Case Report
Volume 1 Issue 4 - 2017
Dysplasia Epiphysealis Hemimelica – Report of A Rare Developmental Condition with An Emphasis on Management
1Central Institute of Orthopaedics, VMMC & Safdarjung Hospital, New Delhi, India
2Post graduate institute of medical education and research, Chandigarh, India
3SMS medical College, Jaipur, India
4VSS medical College, Sambalpur, Odisha, India
2Post graduate institute of medical education and research, Chandigarh, India
3SMS medical College, Jaipur, India
4VSS medical College, Sambalpur, Odisha, India
*Corresponding Author: Prateek Behera, Assistant Professor, Central Institute of Orthopaedics, VMMC & Safdarjung Hospital, New Delhi, India.
Received: May 09, 2017; Published: May 12, 2017
Abstract
Background: Dysplasia Epiphysealis Hemimelica (DEH) is a rare disease (incidence 1:1,000,000), characterized by an osteochondral overgrowth affecting one or more epiphyses. The age of presentation is usually between two and fourteen years. The radiological findings are often considered sufficient for the diagnosis.
Case Presentation: We report a case of a six-year-old boy who presented with a history of ankle and knee pain since past four months and was diagnosed as having DEH after obtaining the necessary radiographs. In view of ankle pain, deformity and restriction of movements decision of excision of lesion from ankle was made. Excision of lesion from knee was also done. At follow up, the ankle pain was absent with good movements but the knee became stiff.
Conclusion and clinical significance: Although case reports describing the management options for patients with DEH are available, the complications of surgery have not been dealt with, in most of the reports. We have described a rare developmental condition and the management undertaken and the complications thereof to emphasize on the need of proper patient and treatment selection in each such case.
Introduction
Dysplasia epiphysealis hemimelica (DEH) is also known as Fairbank's disease and Trevor's disease. It is a rare congenital condition and is believed to be a developmental disorder [1,2]. It is a non-hereditary condition and is believed to mimic synovial chondromatosis [2] and osteochondroma [3,4]. DEH is characterised by an asymmetrical limb deformity due to localized overgrowth of cartilage believed to affect the limb bud in early fetal life [1]. The condition occurs mostly in the ankle or knee region and it is always uncommon in the upper extremity [5,6]. Presentation most often is in childhood when children present with pain, deformity or restriction of movements. We are reporting a case of DEH in a six-year-old child who presented with ankle and knee pain along with ankle deformity and we were faced with management dilemma of whether to operate or not. Following a surgery to excise the mass we were faced with the complication of stiff knee which required vigorous physiotherapy along with bracing for recovery.
Case Report
A six-year-old male, patient presented with pain in his left ankle and knee of four months’ duration to the outpatient department. In the past four months, the patient had progressively increasing pain and limp which was significant when attempting to run or walk quickly. Parents also provided a history of on and off swelling of the ankle and knee joints. He was having constant pain and swelling for the preceding three weeks. On examination, swelling over the medial malleolus was observed with no tenderness (Figure 1); a mild effusion of the ankle joint was also noticed. Ankle plantar flexion and dorsiflexion were restricted as compared to the opposite side and were terminally painful. No swelling was noticed around the knee as such but the flexion was restricted terminally and clicks were noticed each time the knee was flexed beyond 90 degrees.

Figure 1: Clinical photograph of the left ankle of the child showing
an abnormal swelling around the medial malleolus.
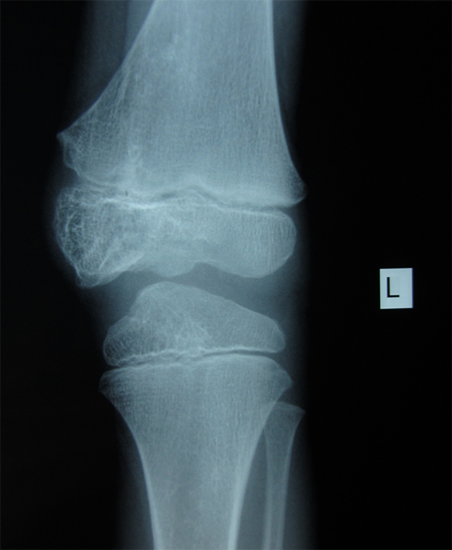
Plain radiographs of both the ankle and the knee joints were obtained in orthogonal planes. Irregularities on the articular surface of
the talus with calcifications were observed in the articular space; also noted was a distinct abnormal growth from the medial malleolus
(Figure 2a, 2b and 2c). An abnormal growth was seen arising from the medial femoral condyle and a small bony outgrowth was seen
from the tibial epiphysis (Figure 3). A sagittal plane CT scan of the knee (Figure 4) showed outgrowths from the femur and tibia both.
Surgical excision of the ankle lesion was planned because of the significant functional limitation and pain but we were in a dilemma regarding the management of the lesion around the knee. We were undecided whether to attempt to manage the knee conservatively or go ahead with surgery. We discussed the two options with the parents who wanted to have a surgical treatment for all the lesions in one go. We finally decided to go ahead with excision of lesion from knee also.
Surgery was performed under general anaesthesia under pneumatic tourniquet. Anterior approach was used dissecting between the tendons of tibialis anterior and extensor hallusis longus. The osteochondral outgrowths from the medial malleolus were identified which were well delineated from it (Figure 5). A part of the deltoid ligament was also found be attached with the growth. After carefully separating it from the deltoid ligament, the osteochondral mass was excised. The articular surface of the talus showed multiple small osteochondral lesions arising from the talar dome (figure 6). These were easily separable from the rest of the talus and were excised. After thorough lavage of the joint the wound was closed in layers. The knee was approached via an anterior midline skin incision and medial parapatellar approach. The osteochondral fragments found arising from the femoral and tibial condyles were excised. Intra op range of motion improved and the clicks on flexion disappeared. Intravenous antibiotics were continued for 48 hours and the immediate post-operative period was uneventful. Histopathological analysis of excised fragments showed a picture like osteochondroma.
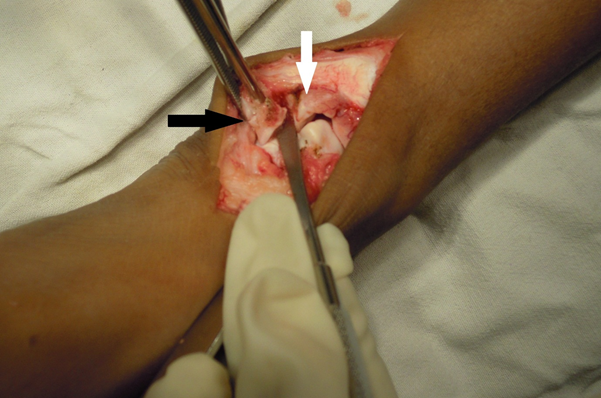
Figure 5: Intra operative picture showing the bony lesion (black arrow) as
separate from rest of medial malleolus (white arrow).
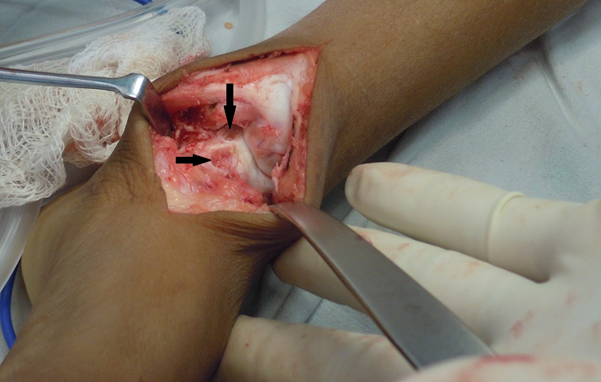
Figure 6: Intra operative picture showing the talar dome after excision of the lesion (black arrows).
The child was followed up at 2 weeks for suture removal and again at 4, 6 and 8 weeks’ post-surgery. The range of motion was found to have increased at ankle but decreased at the knee. There was a restriction of flexion at the knee primarily due to pain. The child was started on supervised range of motion exercises for the knee. At 4 months follow up the child was pain free at the ankle with no limitation of ankle movements but had mild pain at the knee with restriction of knee movements. The knee flexion was around 100 degrees which was better than what it was 8 weeks after surgery but was less than the pre-operative flexion. A flexion deformity of 20 degrees had developed and a moulded knee extension brace was used, with the leg removed regularly for knee flexion exercises. After a period of further 4 months i.e. 8 months after the surgery, full extension and a flexion of 130 degrees were obtained. Some residual flexion limitation still persisited.
Discussion
Dysplasia epiphysealis hemimelica (DEH) was originally described in 1926 by Mouchet and Berlot [7] as ‘tarsomegalie’ but it was Fairbank [1] who proposed the name by which it is known at present. It has a reported incidence of 1:1,000,000 and generally affects children in the age group of 2 to 14 years and is more common in boys. Generally, the involvement is unilateral with the lesions originating from half of the epiphysis especially of the lower limbs [8,9,10]. It is believed to result from an abnormality at the embryonic stage of development with Trevor [11] hypothesising it to be a congenital error or insult perpetrating the defect in the lower limb buds during early fetal life. A differential diagnosis of osteochondroma, synovial chondromatosis, chondrodysplasia punctata among others have often been advanced [2,4].
Clinical presentation is often in the form of localized painless swelling determined by the pattern of epiphyseal cartilage growth but often the patient may present with painful swelling, restriction of movements of the affected joints, angular deformity of the limb, limb length deformity, mechanical symptoms from the presence of the mass etc..., [4,10]. Many atypical presentations in terms of location and symptomatology have been reported in literature. A detailed review of such presentations has been reported by Gopinathan., et al. [4].
Suspicion on part of the treating physician is needed for arriving on a differential diagnosis of DEH. Imaging studies, primarily plain radiographs are needed for arriving at a diagnosis. CT scans and MRI may also be done to further evaluate the extent of the lesion and to define the relationship of mass and the bone. Peduto., et al. [12] have reported that a diagnosis may be made based on radiographic findings and biopsy for diagnosis is not required. Radiographs may show one or more irregular masses with focal ossification adjacent to the border of one of the halves of the epiphysis (with overgrowth), with irregular enlargement of epiphyseal centers and adjacent metaphysic [1]. While CT and MRI are good diagnostic modalities though they are not mandatory in every case and should be ordered based on the merit of the case.
Azouz., et al. [13] have classified the disease depending on the extent of involvement into three types: A. localised form, B. Classic form (more than one area of osseous involvement in a single extremity) and C. generalised or severe form. The type B (classic form) is the most often reported variety and it accounts for more than two -thirds of cases. Our patient also presented with a type B (classic type) of DEH, affecting the distal tibial, talar distal femoral and proximal tibial epiphyses.
Management options have been discussed in detail by previous authors [2,3,4,10]. Supervised neglect or wait and watch approach as well as surgical excision of the lesion has both been described in literature. While some authors favour an early excision of extra articular lesions, a conservative non-operative approach should be given consideration for asymptomatic intra articular lesions in skeletally immature patients. If a patient is asymptomatic and the lesion is causing significant restriction of day to day activities, then a surgical excision of the lesion is probably the best mode of treatment. Hence it is probably best to decide the treatment modality on case by case basis instead of generalizing the treatment.
One critical issue which has not been addressed adequately is that of post-operative stiffness of the joint. As most of the patients are young children who tolerate pain poorly and are non-complaint to range of motion exercises which is due to their awareness to the need of such exercises, post-operative stiffness may be a complication of the surgical line of management and this may lead to poor functional outcomes. Stiffness as a complication has been reported by Kuo., et al. [10]. In the case which we have reported, we had to face this complication of knee stiffness which we believe was mainly due to lack of mobilization of the joint. We excised lesions from both the ankle and knee and had a pain free, mobile ankle but a stiff knee with mild pain. This made us to retrospectively question our decision of operating on the knee as the pre-operative symptoms were not significantly disabling enough for the patient. Though with supervised physiotherapy movement has been regained yet we believe that a proper decision on our part could have avoided the complication all together. Unless and until the symptoms are severe enough to hamper the activities of daily living one should avoid the surgical option at least in the young children.
In conclusion, the case which we have reported has added to the pool of ever increasing number of cases of DEH being reported in the literature thus making this rare condition not so uncommon. We have discussed the management options available and have tried to emphasize the need for proper patient and treatment selection. Stiffness as a complication has not been discussed much in published reports but probably there has been some stiffness in almost every operated case especially in young patients with surgery around the knee.
Acknowledgement
The authors wish to thank the parents of the child for providing consent for the publication of the patient related data and photographs
The authors wish to thank the parents of the child for providing consent for the publication of the patient related data and photographs
References
- Fairbank TJ. “Dysplasia epiphysealis hemimelica (tarso-epiphyseal aclasis)”. The Journal of bone and joint surgery British 38-B.1 (1956): 237-257.
- Gokkus K., et al. “Dysplasia epiphysealis hemimelica of the ankle joint: a case report”. Journal of Orthopaedic Surgery (Hong Kong) 19.2 (2011): 254-256.
- Glick R., et al. “Dysplasia epiphysealis hemimelica (Trevor disease): a rare developmental disorder of bone mimicking osteochondroma of long bones”. Human Pathology 38.8 (2007): 1265-1272.
- Gopinathan NR., et al. “Acutely presenting kissing lesions of the ankle: an atypical Trevor’s disease and literature review of other unusual presentations of the disease”. BMJ Case Reports 25 (2013): bcr0220125798.
- Lamesch AJ. “Dysplasia epiphysealis hemimelica of the carpal bones”. Report of a case and review of the literature Journal of Bone Joint Surgery American volume 65.6 (1983): 398-400.
- Kircher J., et al. “A rare case of Trevor's disease (dysplasia epiphysealis hemimelica) in the elbow”. Journal of Shoulder Elbow Surgery 22.2 (2013): e12-15.
- Mouchet A and Berlot J. “La tarsomegalie”. Journal of Radiol Electrol 10 (1926): 289-293.
- Bansal P., et al. “Dysplasia epiphysealis hemimelica or Trevor’s disease of proximal tibia mimicking loose body”. Journal of Clinical Orthopaedics and Trauma1.2 (2010): 105-106.
- Wiart E., et al. “Bilateral dysplasia epiphysealis hemimelica of the talus associated with a lower leg intramuscular cartilaginous mass”. Pediatric Radiology 42.4 (2012): 503-507.
- Kuo RS., et al. “Dysplasia epiphysealis hemimelica: clinical features and management”. Journal of Pediatric Orthopaedics 18.4 (1998): 543-548.
- Trevor D. “Tarso-epiphysial aclasis: a congenital error of epiphysial development”. Journal of Bone Joint Surgery British 32-B.2 (1950): 204-213.
- Peduto AJ., et al. “MR imaging of dysplasia epiphysealis hemimelica: bony and soft-tissue abnormalities”. American Journal of Roentgenology 172.3 (1999): 819-823.
- Azouz RM., et al. “The variable manifestations of dysphasia epiphysealis hemimelica”. Pediatric Radiology 15.1 (1985): 44-49.
Citation:
Prateek Behera., et al. “Dysplasia Epiphysealis Hemimelica – Report of A Rare Developmental Condition with An Emphasis
on Management”. Orthopaedic Surgery and Traumatology 1.4 (2017): 133-139.
Copyright: © 2017 Prateek Behera., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.







































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.