Research Article
Volume 1 Issue 1 - 2016
Vacuum-Assisted Closure Ulta with Veraflo Instillation for the Healing of Diabetic Foot Wounds
Department of Orthopaedic Surgery, National University Hospital, Singapore
*Corresponding Author: Associate Professor Aziz Nather, University Orthopaedics, Hand & Reconstructive Microsurgery Cluster, National University Health System, Singapore.
Received: June 18, 2016; Published: June 24, 2016
Abstract
Introduction: This is a prospective study to evaluate the effectiveness of Vacuum Assisted Closure (V.A.C) Ulta Therapy Unit with VeraFlo Instillation Therapy in the healing of diabetic foot wounds.
Methods: 5 patients admitted to NUH Diabetic Team from April to May 2014 with infected diabetic foot wounds were subjected to debridement followed by the application of this new technique. Our protocol consisted of setting the unit at continuous mode with 10 minutes soak and 4 hours of suction. A negative pressure of -125mmHg was delivered to the wound bed with a pressure of -25mHg in between the cycles. All patients had at least one palpable pulse and an ABI of > 0.8 and a TBI of > 0.7. Only normal saline was used for instillation. The cases include one ulcer on dorsum of foot, one post-ray amputation wound, one over the calf, one over the tendo-achilles region and one ulcer in the non-weight bearing portion of the sole.
Results: Reduction in wound surface area was found to be approximately 27.16% with healthy granulation tissue. All 5 patients achieved wound closure by split-skin grafting in an average of 8 days. All 5 cases showed 100% healing of the wound with split-skin grafting. All 5 cases showed negative culture before split-skin grafting.
Conclusion: V.A.C. Ulta with V.A.C. VeraFlo was found to be useful in the management of diabetic foot wounds. However, a larger, randomised control study is required to fully evaluate the effectiveness of this new technique.
Keywords: VAC Ulta: VAC Veraflo; Negative Pressure Wound Therapy; Instillation therapy; Healing; Diabetic foot wounds
Abbreviations: V.A.C.: Vacuum Assisted Closure; NUH: National University Hospital; ABI: Ankle-brachial index; TBI: Toe-brachial index; NPWT: Negative pressure wound therapy; NPWTi: Negative pressure wound therapy with instillation; ROCF: Reticulated open-cell foam; HbA1C: Glycated hemoglobin; SSG: Split-skin graft WBC: White blood cell; CRP: C-reactive protein; ESR: Erythrocyte sedimentation rate
Introduction
Diabetes Mellitus is the “global epidemic of the 21st century". In 2015, 1 in 11 adults are diabetic (415 million) and this number will increase to 1 in 10 adults by 2040 (642 million) [1]. 15% of all diabetic patients develop foot ulcers and 85% of diabetic-related lower limb amputations begin with an ulcer [2].
Healing of diabetic foot ulcers often requires long treatment with multiple debridements. Several advanced wound care therapies have been developed to achieve wound bed preparation for eventual wound closure. Such therapies include negative pressure wound therapy (NPWT) using the Vacuum Assisted Closure (V.A.C.) Therapy System. NPWT has been shown to facilitate the rapid formation of healthy granulation tissue [3], complete ulcer closure [4] and faster wound healing. [5]
When compared to conventional dressings such as standard moist wound care, NPWT delivered by the V.A.C. Therapy System led to a higher proportion of healed wounds, faster healing rates and potentially fewer re-amputations than standard care. [6] When VAC was compared with saline-moistened gauze in the healing of diabetic foot wounds, faster wound healing was also noted. [7]
As an extension to V.A.C. therapy, the V.A.C. Ulta Therapy Unit with V.A.C. VeraFlo Instillation Therapy option was developed which utilizes negative pressure wound therapy with instillation (NPWTi). It uses instillation-specific reticulated open-cell foam (ROCF) dressings: ROCF-V, V.A.C. VeraFlo Dressing or ROCF-VC, V.A.C. VeraFlo Cleanse Dressing. It allows for delivery of automated topical wound solution to the wound bed, to clean and treat the wound, while keeping the wound moist, enclosed and sterile. Cycles of negative pressure is delivered to the wound bed while maintaining a low level of negative pressure between cycles. This ensures that suction is maintained throughout therapy (never at 0mmHg) to minimize the risk of leaks and fluid accumulation at wound sites. This may help to minimize patient discomfort from foam expansion that can occur due to over-soaking when negative pressure reaches 0mmHg. [8]
NPWTi has been shown to be effective in the healing of many types of wounds – abdominal and chest wounds [9], severe soft tissue infections and necrotizing fasciitis [10], post traumatic osteomyelitic wounds [11], chronic osteomyelitis wounds [12], periprothetic infections in the knee [13], periprosthetic infection in hip arthroplasty [14], infected orthopedic implants [15] and diabetic foot wounds [16,17].
Clinical trials have shown that NPWTi reduces the rate of recurrence of infection, the need for repeated surgical interventions [11] and the mean time to wound closure. [18]
This pilot study discusses the role of VAC VeraFlo and advanced reticulated open-cell foam (ROCF) dressings in the healing of diabetic foot wounds.
Materials and Methods
A prospective case series of five patients was conducted by the National University Hospital, Diabetic Foot Team from April 2014 to May 2014. The study population was made up of 3 males and 2 females with a mean age of 60.6 (range, 51-79 years). Patients selected for this study must fulfill the following criteria: ankle-brachial index (ABI) > 0.8, toe-brachial index (TBI) > 0.7 and at least one pulse palpable.
Study protocol
Documentation in the study protocol included the patients’ profile, history of diabetes and presence of complications of diabetes. The progress and appearance of the wound throughout the application of VAC VeraFlo therapy were closely followed. All wounds were measured and photographed with a ruler placed beside the wound to allow the length and width of the wound to be measured.
Documentation in the study protocol included the patients’ profile, history of diabetes and presence of complications of diabetes. The progress and appearance of the wound throughout the application of VAC VeraFlo therapy were closely followed. All wounds were measured and photographed with a ruler placed beside the wound to allow the length and width of the wound to be measured.
Investigations performed and documented included markers of healing (Glycated Haemoglobin - HbA1C, hemoglobin count and albumin level) and markers of infection (leukocyte count, C-reactive protein and erythrocyte sedimentation rate). A tissue specimen was taken from the wound and sent for culture and sensitivity.
The pressure settings, instillation volume, date of initiation and end of V.A.C. VeraFlo therapy, number and date of V.A.C. VeraFlo dressing changes were recorded.
Method of application of V.A.C. VeraFlo therapy
Prior to application of V.A.C. VeraFlo therapy, adequate debridement of all necrotic and infected tissue was performed. The wound was then thoroughly washed with normal saline.
Prior to application of V.A.C. VeraFlo therapy, adequate debridement of all necrotic and infected tissue was performed. The wound was then thoroughly washed with normal saline.
The V.A.C. VeraFlo dressing was cut to fit the size and shape of the wound.
The wounds were sealed using semi-permeable film drape and a small hole cut in the center of film.
The V.A.C. Vera T.R.A.C. Pad was placed directly over the hole in the film to allow for the delivery and removal of topical wound solution to the wound bed.
The Vera T.R.A.C. Tubing was connected to the Canister tubing. The pressure level and mode on the V.A.C. Ulta therapy unit was then set by the clinician.
For all patients, the V.A.C. Ulta therapy unit was set at continuous mode with 10 minutes soak and 4 hours of suction. A negative pressure of -125mmHg was delivered during suction and -25mmHg during soak. V.A.C VeraFlo dressing change was performed every 72-96 hours. The volume of instillation solution was determined via fill assist followed by a clinical evaluation by the doctor at patients’ bedside.
The dressings used were instillation-specific reticulated open-cell foam (ROCF) dressings, ROCF-V, V.A.C. VeraFlo Dressing.
At each dressing change, the wound was carefully assessed and photographed. The nature of the drainage fluid from the wound was also inspected. V.A.C. VeraFlo therapy was stopped if the flow was clean. At the end of V.A.C. VeraFlo therapy, the final appearance of the wound was photographed and recorded.
When instillation therapy stopped, the wound was treated with VAC therapy without instillation. Tissue from the wound was taken and sent for culture and sensitivity. Once the result of culture and sensitivity is negative, split skin grafting was then performed.
Results
Table I showed the demographics of the study cohort. The age of patients in this study ranged from 51 – 79 (average: 60.6). There were 3 males and 2 females. There were 3 Chinese, 1 Indian and 1 Malay.
| Age (y) | Gender | Race | Markers of Healing | Vascular status | Wound diagnosis | Wagner grade | Infection markers | Culture and Sensitivity of wound | ||||||
| Hb | Albumin | HbA1c (%) | ||||||||||||
| Pulses | ABI | TBI | WBC | CRP | ESR | |||||||||
| 51 | Male | Indian | 13.1 | 34 | 16.2 | 2+ | 1.18 | 0.9 | Ulcer dorsum right foot | 2 | 10.91 | 22 | 67 | Methicillin-sensitive staphylococcus aureus |
| 57 | Male | Chinese | 10 | 38 | 8.3 | 2 | 2.32 | 0.8 | Ulcer post 5th ray amputation | 2 | 17.43 | 186 | 104 | Pseudomonas, Streptococcus agalactiae |
| 65 | Female | Chinese | 8.8 | 32 | 10.1 | 2 | 0.9 | 0.8 | Ulcer over right calf | 2 | 16.04 | 195 | 111 | Klebsiella |
| 51 | Female | Malay | 10.1 | 36 | 10.3 | 2 | 1.04 | 0.89 | Ulcer sole of foot | 2 | 22.50 | 217 | 40 | Methicillin-sensitive staphylococcus aureus |
| 79 | Male | Chinese | 9.8 | 33 | 7 | 2+ | 1.15 | 0.8 | Ulcer over right tendoachilles | 2 | 7.55 | 117 | 55 | E.coli, Morganella, Enterobacter |
Table 1: Patient demographics, wound diagnosis and infection markers.
All patients satisfied the pre-requisites requirement of ankle-brachial index (ABI) > 0.8, toe-brachial index (TBI) > 0.7 and at least one pulse palpable. (Table I)
One wound was over the 5th metatarsal bed (post 5th ray amputation), one on the dorsum of the foot, one on the sole of the foot, one over the right tendoachilles region and one over the right calf. (Table I)
All ulcers were classified as Grade 2, according to Wagner-Meggitt Wound Classification. [19,20] (Table I)
Table II showed the V.A.C. Ulta settings for the patients. A pressure of -125mmHg was applied to all 5 wounds, at Continuous Mode, with 4 hours of negative pressure suction at -125mmHg and 10 minutes of soak at -25mmHg. (Table II) For all patients, the topical wound solution used was Normal Saline (Table II) The volume of solution used per instillation as indicated by fill assist ranged from 6-15ml. (Table II) The frequency of V.A.C. VeraFlo dressing change was every 72 – 96 hours. Wounds were administered V.A.C. VeraFlo therapy for an average of 8 days (range, 5-12) (Table II). There was an average of 2 V.A.C. Ulta dressing changes (range 1-3) per patient in the study. (Table II)
| Settings for VAC therapy | Frequency of VAC dressing change (h) | Days on VAC Ulta | Number of VAC Ulta dressing changes | ||||
| Negative pressure (mmHg) | Mode of application | Solution | Volume of solution per instillation (cc) | Total volume of solution used (cc) | |||
| -125 | Continuous, 4 hours VAC, 10 mins soak | Normal Saline | 6 | 432 | 72 - 96 | 12 | 3 |
| -125 | Continuous, 4 hours VAC, 10 mins soak | Normal Saline | 6 | 432 | 72 - 96 | 12 | 3 |
| -125 | Continuous, 4 hours VAC, 10 mins soak | Normal Saline | 15 | 450 | 72 | 5 | 1 |
| -125 | Continuous, 4 hours VAC, 10 mins soak | Normal Saline | 10 | 240 | 96 | 4 | 1 |
| -125 | Continuous, 4 hours VAC, 10 mins soak | Normal Saline | 12 | 504 | 96 | 7 | 2 |
Table 2: V.A.C. VeraFlo therapy settings and duration.
Table III illustrated the decrease in wound dimension and final outcome of the wounds for all patients. There was decrease in wound dimension before SSG was performed in all five patients. The average decrease in size was about 27.16%. (Range 25 – 29.5%) There was 100% take of the skin grafts with complete healing of the wound in all cases.
| Decrease in wound size before SSG/cm2 | % Decrease before SSG | Final outcome | % healed |
| 6.5 | 25 | Split-skin graft | 100 |
| 3.1 | 29.5 | Split-skin graft | 100 |
| 21.7 | 28 | Split-skin graft | 100 |
| 13 | 25 | Split-skin graft | 100 |
| 13 | 28.3 | Split-skin graft | 100 |
Table 3: Decrease in wound size, final outcome of wound & percentage of healing.
Case Study 1
A 79-year-old Chinese male presented with an ulcer post-debridement, abscess right tendoachilles region. Risk factors associated with healing consisted of a 10-year history of Type II Diabetes Mellitus, Hyperlipidemia, Hypertension Chronic Renal Failure, Chronic Obstructive Pulmonary Disease and Benign Prostatic Hyperplasia. The patient had previously undergone 3 surgical wound debridements. Both pulses were palpable, with an ABI and TBI reading of 1.15 and 0.8 respectively. The ulcer grade was given a Wagner Grade of 2. The markers of healing included 7% for HbA1C, 9.8 for haemoglobin count and 33 for albumin level. The markers of infection were 7.55 for WBC, 117 for CRP and 55 for ESR. A test for culture and sensitivity indicated that the following microorganisms were present: "E.coli, Morganella and Enterobacter" The patient was given intravenous Piptazo and surgical wound debridement followed by the application of V.A.C. Ulta dressing. After 2 cycles of instillation, the nature of the fluid in the instillation was clean. VAC instillation therapy was stopped. Tissue was taken from the wound and sent for culture and sensitivity. The wound was then treated with VAC without instillation. The culture result was negative. A split-skin graft was then carried out after 1 week. The wound area decreased by 28.3% before split-skin graft. Photos of the wound progression are included in Figure. 4.
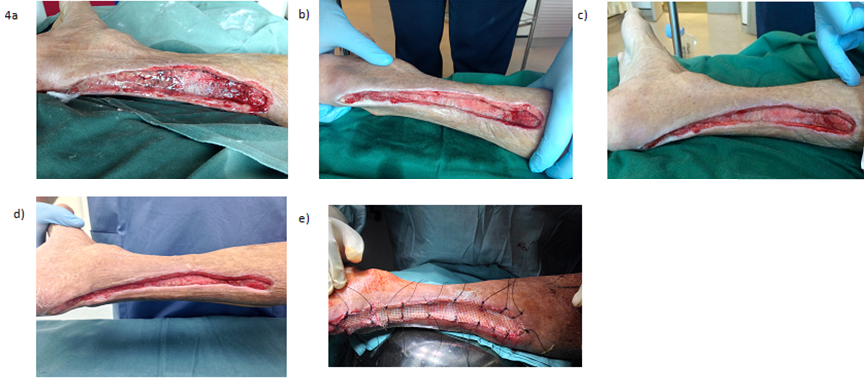
Figure 4: (a) Right Tendoachilles wound, before application of V.A.C. Ulta,
day past-operatively (b) During 3 Veraflotherapy, day 11 past-operatively (c)
During V.A.C. Veraflo therapy, day 13 postoperatively (d) End of V.A.C. Veraflotherapy,
day 14 past-operatively (e) Wound closed by split-skin graft
Case Study 2
A 51-year-old Indian male presented with an ulcer post-debridement, abscess dorsum right foot. Risk factors associated with healing consisted of a history of Type II Diabetes Mellitus, Hyperlipidemia and Hypertension. The patient had previously undergone a debridement of the right foot. Both pulses were palpable, with ABI and TBI reading of 1.18 and 0.9 respectively. His ulcer grade was given a Wagner Grade of 2. The markers of healing included 16.2% for HbA1C, 13.1 for haemoglobin count and 34 for albumin level. The markers of infection were 10.91 for WBC, 22 for CRP and 67 for ESR. A test for culture and sensitivity indicated that the following microorganism was present: Methicillin-sensitive staphylococcus aureus. The patient was given intravenous Piptazo and surgical wound debridement. This was followed by the application of V.A.C. Ulta dressing. After 3 cycles of instillation, the nature of the fluid in the instillation was clean. VAC instillation therapy was stopped. Tissue was taken from the wound and sent for culture and sensitivity. The wound was then treated with VAC without instillation. The culture result was negative. A split-skin graft was then carried out and intravenous antibiotics were removed after 12 days. The wound area decreased by 25% before split-skin graft. Photos of the wound progression are included in Figure: 5.
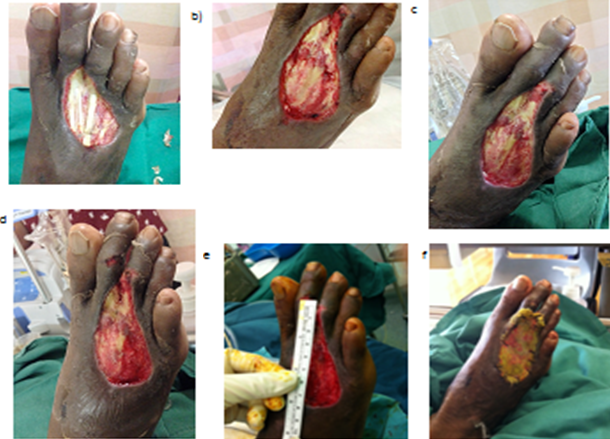
Figure 5: (a) Right dorsum ulcer, upon application of V.A.C. Ulta, day 5 post-operatively (b)
During V.A.C. VeraFlo therapy, day 8 post-operatively (c) During V.A.C. VeraFlo therapy, day
12 post-operatively (d) During V.A.C. VeraFlo therapy, day 14 post-operatively (e) End of
V.A.C. VeraFlo therapy, day 18 post-operatively (f) Wound closed by split-skin graft.
Discussion
V.A.C. VeraFlo Therapy has been shown by several studies to facilitate wound healing. An evolvement from the NPWT system, NPWTi allows for intermittent instillation of solutions into the wound. It provides a controlled, protected environment for the cleansing of wounds, protecting from external contamination sources while allowing for instillation of topical wound cleansers and removing infectious material.
Reticulated open-cell foam dressing
An advantage of V.A.C. VeraFlo Therapy is the usage of the new reticulated open-cell foam (ROCF) dressing that is specifically designed for instillation. Lessing., et al. [21] compared the new ROCF-V dressing, V.A.C. VeraFlo Dressing and the traditional ROCF dressing (ROCF-G), and revealed that ROCF-V is stronger than ROCF-G under tension and tear loading. ROCF-V was shown to be less hydrophobic than ROCF-G dressings. Under wet conditions, ROCF-V absorbs more fluid and shows less pressure drop than ROCF-G, suggesting ROCF-V to be better suited for use in NPWTi.
An advantage of V.A.C. VeraFlo Therapy is the usage of the new reticulated open-cell foam (ROCF) dressing that is specifically designed for instillation. Lessing., et al. [21] compared the new ROCF-V dressing, V.A.C. VeraFlo Dressing and the traditional ROCF dressing (ROCF-G), and revealed that ROCF-V is stronger than ROCF-G under tension and tear loading. ROCF-V was shown to be less hydrophobic than ROCF-G dressings. Under wet conditions, ROCF-V absorbs more fluid and shows less pressure drop than ROCF-G, suggesting ROCF-V to be better suited for use in NPWTi.
Type of instillation solutions
VAC Ulta can also be used with various types of topical wound solutions such as Dakin’s Solution, Microcyn antiseptic solution [9], 1% lidocaine in normal saline [17], Polyhexanide [15] and antibiotic solutions including Bacitracin [16], Vancomycin, Gentamycin, Tobramycin [17] and Polymyxin [16]. In our study the instillation consisted of normal saline only. We were reluctant to use local antibiotic perfusion as this could cause hypersensitivity. Anaphylaxis has been reported in patients who received Bacitracin irrigation [22]. Theoretically, local antibiotic perfusion might also cause development of antibiotic resistance.
VAC Ulta can also be used with various types of topical wound solutions such as Dakin’s Solution, Microcyn antiseptic solution [9], 1% lidocaine in normal saline [17], Polyhexanide [15] and antibiotic solutions including Bacitracin [16], Vancomycin, Gentamycin, Tobramycin [17] and Polymyxin [16]. In our study the instillation consisted of normal saline only. We were reluctant to use local antibiotic perfusion as this could cause hypersensitivity. Anaphylaxis has been reported in patients who received Bacitracin irrigation [22]. Theoretically, local antibiotic perfusion might also cause development of antibiotic resistance.
We have found Normal Saline to be just as effective in facilitating wound healing as the solutions above.
V.A.C. VeraFlo therapy has been shown to encourage faster wound closure. A pilot study conducted by Gabriel., et al. [18] of 15 patients with complex infected wounds treated with NPWTi using culture-specific systemic antibiotics compared to a retrospective control of 15 patients treated with moist gauze wound care found that patients with NPWTi achieved wound closure sooner. (13.2 ± 6.8 vs. 29.6 ± 6.5 days, p<0.001). In our study, patients treated with VAC VeraFlo therapy achieved wound closure with an average of 8 days. (Range: 4-12 days).
A study by Timmers., et al. [11] found that the usage of NPWTi can also reduce the need for repeated surgical interventions. The study evaluated the clinical outcome of 30 patients diagnosed with osteomyelitis treated with debridement followed by NPWTi using polyhexanide. In our study, patients with diabetic foot wounds treated with V.A.C. VeraFlo therapy did not require any further surgical procedure after the end of the therapy. All 5 cases ended with split-skin grafting with complete healing of the wounds.
V.A.C. VeraFlo therapy is also able to control bacterial infection in a wound. In the study performed by Schintler., et al. [10], infection was controlled for all 15 patients with skin and soft tissue infection treated with NPWTi. In another study conducted by Timmers., et al. [11], recurrence infection rate was 10% for 30 patients with osteomyelitis treated with NPWTi compared to 58.5% for the control group who received standard care. In our study, wound culture and sensitivity were found to be positive for micro-organisms for all wounds at the start of V.A.C. VeraFlo therapy. All 5 wounds showed clearance of bacterial infection with healthy granulation at the end of VAC VeraFlo therapy.
Bernstein and Tam [16] reported a study of 5 case studies on the healing of diabetic foot wounds. All 5 cases were diabetic foot infections - 1 on plantar of foot, 1 on metatarsal head, 1 on ray amputation wound, 1 on lateral border of foot, 1 on hallux of foot. Vascularity of the wound was determined by non-invasive vascular testing or a Doppler examination, but no specific values were given. Our work was also on 5 case studies on the healing of 5 diabetic foot ulcers – 1 on dorsum, 1 on ray amputation wound, 1 on calf, 1 on plantar (non-weight bearing portion of the sole of the foot), 1 on tendo-achilles region. In all 5 cases, the vascularity of the foot was good with at least one palpable pulse and an ABI of > 0.8 and a TBI of > 0.7.
In Bernstein and Tam’s paper, V.A.C. Ulta was used only for part of the wound treatment, and the ulcer left to heal using other dressings. Patients were put on V.A.C Ulta for an average of 6.2 days and then discharged with a treatment plan comprising of dressings or contact casting until full healing was achieved in an average of 9.3 weeks. In Wolvos [17] 2004 study of 5 cases, 3 of which had diabetic foot wounds, V.A.C Ulta was also used only for part of the wound treatment. NPWTi was stopped when wound was decided to be suitable for treatment with local wound care alone. It is difficult to conclude how much healing is due to VAC Ulta and how much is contributed by dressings or contact casting applied. However, in our series, V.A.C. Ulta was used till the instillation fluid was found to be clean. It was stopped and tissue from the wound was sent for culture and sensitivity. The wound was then treated with VAC without instillation. Upon confirmation of negative culture from the wound, split-skin grafting was performed. The healing of all 5 cases in our study can be attributed to the use of V.A.C. Ulta Veraflo alone.
Conclusion
This is a study of 5 cases with diabetic foot ulcers treated with V.A.C. Ulta and V.A.C. VeraFlo. All 5 cases healed in an average of 8 days without the need for further debridement. Culture and sensitivity showed microbial clearance as well. However, a major limitation of this study is the small cohort size and the lack of randomised controls. Further studies with controls are needed to evaluate the effectiveness of V.A.C. VeraFlo with Instillation compared to conventional dressings in the healing of diabetic foot wounds.
Acknowledgements
The authors would like to thank KCI, Singapore for sponsoring the V.A.C. dressings for all 5 patients in this study.
Conflict of interest
The authors would like to declare that there is no conflict of interest. No grant has been obtained from KCI, Singapore.
The authors would like to declare that there is no conflict of interest. No grant has been obtained from KCI, Singapore.
KCI was not involved in the data collection, analysis or write-up of the paper and will not be given editing rights to the paper. No benefits in any form will be received by KCI, Singapore.
References
- International Diabetes Federation. Diabetes: a global emergency. In: IDF Diabetes Atlas, 7th ed. 2015. Web. 15 May, 2016.
- International Working Group on the Diabetic Foot. Diabetes: The Epidemic of the 21st Century. 2011.
- Lee HJ., et al. “Negative pressure wound therapy for soft tissue injuries around the foot and ankle”. Journal of Orthopaedic Surgery and Research 4 (2009): 14.
- Blume PA., et al. “Comparison of negative pressure wound therapy using vacuum-assisted closure with advanced moist wound therapy in the treatment of diabetic foot ulcers: a multicenter randomized controlled trial”. Diabetes Care 31 (2008): 631-636.
- Vuerstaek JD., et al. “State-of-the-art treatment of chronic leg ulcers: A randomized controlled trial comparing vacuum-assisted closure (V.A.C.) with modern wound dressings”. Journal of Vascular Surgery 44 (2006): 1029-1038.
- Armstrong DG and Lavery LA. “Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial”. Lancet 366 (2005): 1704-1710.
- McCallon SK., et al. “V.A.C.uum-assisted closure versus saline-moistened gauze in the healing of postoperative diabetic foot wounds”. Ostomy Wound Manage 46 (2000): 28-32.
- Rycerz A., et al. “V.A.C.Ulta™ NPWT System Made Easy”. In: Wounds International. 2015. Web. 15 May, 2016.
- Wolvos T. “The use of negative pressure wound therapy with an automated, volumetric fluid administration: an advancement in wound care”. Wounds 25.3 (2013): 75-83.
- Schintler MV., et al. “The impact of V.A.C. instill in severe soft tissue infections and necrotizing fasciitis”. Infection 37 (2009): 31-32.
- Timmers MS., et al. “Negative pressure wound treatment with polyvinyl alcohol foam and polyhexanide antiseptic solution instillation in posttraumatic osteomyelitis”. Wound Repair Regen 17 (2009): 278-286.
- Leffler M., et al. “Instillation therapy and chronic osteomyelitis-preliminary results with the V.A.C. Instill therapy”. Infection 37 (2009): 24-30.
- Koster G. “Management of early periprothetic infections in the knee using the vacuum-instillation therapy”. Infection 37 suppl 1 (2009): 18-20.
- Lehner B., et al. “Application of V.A.C Instill ® therapy in case of periprosthetic infection in hip arthroplasty”. Infection 37 (2009): 13-17.
- Lehner B., et al. “First experiences with negative pressure wound therapy and instillation in the treatment of infected orthopaedic implants: a clinical observational study”. International Orthopaedics 35 (2011): 1415-1420.
- Bernstein BH. and Tam H. “Combination of subatmospheric pressure dressing and gravity feed antibiotic instillation in the treatment of post-surgical diabetic foot wounds: A case series”. Wounds 17 (2005): 37-48.
- Wolvos T. “Wound instillation--the next step in negative pressure wound therapy. Lessons learned from initial experiences.” Ostomy Wound Manage 50 (2004): 56–66.
- Gabriel A., et al. “Negative pressure wound therapy with instillation: a pilot study describing a new method for treating infected wounds”. International Wound Journal 5 (2008): 399-413.
- Meggitt B. “Surgical management of the diabetic foot”. British Journal of Hospital Medicine 16 (1976): 227-232.
- Wagner FW. “The dysvascular foot: a system for diagnosis and treatment”. Foot and Ankle 2 (1981): 64-122.
- Lessing C., et al. “Negative pressure wound therapy with controlled saline instillation (NPWTi): dressing properties and granulation response in vivo”. Wounds 23 (2011): 309-319.
- Antevil JL., et al. “Intraoperative anaphylactic shock associated with bacitracin irrigation during revision total knee arthroplasty: a case report”. Journal Bone Joint Surgery America 85 (2003): 339-342.
Citation:
Aziz Nather., et al. “Vacuum-Assisted Closure Ulta with Veraflo Instillation for the Healing of Diabetic Foot Wounds”. Orthopaedic
Surgery and Traumatology 1.1 (2016): 10-18.
Copyright: © 2016 Aziz Nather., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.