first-line drugs. [20]
The most commonly used class in our study were prostaglandin analogues (67.5%) followed by beta-blockers (63%), showing different results from previous Brazilian reports where timolol maleate was the most prescribed topical hypotensive agent. [5, 12,14] In this study, 42% patients were in monotherapy and 58% in drug association, differing from Oliveira., et al. (2003) and Ramalho., et al. (2007) who observed in their analysis 19% and 73% of the patients under monotherapy treatment, respectively. [5,14] Our most commonly used association was the prostaglandin analog with beta-blocker, differing from Oliveira., et al. (2003) who had timolol maleate with brimonidine as the most frequent. [14]
The greater frequency of prostaglandin analogues in this study compared to other Brazilian reports is due to the availability of access to medication through its dispensation in our Glaucoma and Cataract Reference Center, linked to the policy of dispensing eye drops from the Brazilian State Healthcare System (SUS). This class of IOP-reducing agents gained popularity in glaucoma medical management because of the good systemic safety profile and the best user compliance with a dosage convenience (only once daily), improving the quality of life of patients treated in our Glaucoma and Cataract Reference Center.
Conclusion
Glaucoma is a public health problem. Early diagnosis and appropriate treatment are importants for the prevention of blindness caused by advanced stage disease. Adherence to treatment is linked to the dosage of medications, their cost and side effects. In the case of a multifactorial disease, with only one modifiable risk factor, intraocular pressure, it is essential to control the disease a regular clinical treatment and patient adherence. Further studies on the Brazilian epidemiological profile of glaucoma are needed to adequately characterize it and help in terms of prevention (glaucoma and blindness) and public health policy, motivating the expansion of this project throughout a 12 month follow up in the population of nearly 7,000 patients enrolled in the Glaucoma Carrier Care Program of this Tertiary Eye Care Reference Center.
Acknowledgements
We thank Leandro Cunha, MD for clinical support.
We thank Leandro Cunha, MD for clinical support.
References
- Quigley HA. “Glaucoma”. Lancet 377.9774 (2011): 1367-1377.
- Sperandio AMG. “Promoção da saúde ocular e prevenção precoce de problemas visuais nos serviços de saúde pública”. Rev Saúde Pública 33.5 (1999): 513-520.
- Amaral Filho JM., et al. “Custo mensal de medicações antiglaucomatosas no Brasil”. Arquivos Brasileiros de Oftalmologia6 (1999): 123-126.
- Tham YC., et al. “Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis”. Ophthalmology 121.11 (2014): 2081-2090.
- Ramalho CM., et al. “Perfil socioeconômico dos portadores de glaucoma no serviço de oftalmologia do hospital universitário da Universidade Federal de Juiz de Fora - Minas Gerais – Brasil”. Arquivos Brasileiros de Oftalmologia 70 (2007): 809-813.
- Portal da Saude. “Ministério da Saúde”. (2018):
- Censo demográfico 2010. “Instituto Brasileiro de Geografia e Estatística”. (2017):
- “3° Consenso brasileiro glaucoma primário de angulo aberto. 3a ed”. São Paulo: Sociedade brasileira de glaucoma (2009):
- Sakata K., et al.“Prevalence of glaucoma in South Brazilian population: Projeto Glaucoma”. Investigative Ophthalmology & Visual Science 48.11 (2007): 4974-4979.
- Urbano AP., et al. “Avaliacao dos tipos de glaucoma no serviço de oftalmologia da UNICAMP”. Arquivos Brasileiros de Oftalmologia 66 (2003): 61-65.
- McMonnies and Charles W. “Glaucoma History and Risk Factors”. Journal of Optometry 10.2 (2017): 71-78.
- Silva LM., et al. “Tratamento clinico do glaucoma em um hospital universitário: custo mensal e impacto na renda familiar”. Arquivos Brasileiros de Oftalmologia65 (2002): 299-303.
- Salai AF., et al.“Perfil clinico epidemiológico de pacientes com glaucoma encaminhados ao serviço de oftalmologia do Hospital Universitario da Universidade Federal de Santa Catarina”. Arquivos Catarinenses de Medicina 40 (2011): 37-42.
- Oliveira A., et al.“Caracteristicas dos pacientes atendidos pela primeira vez no sector de glaucoma da Universidade Federal de Sao Paulo – UNIFESP”. Arquivos Brasileiros de Oftalmologia 66 (2003): 785-790.
- Quigley HA., et al.“Rate of progression in open-angle glaucoma estimated from cross- sectional prevalence of visual field”. American Journal of Ophthalmology 122.3 (1996): 355-363.
- Kapetanakis VV., et al. “Global variations and time trends in the prevalence of primary open angle glaucoma (POAG): a systematic review and meta-analysis”. British Journal of Ophthalmology 100 (2015): 86-93.
- Leske MC., et al.“Risk factors for open angle glaucoma. The Barbados Eye Study”. Archives of ophthalmology 113 (1995): 918-924.
- Tielsch JM., et al.“Diabetes, intraocular pressure and primary open-angle glaucoma in the Baltimore Eye Survey”. Ophthalmology 102 (1995): 48-53.
- Leske MC. “Open-angle glaucoma - an epidemiologic overview”. Ophthalmic Epidemiology 14 (2007): 166-172.
- Lichter PR., et al. “Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery”. Ophthalmology 108 (2001): 1943-1953.
Citation:
Hévila Rolim., et al. “Epidemiological Profile of Patients Registered in the Brazilian Glaucoma Carrier Attention Program
from A Tertiary Eye Care Reference Center”. Ophthalmology and Vision Science 1.5 (2018): 188-194.
Copyright: © 2018 Hévila Rolim., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.