Clinical Case Report
Volume 1 Issue 1 - 2017
Iatrogenic Left Ventricular Dysfunction after Exogenous Administration of Intravenous Adrenaline
Department of Cardiology, Inmaculada Concepcion Hospital, Spain
*Corresponding Author: Antonio L Arrebola Moreno, Department of Cardiology, Inmaculada Concepcion Hospital, Spain.
Received: December 12, 2016; Published: January 09, 2017
Abstract
We present the clinic case of a healthy 19 year-old women that suffered an anaphylactic reaction after the sting of a vermin. She was administered intravenous adrenaline and developed acute left ventricular dysfunction.
Keywords: Adrenergic myocardiopathy; Adrenaline; Ventricular dysfunction
Manuscript
We present the clinical case of a healthy 19 year-old woman without any relevant past clinical history that suffered the sting of a vermin (probably a wasp) while riding a bicycle. Afterwards she presented an allergic reaction with skin rash and dyspnea. She went to the nearest emergency center and was administered a single dose of subcutaneous adrenaline relieving her symptoms. A few minutes later she started a new dyspnea episode and was administered an intravenous 80mg of methylprednisolone and 250 mg of adrenaline. After the last dose, she started an intense palpitation and sensation an oppressive non-irradiated chest pain with vegetative symptoms, vomiting and sweating. She was performed and EKG (Figure 1A) were sinus tachycardia, mild ST elevation and inverted T waves in the inferior- lateral territory, mild descended ST segment in V3 and V4, and marked (1.5 mm) elevation of ST segment in I and aVL were found. 20-30 minutes later the chest pain and EKG changes disappeared (Figure 1B). The peak levels of troponin-I were 2.75. The following days she was performed an echocardiogram (Figures 2A and 2B) were a mild dilated left ventricle (54 mm) was found together with global hipokinesia and moderately decreased ejection fraction (37%). The patient remained asymptomatic in the Cardiology ward and started treatment on Bisoprolol 2.5 mg. One week later a control echocardiogram revealed an ejection fraction of 50% and she was discharged asymptomatic. Finally, another echocardiogram was performed 6 months later showing an ejection fraction of 65% and bisoprolol was removed.
Several clinical cases have been reported regarding transient apical dyskinesia (Tako-Tsubo syndrome) after the administration of intravenous catecholamine [1,2]. Moreover, some catecholaminergic myocardiopathy cases have been reported [3,4] in patients presenting pheochromocytoma. However, no global left ventricular dysfunction (without segment wall motion abnormalities) in a complete healthy heart has been reported in this context. This case support the theory of myocardial contusion as a cause of ventricular dysfunction in patients suffering pheochromocytoma, thus, the catecholamine excess would lead to calcium overload mediated by cyclic adenosine- triphosphate that would decrease the myocyte´s synthetic activity and viability [5]. Although other pathophysiological pathways cannot be ruled out, like the production of diffuse vasospasm [6]. In the majority of these cases the ventricular dysfunction have good response to beta blockers, as well as in our patient [7]
To sum up, the novelty of this clinical case is that no other global ventricular dysfunction has been reported after the administration of intravenous catecholamines in a complete healthy heart, and helps to understand the pathophysiology of other illnneses (Tako-Tsubo Syndrome, Ventricular dysfunction in pheochromocytoma…) as well as to determine the usefulness of beta blockers in such a cases, and the possible adverse effects of exogenous adrenaline in patients with previous myocardiopathy.
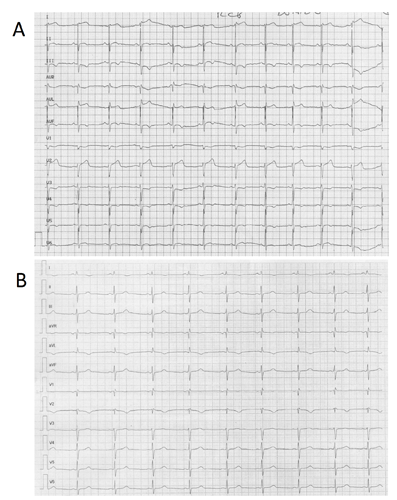
Figure 1A: Electrocardiograma tras la administración de adrenalina intravenosa.
Figure 1B: Electrocardiograma de control.
Figure 1B: Electrocardiograma de control.
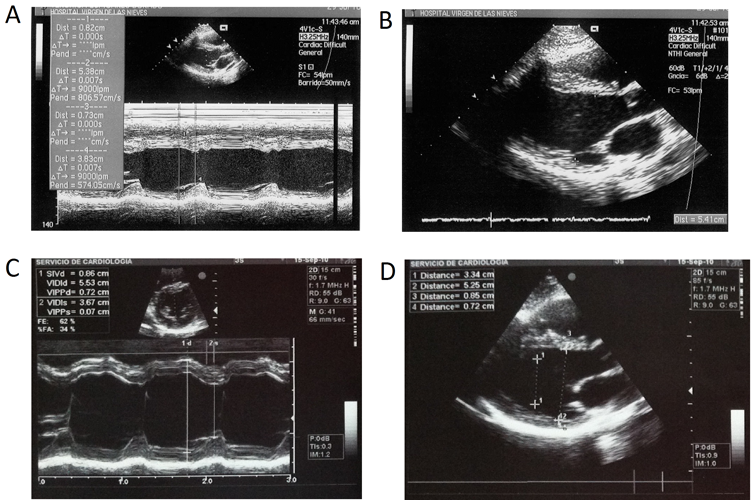
Figure 2: Ecocardiograma al ingreso en 2 dimensiones (A) y modo M (B). Ecocardiograma de control a los 6 meses en 2 dimensiones (A) y modo M (B)
References
- Laínez B., et al. “Iatrogenic tako-tsubo cardiomyopathy secondary to catecholamine administration”. Revista Espanola de Cardiologia 62.12 (2009): 1498-9.
- Litvinov IV., et al. “Iatrogenic epinephrine-induced reverse Takotsubo cardiomyopathy: direct evidence supporting the role of catecholamines in the pathophysiology of the "broken heart syndrome”. Clinical Research in Cardiology 98.7 (2009): 457-62.
- Di Palma G., et al. “Cardiogenic shock with basal transient left ventricular ballooning (Takotsubo-like cardiomyopathy) as first presentation of pheochromocytoma”. Journal of Cardiovascular Medicine (Hagerstown) 11.7 (2010): 507-10.
- Ter Bekke RM., et al. “Pheochromocytoma-induced ventricular tachycardia and reversible cardiomyopathy”. International Journal of Cardiology 147.1 (2009): 145-6.
- Mann DL., et al. “Adrenergic effects on the biology of the adult mammalian cardiocyte”. Circulation 85.2 (1992): 790–804.
- Galetta F., et al. “Cardiovascular complications in patients with pheochromocytoma: a mini-review”. Biomedicine & Pharmacotherapy 64.7 (2010): 505-9.
- Sutherland JA., et al. “Catecholamine-induced cardiomyopathy rapidly reversed with beta-blocker therapy”. Congestive Heart Failure 15.4 (2009): 193-5.
Citation:
Antonio L Arrebola Moreno. “Iatrogenic Left Ventricular Dysfunction after Exogenous Administration of Intravenous Adrenaline”. Therapeutic Advances in Cardiology 1.1 (2017): 12-14.
Copyright: © 2017 Antonio L Arrebola Moreno. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.