Research Article
Volume 1 Issue 6 - 2017
Direct Anterior Approach versus Posterior Approach for Total Hip Arthroplasty; Short-Term Results of Functional Assessment in the Early Phase of Recovery
1Department of Trauma and Orthopaedics, the Royal Stoke University Hospital, Newcastle Road, England, UK
2Consultant Trauma and Orthopaedic Surgeon, the Royal Stoke University Hospital, Newcastle Road, England, UK
2Consultant Trauma and Orthopaedic Surgeon, the Royal Stoke University Hospital, Newcastle Road, England, UK
*Corresponding Author: Dr. Haroon Majeed, MBBS; MRCS; MSc; FEBOT; FRCS (Tr & Orth)
Specialist Registrar, Department of Trauma and Orthopaedics, The Royal Stoke University Hospital, Newcastle Road, England, UK.
Received: October 17, 2017; Published: October 20, 2017
Abstract
Introduction: The objective of our study was to assess the outcome of primary total hip arthroplasty performed using direct anterior approach and to compare them with posterior approach.
Material and Methods: Between March 2013 and March 2015, the senior author performed 20 primary total hip arthroplasty through direct anterior approach. We reviewed their results and compared them with equal number of patients who underwent total hip arthroplasty through posterior approach, operated by the same surgeon. Data included demographic details, body mass index, duration of operative time and hospital stay, assessment of pain scores and functional scores and hemoglobin levels.
Results: In direct anterior approach group, 85% (17/20) patients went home within 3 days compared to 55% (11/20) in posterior approach group. Average duration of operative time in direct anterior group was significantly longer (123 minutes) than in posterior approach group (74 minute, p = 0.01). Average follow up was 12 months and 14 months respectively in each group. Average BMI was 26.3 and 30 respectively in each group. Harris Hip Scores and Oxford Scores were clinically better in both groups but were not significantly different. There was significant reduction in the use of analgesia in patients in direct anterior approach group within 4 weeks after surgery compared to posterior approach group (p = 0.02).
Conclusion: Total hip arthroplasty through direct anterior approach in our early experience has provided clinically better pain scores, functional scores and physical abilities in early phase of recovery and associated with significantly less analgesia requirements within first month after surgery.
Keywords: Hip arthroplasty; Direct anterior approach; Minimally invasive surgery; Posterior approach; Internervous approach
Introduction
An ideal surgical approach for total hip arthroplasty (THA) should aim to achieve reduced operative invasion, better operative accuracy, and early functional recovery [1]. However, there is an endless debate and a lack of consensus among the hip surgeons to agree on such an ideal approach. Total hip arthroplasty through the direct anterior approach (DAA), was first described by Heuter in 1885, was later referred to as the Heuter-Volkmann approach and was modified into the Smith-Petersen approach for hip hemiarthroplasty [2,3]. Total hip arthroplasty through the direct anterior approach was first performed by Robert Judet in 1947 [4]. Light and Keggi described a further modification of the Smith-Peterson approach in 1980, such that the tensor fasciae lata was split longitudinally to provide the desired exposure with or without performing trochanteric osteotomy if necessary [5]. In the current practice, primary total hip arthroplasty through the DAA is performed by using the distal half of the Smith-Peterson approach.
The anterior approach through the internervous and intermuscular plane between the tensor fascia lata (laterally), and sartorius and rectus femoris (medially), has been described as the most direct and simple of all surgical approaches to the hip joint [5]. This approach aims to preserve the posterior structures, along with abductor muscle attachments to the greater trochanter, which are important to prevent dislocation and facilitate early functional recovery [6-8]. However, the direct anterior approach is technically challenging and does have a significant learning curve. The surgeon needs to have a thorough familiarity with this approach to be able to perform total hip arthroplasty safely to achieve the desired results. We hypothesized that total hip arthroplasty through direct anterior approach provides better functional outcome in the early phase of recovery (within 6 weeks after surgery) as compared to posterior approach (PA).
Material and Methods
Between March 2013 and March 2015, the senior author (IDR) performed 20 primary total hip arthroplasties (18 patients) through the direct anterior approach. We retrospectively reviewed the results of these patients and compared them with primary total hip arthroplasties performed through posterior approach by the same surgeon. The same number of total hip arthroplasties (20 THAs in 19 patients) through PA was selected randomly from the operating list records during the same time period to avoid any bias.
Although there was no randomization carried out but patients were selected randomly for the direct anterior approach at the time of preoperative assessment. The operative notes were reviewed to identify all the patients who had their hip surgeries done through the DAA and equal numbers of patients were selected who had their THAs performed through the posterior approach. Two groups were formed; each with 20 hip arthroplasties; the DAA group (18 patients) and the PA group (19 patients).
Further data were collected through the case notes and included demographic details, body mass index (BMI), type and material of the prostheses, duration of anaesthesia and surgery, in-patient hospital stay, preoperative and postoperative pain scores and functional assessment using Harris Hip Score and Oxford Score, which were routinely obtained before surgery and 6 weeks after surgery, and preoperative and postoperative haemoglobin (Hb) levels to assess the drop in Hb level. All the patients were operated on in laminar flow theatres. The direct anterior approach was performed in supine position on a standard orthopaedic operating table. The posterior approach was performed in lateral position using the standard technique.
Enhanced recovery protocol was used in all the patients in both the groups using a combination of 30ml of Bupivacaine with Adrenaline, 30mg of Ketorolac (Toradol) and 30ml of normal saline, infiltrated around the joint capsule and soft tissues. Single closed suction drain (size 14) was used in all the patients. Same intraoperative and postoperative routine was followed in all the patients for antibiotic prophylaxis (1 dose of intravenous Flucloxacillin and Gentamicin) and venous thromboembolic prophylaxis (Riveroxaban, oral 10mg for 5 weeks and graduated compression stockings for 6 weeks). Routine blood tests (full blood count, renal profile) along with plain radiographs were obtained in all the patients on the first day after surgery. Early mobilization was encouraged in all the patients, with daily in-patient assessment by physiotherapists. Patients were discharged home when their pain level was under control and they were considered safe after their mobility assessment. Postoperative radiographs were reviewed to assess the inclination angles of acetabular components.
Statistical Analysis
Demographics of the two groups were compared using Fisher's Exact test (two-tailed) for categorical variables and Student’s t-tests (two-tailed) for numerical variables. BMI, length of hospitalization, operative duration and drop in Hb were analyzed using Student’s t-test. The proportion of subjects able to walk to unlimited distances and reduction in analgesia requirements were evaluated using a two-tailed Fisher's exact test. VAS pain scores were compared preoperatively, at 6 weeks postoperatively and at the latest follow up using t-test. Functional assessment using Harris Hip Scores and Oxford Scores was performed preoperatively and at 6 weeks postoperatively using Mann-Whitney test (two-tailed). Cup inclination on postoperative radiographs was compared using t-tests. Stem orientation was compared at 6 weeks with Fisher's Exact test. In all tests, a P-value of less than 0.05 was considered statistically significant.
Demographics of the two groups were compared using Fisher's Exact test (two-tailed) for categorical variables and Student’s t-tests (two-tailed) for numerical variables. BMI, length of hospitalization, operative duration and drop in Hb were analyzed using Student’s t-test. The proportion of subjects able to walk to unlimited distances and reduction in analgesia requirements were evaluated using a two-tailed Fisher's exact test. VAS pain scores were compared preoperatively, at 6 weeks postoperatively and at the latest follow up using t-test. Functional assessment using Harris Hip Scores and Oxford Scores was performed preoperatively and at 6 weeks postoperatively using Mann-Whitney test (two-tailed). Cup inclination on postoperative radiographs was compared using t-tests. Stem orientation was compared at 6 weeks with Fisher's Exact test. In all tests, a P-value of less than 0.05 was considered statistically significant.
Surgical Technique (Direct Anterior Approach)
The patient was positioned supine on standard orthopaedic table without traction, with hip extension achievable during the procedure (approximately 25°). Both legs were prepared sterile and draped in standard manner. All these patients were operated with the help of a single assisting surgeon. No intraoperative image intensifier or traction devices were used. The initial landmark used was a line joining the anterior superior iliac spine (ASIS) and fibular head. The starting point of the incision was 3 cm posterior and 2 cm distal to ASIS, 20° angulated posteriorly to the line already drawn, 8 to 10 cm in length (Figure 1).
The patient was positioned supine on standard orthopaedic table without traction, with hip extension achievable during the procedure (approximately 25°). Both legs were prepared sterile and draped in standard manner. All these patients were operated with the help of a single assisting surgeon. No intraoperative image intensifier or traction devices were used. The initial landmark used was a line joining the anterior superior iliac spine (ASIS) and fibular head. The starting point of the incision was 3 cm posterior and 2 cm distal to ASIS, 20° angulated posteriorly to the line already drawn, 8 to 10 cm in length (Figure 1).
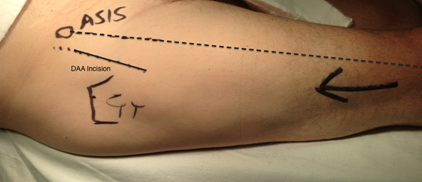
Figure 1: Lateral aspect of right thigh in supine position showing the surface markings for surgical incision for direct anterior approach.
This incision corresponds to the middle of the bulge of tensor fascia lata (TFL) muscle. This modification of incision was made by the senior author in order to prevent injury to lateral femoral cutaneous nerve of the thigh. The fascia of the TFL was incised in line with the skin incision. Blunt finger dissection is considered most efficient at this stage to identify the passage between the tensor muscle laterally and the sartorius muscle medially. The perimysium of the underlying rectus femoris muscle was then incised and the muscle was retracted medially to expose the hip capsule.Retractors were placed along the lateral and medial hip capsule to retract the tensor and gluteus minimus laterally and retract the sartorius and rectus femoris muscles medially. This muscle retraction brings the ascending branches of the lateral femoral circumflex vessels into view at the distal end of the wound, which were clamped and ligated.
The anterior capsule can either be excised or opened but the senior author excised the capsule in majority of the cases. The medial and lateral retractors were then repositioned intra-articular around the femoral neck, protecting the soft tissues from the oscillating saw. The neck was cut in situ by double osteotomy to extricate a wafer of bone, thereby decompressing the joint and facilitating removal of the femoral head using a corkscrew. The retractors were repositioned to improve the exposure to the acetabulum. A blunt-tipped retractor was placed outside the acetabular labrum posteriorly. A sharp-tipped retractor was placed around the anteroinferior acetabular wall. The acetabulum was then reamed in a standard fashion with an offset reamer attachment under direct vision. The cup and liner were impacted under direct visualization, taking care to maintain correct orientation.
By the use of the table, the leg was then extended at the hip approximately 25° and externally rotated and adducted by bringing it in figure of ‘4’. To achieve sufficient adduction of the leg is of paramount importance at this stage. Care was taken to mobilize the proximal femur anteriorly by appropriate soft tissue release, to avoid entrapment of the tip of the greater trochanter behind the posterior acetabular rim, thereby avoiding risk of fracture. Exposure of the femur was maintained with a double-pronged retractor placed posterior to the greater trochanter. The femoral canal was prepared in routine fashion, and trial reduction was performed for assessing stability and leg length measurement. Definitive implants were then inserted under direct visualization. The muscles were then allowed to return to their respective anatomic positions, leaving only the fascia and skin for closure. The retractors and implant introducers used for the DAA are shown in Figure 2.
Results
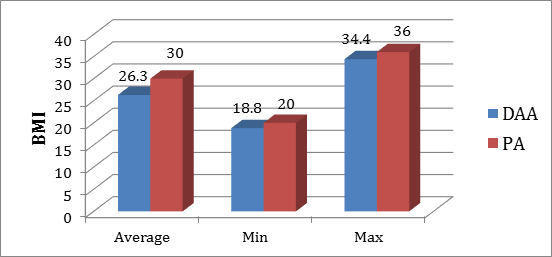
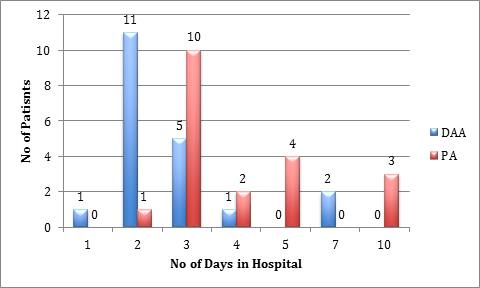
Both the groups had comparable distribution of gender and age (Figure 3). Table 1 summarizes the demographic data of the two groups. The average body mass index (BMI) was found to be lower (p = 0.02) in the DAA group (Figure 4). This was, however, not taken in to account as a selection criteria when selecting the patients for either approach at the time of their preoperative assessment. Patients in DAA group were discharged significantly earlier than the patients in PA group (P = 0.001). The average length of hospital stay was 2.8 days in the DAA group (1 to 7 days) and 4.4 days in the PA group (2 to 10 days) (Figure 4, p = 0.005). It is important to note that 55% patients (11/20) in the DAA group were discharged from the hospital at 2nd postoperative day, whereas in the PA group, 15% patients (3/20) were discharged within first 2 days (p = 0.001).
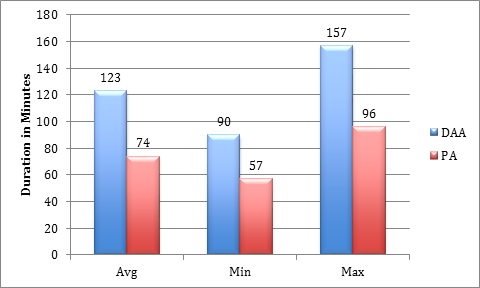
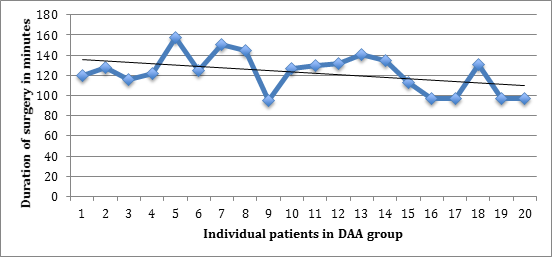
Most patients in both the groups had their surgery performed under general anaesthesia with only a small number of patients having had spinal anaesthesia or a combination of the two (Table 1). Average duration of the operative time in the DAA group was 123 minutes (90 to 157) and in the PA group was 74 minute (57 to 96), which was found to be significantly longer in the DAA group (p < 0.00001). It was interesting to note that there was a trend towards a gradual reduction in the operative duration with progressive learning curve in the DAA group (Figures 5,6). Average duration of follow up was 13 months in the DAA group and 15 months in the PA group.
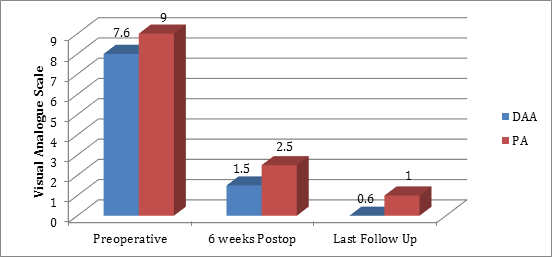
Assessment of VAS pain score showed significantly worse pain scores in the PA group at the time of their preoperative assessment (p = 0.006). However, at 6 weeks after surgery (p = 0.41) and on the last follow up (p = 0.32), pain scores were not significantly different (Figure 7). The requirement for analgesic medications reduced to none within 3 weeks after surgery in the DAA group, which was significantly earlier than PA group (p = 0.02).
| DAA | PA | |
| Male | 12 | 11 |
| Female | 8 | 9 |
| Average Age (years) | 64.5 | 64 |
| General Anaesthetic | 17 | 15 |
| Spinal Anaesthetic | 1 | 2 |
| GA + Spinal | 2 | 3 |
| Follow up (months) | 13 (8-18) | 15 (10-26) |
| Osteoarthritis | 14 | 14 |
| Rheumatoid arthritis | 1 | 2 |
| Avascular necrosis | 4 | 4 |
| Dysplasia | 1 | 0 |
Table 1: Demographic data in both the groups.
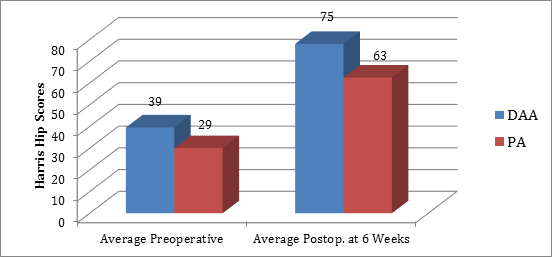
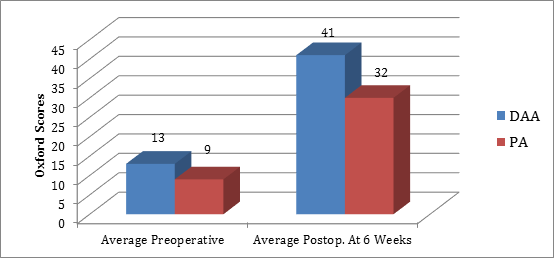
Preoperative assessment of functional scores showed an average Harris Hip Score of 39 in the DAA group and 29 in the PA group (p = 0.002). After surgery at six weeks stage, the average score improved to 75 and 63 in both the groups respectively (p = 0.03). These scores were found significantly better in the DAA group both pre and postoperatively (Figure 8). All the patients in both the groups had successful outcomes of their hip replacements based on the criteria described by Marchetti., et al. as per functional assessment using Harris Hip Score (9). Before surgery, the average Oxford Score was 13 in DAA group and 9 in PA group. At 6 weeks after surgery, the scores were clinically and statistically better in the DAA group than the PA group (41 vs. 32, p = 0.002) (Figure 9).
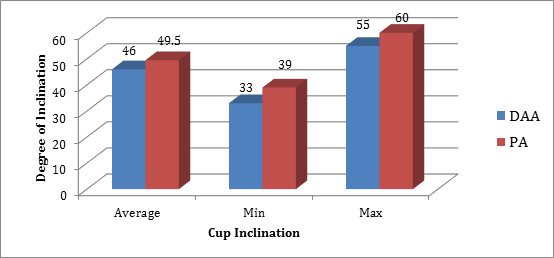
The average cup inclination in the DAA group was measured to be 46° (33° to 55°) compared to 49.5° (29° to 60°) in PA group (Figure 10), showing no significant difference (p = 0.06). The DAA group had 14 cups inserted within the safe zone of Lewinnek compared to 10 cups in the PA group (p = 0.6) (10). The average drop in Hb level immediately after surgery was comparable in the two groups (DAA: 39 g/L vs. PA: 37 g/L, p = 0.6) (Table 2). Only one patient in the DAA group required blood transfusion because of being symptomatic due to low Hb after surgery, while in the PA group, none of the patients required transfusion.
Two patients in the DAA group and three in the PA group had postoperative complications. In the DAA group, 1 patient had persistent drain site leakage after drain removal, which settled gradually with regular dressings and did not require surgical intervention. The second patient developed acute renal impairment (background of previous renal impairment), which improved with intravenous fluid management without any further consequences.
However, in these two patients the duration of hospital stay was prolonged due to these issues. In the PA group, two patients had periprosthetic fractures, one of which was identified intraoperatively and fixed with cerclage wires. The second patient was found to have an undisplaced periprosthetic fracture on routine postoperative radiographs but it did not require any further intervention and the patient was mobilized with protected weight bearing for 6 weeks with no further consequences. One patient in this group had superficial wound infection, which settled with oral antibiotics within one week and did not require any further surgical intervention. There have been no implant failure or dislocation in any of these patients in either group. The types of implants used in both groups are described in Table 3.
| DAA | PA | |
| Avg. Preoperative Hb (g/L) | 143 | 139 |
| Avg. Postoperative Hb (g/L) | 104 | 103 |
| Avg. drop in Hb (g/L) | 39 | 37 |
Table 2: Haemoglobin levels in both the groups.
| Type of Implants | DAA | PA | |
| Implants | Polar/R3 (Smith & Nephew) | 18 | 1 |
| Corail/Pinnacle (Depuy) | 0 | 17 | |
| Short Modular Femur (SMF) | 2 | 2 | |
| Bearing Surfaces | Ceramic/Ceramic | 18 | 15 |
| Polyethelene/Ceramic | 1 | 5 | |
| Polyethelene/Oxinium | 1 | 0 | |
| Head Size | 36 mm | 15 | 11 |
| 32 mm | 5 | 8 | |
| 28 mm | 0 | 1 | |
Table 3: Implants used in both the groups.
On the latest follow up, 16 patients in the DAA group reported that they were able to walk to unlimited distances without any limitation, whereas 8 patients in the PA group reported similar abilities (p = 0.2). Thirteen patients in the DAA group have been able to squat after their surgery and the other 5 have not tried to squat. Squatting is however, not advisable after undergoing total hip replacement through posterior approach due to the concern of dislocation.
One-third patients in each group reported the presence of paraesthesia around the scar, however, this was not found troublesome by any patient and half of these patients in each group reported gradual improvement in sensations 6 to 12 months after surgery. When examined on the last follow up, all the patients in the DAA group had negative Trendelenburg test, while in the PA group 4 patients had a positive test (p = 0.11). Surgical and postoperative data is summarized in Table 4.
| Variables (Mean ± Standard Deviation) | DAA | PA | P-value |
| Average BMI | 26.3 ± 3.86 | 30 ± 5.10 | 0.02 |
| Discharge on day 2 | 11 (55%) | 3 (15%) | 0.0001 |
| Discharge on day 3 | 17 (85%) | 11 (55%) | 0.06 |
| Avg. length of hospital stay (days) | 2.8 ± 1.57 | 4.4 ± 2.68 | 0.005 |
| Duration of operative time (minutes) | 123 ± 19.3 | 74 ± 15.7 | <0.00001 |
| VAS pain score Avg. Preoperative 6 weeks after surgery Last follow up |
7.6 ± 1.70 | 9 ± 1.23 | 0.006 |
| 1.5 ± 2.27 | 2.5 ± 2.53 | 0.41 | |
| 0.6 ± 1.44 | 1 ± 2.18 | 0.32 | |
| Unlimited walking | 16 | 8 | 0.2 |
| No analgesia at 4 weeks | 16 | 4 | 0.02 |
| Trendelenburg +ve | 0 | 4 | 0.11 |
Table 4: Surgical and postoperative data.
Discussion
Some studies have compared the short-term outcomes of hip arthroplasties through the direct anterior approach and the posterior approach. A prospective randomized controlled trial by Barrett., et al. compared these two approaches, and reported that the benefits of the DAA were specifically more marked in the early phase of recovery after surgery. Their study showed lesser pain score and better walking distance on first and second days after surgery, as well as significantly better functional status and Harris Hip Scores at 6 weeks and 12 weeks after surgery [11]. Bhandari., et al. reported the outcomes of THA through the DAA performed across 9 hospitals in the United States, with a cohort of 1152 patients, and found an acceptable complication rate, low dislocation rate and rapid functional recovery [12]. Maffiuletti., et al. performed spatiotemporal gait analysis of the patients who underwent THA through the DAA and compared them with posterior approach. They reported that the patients operated through the posterior approach had significantly higher stiffness compared to the DAA group, however the pain scores and functional outcomes were similar in the two groups [13].
Bergin., et al. compared the biochemical markers of inflammation and muscle trauma (Creatine Kinase) in patients who underwent THA through these two approaches. They reported that there was significantly less muscle damage in patients who had surgery through the DAA as compared to surgery done through the posterior approach [14]. Nakata., et al. compared THA through the direct anterior approach with THA through minimally invasive posterior approach, and reported relatively faster postoperative recovery of functional status and gait after the direct anterior approach. Moskal also reported faster recovery, less muscle damage, and improved functional outcomes after THA performed through the DAA [15]. Vail., et al. and Berend., et al. have reported relative ease of placement of the components, less incidence of dislocation, preservation of hip abductors, less pain after surgery, and faster recovery of patients operated through the DAA [16, 17]. Studies have also reported that THA through the direct anterior approach has a learning curve for the operating surgeons [8,15]. Oinuma., et al. performed 116 THAs through the direct anterior approach and reported a gradual decrease in the duration of surgical time, with no intraoperative complications [18].
Many authors have described the relative safety of hip arthroplasty through the direct anterior approach [19-21]. However, one of the most specific concerns related to this approach is lateral thigh numbness associated with injury or neuropraxia of lateral femoral cutaneous nerve [8,22]. Some studies have reported high incidence of this complication, however, gradual resolution of symptoms has been described after 1 year of surgery without causing any functional limitations [24]. If appropriate care is taken in planning the incision and muscle layer dissection, the rate of this complication can be minimized.
Our results have shown similar outcomes to the previously available reports from North America and some other European countries. To our knowledge, this is the first report of early results of total hip arthroplasty through the direct anterior approach in the United Kingdom.
Undoubtedly, the DAA has a longer intraoperative duration compared to the standard and commonly used posterior approach, however, our patients have reported clinically and subjectively better functional scores and physical abilities in the early phase of recovery after their hip replacements through this approach. There was a noticeable and gradual reduction in the operative time as the experience of the operating surgeon and the assisting surgeons progressed. There has been significantly reduced analgesia requirement within first 3 to 4 weeks after surgery through this approach, adding further to an improved quality of life after a successful hip arthroplasty.
We had no procedure-related complications in this group of patients, indicating a safe approach. However, it has a progressive learning curve for the operating surgeon and the assisting team, along with the requirement of appropriate instrumentation. Our study had a few limitations. It started as a retrospective review, however, functional scoring was performed in a prospective manner. The records of intraoperative blood loss were not available for all the patients from their operative or anaesthetic notes, therefore were not included in the analysis of our results.
Conclusion
Our early experience of hip arthroplasties through the direct anterior approach has shown promising results with significantly less analgesia requirements and better clinical and functional recovery in the early phase of recovery, in comparison to the patients operated through the posterior approach. It is a safe option to perform hip arthroplasty with no major procedure-related complications and without causing major muscle trauma, however, it has a progressive learning curve and the surgeon’s familiarity at each step of this approach is critical. However, our results highlight a potential requirement for a prospective randomized controlled for more accurate assessment of the outcomes through different approaches used for hip arthroplasty.
Conflicts of Interest: ‘None’
Ethical standards statement
Being a retrospective study, it did not require informed consent of the patients or the permission from the local ethical committee. However, the figure 1, which shows intraoperative incision markings, was taken after an informed consent from the patient for this study.
Being a retrospective study, it did not require informed consent of the patients or the permission from the local ethical committee. However, the figure 1, which shows intraoperative incision markings, was taken after an informed consent from the patient for this study.
References
- Nakata K., et al. "A clinical comparative study of the direct anterior with mini-posterior approach: two consecutive series". The Journal of arthroplasty24.5 (2009): 698-704.
- M Smith-Petersen. "A new supra-articular subperiosteal approach to the hip joint". The American Journal of Orthopedics 15 (1917): 592-596.
- Smith-Petersen MN. "Approach to and exposure of the hip joint for mold arthroplasty". The Journal of bone and joint surgery American volume 31A.1 (1949): 40-46.
- Judet R and Judet J. "Technique and results with the acrylic femoral head prosthesis". The Journal of bone and joint surgery British volume 34-B.2 (1952): 173-180.
- Light TR and Keggi KJ. "Anterior approach to hip arthroplasty". Clinical orthopaedics and related research 152 (1980): 255-260.
- Bourne RB and Rorabeck CH. "Soft tissue balancing: the hip".The Journal of arthroplasty 17.4 Suppl 1 (2002): 17-22.
- DeWal H., et al. "Instability following total hip arthroplasty". American Journal of Orthopedics (Belle Mead NJ) 32.8 (2003): 377-382.
- Masonis JL and Bourne RB. "Surgical approach, abductor function, and total hip arthroplasty dislocation". Clinical orthopaedics and related research 405 (2002): 46-53.
- Marchetti P., et al. "Long-term results with cementless Fitek (or Fitmore) cups". The Journal of arthroplasty 20.6 (2005): 730-737.
- Lewinnek GE., et al. "Dislocations after total hip-replacement arthroplasties". The Journal of bone and joint surgery American volume 60.2 (1978): 217-220.
- Barrett WP., et al. "Prospective Randomized Study of Direct Anterior vs Postero-Lateral Approach for Total Hip Arthroplasty". The Journal of arthroplasty 28.9 (2013): 1634-1638.
- Bhandari M., et al. "Outcomes following the single-incision anterior approach to total hip arthroplasty: a multicenter observational study". The Orthopedic clinics of North America 40.3 (2009): 329-342.
- Maffiuletti NA., et al. "Spatiotemporal parameters of gait after total hip replacement: anterior versus posterior approach". The Orthopedic clinics of North America 40.3 (2009): 407-415.
- Bergin PF., et al. "Comparison of minimally invasive direct anterior versus posterior total hip arthroplasty based on inflammation and muscle damage markers". The Journal of bone and joint surgery American volume 93.15 (2011): 1392-1398.
- Moskal JT and Capps SG. "Acetabular component positioning in total hip arthroplasty: an evidence-based analysis". The Journal of arthroplasty 26.8 (2011): 1432-1437.
- Vail TP., et al. "Approaches in primary total hip arthroplasty". The Journal of bone and joint surgery American volume 91(Suppl 5) (2009): 10-12.
- Berend KR., et al. "Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty". The Journal of bone and joint surgery American volume 91 (Suppl 6) (2009): 107-120.
- Oinuma K., et al. "Total hip arthroplasty by a minimally invasive, direct anterior approach". Operative Orthopadie und Traumatologie 19.3 (2007): 310-326.
- Matta JM., et al. "Single-incision anterior approach for total hip arthroplasty on an orthopaedic table". Clinical orthopaedics and related research 441 (2005): 115-124.
- Kennon RE., et al. "Total hip arthroplasty through a minimally invasive anterior surgical approach". The Journal of bone and joint surgery American volume 85-A Suppl 4 (2003): 39-48.
- Rachbauer F. "[Minimally invasive total hip arthroplasty via direct anterior approach]". Der Orthopade 34.11 (2005): 1103-4, 1106-8, 1110.
- Smith TO., et al. "Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes". International orthopaedics 35.2 (2011): 173-184.
- Martin CT., et al. "A comparison of hospital length of stay and short-term morbidity between the anterior and the posterior approaches to total hip arthroplasty". The Journal of arthroplasty 28.5 (2013): 849-854.
- Goulding K., et al. "Incidence of lateral femoral cutaneous nerve neuropraxia after anterior approach hip arthroplasty". Clinical orthopaedics and related research 468.9 (2010): 2397-2404.
Citation:
Haroon Majeed and Ian dos Remedios. “Direct Anterior Approach versus Posterior Approach for Total Hip Arthroplasty;
Short-Term Results of Functional Assessment in the Early Phase of Recovery”. Orthopaedic Surgery and Traumatology 1.6 (2017): 203-
214.
Copyright: © 2017 Haroon Majeed and Ian dos Remedios. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.




































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.