Case Report
Volume 2 Issue 3 - 2018
Metal-Hypersensitivity (MHR) in Total Knee Arthroplasty: A Case Report
1Casa di Cura I Cedri, Largo Don Guanella, 1, 28073 Fara Novarese NO, Italy
2Undergraduate student at the University of Central Oklahoma
3Orthopedic Director, Associate Professor University of Milan
2Undergraduate student at the University of Central Oklahoma
3Orthopedic Director, Associate Professor University of Milan
*Corresponding Author: Villa Tiziano MD, Casa di Cura I Cedri, Largo Don Guanella, 1, 28073 Fara Novarese NO, Italy.
Received: June 27, 2018; Published: July 12, 2018
Abstract
Metal sensitivity after total joint arthroplasty has been of increased concern; the impact of a patient reported metal allergy on clinical outcomes is investigated. Patient-reported metal allergy is associated with decreased functional outcomes after TKA. Although total knee arthroplasty is a successful and cost-effective procedure, patient dissatisfaction remains as high as 50%. Postoperative residual knee pain after total knee arthroplasty, with or without crepitation, is a major factor that contributes to patient dissatisfaction. Up to 10% to 15% of patients with residual pain may have unexplained pain. Various etiologies have been implicated in residual pain, including low-grade infection, component malalignment with patellar malt racking, early aseptic loosening and hypersensitivity to metal or cement.
Keywords: TKA; Metal-Hypersensitivity in TKA; Revision TKA
Introduction
The use of metals in Orthopedics is widespread, and there has been increasing concern with regards to the possibility of developing cutaneous and systemic hypersensitivity reactions to constituent metals in implant devices. Although hypersensitivity reactions to metals are not common, they require evaluation and management when they do occur. Regrettably, there is an ostensible lack of accord in the field on the appropriate steps to evaluate, diagnose and manage patients with suspected metal hypersensitivity reactions [1]. Orthopedic implants are composed of nickel, cobalt, chromium, molybdenum, zirconium and/or titanium alloys, while stainless steel is used in fixed orthopedic devices such as screws/plates. As a cause of complication after joint replacement, metal allergy was first reported in 1966, with slowly increasing awareness and reported incidence.
While the association between metal implant failure and allergy is well documented, it remains a phenomenon that is relatively unpredictable, poorly understood and highly debated. Skin reactions caused by MHR include dermatitis reactions adjacent to and regionally adjacent to the implant site, generalized dermatitis, as well as erythema, generalized urticaria and cutaneous vacuities. Reactions occur following implantation of static implants as well as dynamic prostheses. Other adverse reactions including device failure, chronic inflammation, and pain, loosening of joint prostheses or re-stenosis of cardiac stents can also occur. In some cases, metallosis (metallic staining of the surrounding tissue), excessive periprosthetic fibrosis and muscular necrosis have also been reported [1,7].
With an aging population, clarifying the association between metal hypersensitivity reactions and implant failures bears enormous repercussions for health care costs, and avoids unnecessary morbidity in patients.
Case Report
A 69 years old male patient with both varus knees affected by medial osteoarthritis. No referred previous metal allergies. In June 2015 the patient underwent primary total knee replacement on the left knee, receiving a Postero-stabilized cemented total knee prosthesis Vanguard knee (Biomet) With a CoCrMo fixed tibial tray with no patellar resurfacing. The bone cement used was by Synimed (Synicem 1). The first postoperative follow-up after two months showed a patient free of pain with the following ROM: flexion-extension was 0°-140°.
The 14 months follow-up showed an asymptomatic patient, good clinical outcome of the left TKA, with negative CRP; the only suspicious factor was an elevated ESR and monocytes in the lab work up. Two years after first surgery, the patient started referring pain at the operated left knee. The radiological exam showed a normal radiological outcome after TKR; slight ossification of the medial collateral ligament and a moderate soft tissues swelling over the patella (Figure 1).
An ultrasonic examination confirmed an abundant articular effusion in the area underlying the quadriceps tendon with thicker synovial capsule. The skin was normal at that time of examination. In the further examination, the patch-test for nickel, cobalt, chromium and PMMA was made. There was no proved patient’s metal hypersensitivity to all tested elements. In the lab test, ESR was still elevated at 30 mm/h, but CRP showed a normal value. The performed two knee needle aspirations (each with 5-10 ml of synovial fluid) confirmed a negative result in the cultures form both aspirates.
As requested for medical clarification, a three-phase technetium bone scan was performed and resulted positive on the left knee. The biopsy, carried out 31 months after first implantation, of the periprosthetic tissues showed the following result: histopathologic analysis revealed periprosthetic tissue with diffuse synovial erosion and villonodular synovitis areas. Massive fibrosis with moderate lymphohistiocytic infiltrates were present in the periprosthetic tissues without any prosthetic dark-stained materials indicative of prosthetic wear and metallosis. No infection signs was present in the samples. As pain, swelling, reduced ROM continued to influence patients QDL, 31 months after primary surgery, we decided to re-operate the patient; putative diagnosis of allergic reaction to the primary implant.
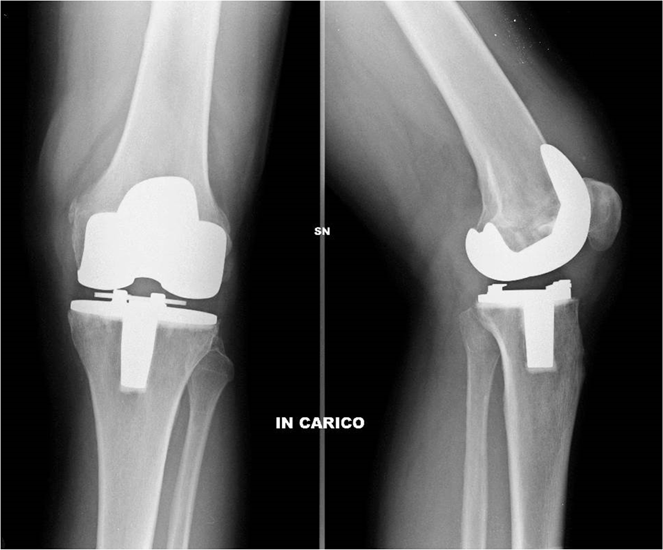
During surgery, the primary total knee arthroplasty was in place; exposure of the joint immediately revealed extensive discoloration infiltrating all the periprosthetic tissue and an important edema of the joint. There were no signs of infection or osteolysis; slight ossification in the ligamentous part medially. The primary TKA was removed and replaced with a semi constrained cemented TiNbN coated total knee prosthesis (GKS Butterfly, Permedica), so a completely an allergic implant (Figure 2).

Figure 2: Revision total knee arthroplasty with a cemented
semi-constrained TiNbN-coated total knee prosthesis.
Postoperatively, the patient recovered well with minimal pain in the operated knee. At the 3 months control, the patient was satisfied; clinically, the knee without swelling; normal skin color. ROM was still slightly reduced to flexion/extension 110°-0°.
Discussion
The literature regarding reactions following hip arthroplasty shows conflicting research, and the extent to which metal sensitivity affects implant lifespan and longevity remains debated, without clear evidence-based guidelines. Histopathological examination of periprosthetic tissue supports the correlation between wear particles leading to metal allergy and subsequent implant failure [2]. A prospective examination in patients following total knee arthroplasty (TKA) showed metal allergy by patch test was often seen in those with aseptic loosening (59%) versus stable prosthesis (48%) versus controls without prior orthopedic device implantation (20%) [3].
Individuals reporting a prior history of metal reactions before device implantation were four times more likely to develop implant failure [3]. A lymphocyte stimulation test before implantation of a chromium-containing device in those positive for chromium increased the risk of post-implant eczema. Metal hypersensitivity reactions following TKA are rare-the exact prevalence of MHR is unknown but estimates ranges from 0 to 5% of implanted devices [4]. A cohort study of 127 patients with 161 TKA compared to 161 control knee arthroplasty revealed that those with patch test positives to metal had similar complication, reoperation or revision rates when compared to those without allergy/matched controls.
Rates of post-operative pain were similar in those with metal allergy determined by patch testing, compared to control patients [5]. Given that there is no clear conclusion on the link between metal allergy and implant failure, it logically follows that there is a similar lack of consensus on the approach to the testing and management of patients. The crucial question at hand is whether there is a need to carry out screening prior to implanting metal devices.
Conclusion
To date there is no standard of care for the diagnosis of deep-tissue metal hypersensitivity associated with the presence of metallic orthopaedics implants. There is no agreement regarding the morbidity of metal allergy from implanted devices. In the clinical practice, we need to understand the risk of using devices which could provocate allergic reactions; being conscient that on the market do exist implant devices out of completely an allergic materials. As the clear relationship is not yet defined, we should take in consideration the possibility of an allergic reaction in our patients, suffering from pain, restricted ROM after primary TKA with a conventional metallic implant.
Patch testing is probably the best pre- and post-implant screening test, even if the postoperative one can vary in the diagnosis. Postoperatively, further criteria of metal hypersensitivity reactions include, together with a positive Patch test to the used metal, a skin reaction over the implant until a chronic dermatitis, starting often months after the primary implant [6,7]. For patients who experience residual pain after TKA, metal hypersensitivity should be suspected if the patient had a normal physical exam, normal X-ray and/or CT scan, and a normal laboratory exam.
References
- Lachiewicz PF., et al. “Metal Hypersensitivity and Total Knee Arthroplasty”. Journal of the American Academy of Orthopaedic Surgeons 24.2 (2016):106-112.
- Thakur RR., et al. “Severe persistent synovitis after cobalt-chromium total knee arthroplasty requiring revision”. Orthopedics 36.4 (2013): e520-524.
- Granchi D., et al. “Sensitivity to implant materials in patients with total knee arthroplasties”. Biomaterials 29.10 (2008):1494-1500.
- Guenther D., et al. “Allergic reactions in arthroplasty: myth or serious problem?” International Orthopaedics 40.2 (2016): 239-244.
- Bravo D., et al. “No Increased Risk of Knee Arthroplasty Failure in Patients With Positive Skin Patch Testing for Metal Hypersensitivity: A Matched Cohort Study”. Journal of Arthroplasty 31.8 (2016): 1717-1721.
- Frigerio E., et al. “Metal sensitivity in patients with orthopaedic implants: a prospective study”. Contact Dermatitis 64.5 (2011): 273-279.
- Mitchelson AJ., et al. “Biomaterial hypersensitivity: is it real? Supportive evidence and approach considerations for metal allergic patients following total knee arthroplasty”. BioMed Research International 2015 (2015): 137287.
Citation:
Villa Tiziano MD., et al. “Metal-Hypersensitivity (MHR) in Total Knee Arthroplasty: A Case Report”. Orthopaedic Surgery and
Traumatology 2.3 (2018): 343-346.
Copyright: © 2018 Villa Tiziano MD., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.