Research Article
Volume 1 Issue 1 - 2017
Implementation and Impact of Asthma Programme at Emergency Department.
1Nursing, Tan Tock Seng Hospital, Singapore
2Research Analyst Information Management Regional Health, National Healthcare Group, Singapore
3Respiratory Critical Care Medicine, Tan Tock Seng Hospital, Singapore
2Research Analyst Information Management Regional Health, National Healthcare Group, Singapore
3Respiratory Critical Care Medicine, Tan Tock Seng Hospital, Singapore
*Corresponding Author: Neo Lay Ping, BHSC (Nurs), RN, Registered Nurse, Tan Tock Seng Hospital, Singapore.
Received: September 12, 2017; Published: September 22, 2017
Abstract
Objective: The objective of this study was to evaluate the impact of an asthma programme (AP) on subsequent healthcare utilization and care practices in the Emergency Department.
Method: A retrospective pre-post study of AP group and a comparator group using a matched-group design. The AP group was composed of patients who had received education at ED; the comparator group was composed of patients who had attended ED before the implementation of the AP. The intervention consisted of education of asthma prevention, optimization of asthma treatment, and coordination of follow-up care after discharge.
Results: In total, 265 patients were selected for the AP group and 797 patients for the comparator group. The results showed that the implementation of an AP reduced ED utilization by 3.9% at 30 days and by 5.8% in 6 months. Average hospitalization rate was reduced by 1.3% and 2.2% at 30 days and 6 months respectively. The use of PEF readings increased by 77.7% as part of treatment planning, while the use of ACT scores increased by 93.6%. Of the patients in the AP group, 92.8% received follow-up appointments after their ED discharge. Compared to the comparator group, those with asthma durations of more than 5 years in the AP groupreported a significantly lower ED re-attendance rate at 6 months.
Conclusion: The AP successfully averted an undue increase in hospitalization rates and healthcare utilization at the ED. There was overall improvement in care practices by ED Physicians and coordination of follow-up post-discharge.
Keywords: Asthma; Emergency department; Nurse; Patient education
Abbreviations: ED: Emergency department; AP: Asthma Programme; TTSH: Tan Tock Seng Hospital; COPD: Chronic obstructive pulmonary disease; ESRD: End stage renal disease; SNAP: Singapore National; Asthma Programme; CPG: Clinical Practice Guidelines; CPRS: Cluster Patient Record System; CDMS: Chronic Disease Management System; NHG: National Healthcare Group; ACT: Asthma control test; PEF: Peak expiratory flow; PCP: primary care provider; GEE: Generalized Estimating Equation; SPSS: Statistical Packages for Social Sciences; ICS: Inhaled corticosteroids
Introduction
Asthma is a chronic inflammatory airway disease that affects more than 300 million people worldwide. [1] In Singapore, asthma affects about 5% of the adult population. [2] Patients with asthma are often admitted at the emergency department (ED) for acute exacerbation and the true burden of asthma in Singapore is unknown. In the public hospitals in Singapore, the number of ED visits due to asthma has increased at an annual rate of 5-10% since 2010. [3] This increase has largely been attributed to poor control of asthma due to inadequate long-term disease control, patient education, physiological changes, and social economic factors. [4-7] Furthermore, reports reveal that prior to ED attendance, most patients do not consult their primary care service for asthma care [8] despite the continual emphasis that the ultimate goal of GINA guideline should be to achieve and maintain asthma control for a prolonged period of time at primary care settings. [9]
Underutilization of primary care services lead to patient dependence on the ED as a site for episodic, crisis-oriented asthma care. [3] According to Lim and Chay, such suboptimal follow-ups with primary care services is a factor for fatal and near-fatal asthma. [10] The suboptimal follow-ups are also the reason the quality of asthma care and control in Singapore to be still below the global average. Among other identified barriers to best medical care practices are disease diagnosis, drug costs, patient factors, and prescription behaviour on the part of medical professionals. [11]
A previous study from Tan Tock Seng Hospital (TTSH) had identified lack of patient education, poor linkages to primary care providers, inadequate treatment to optimize asthma control, and lack of objective assessment as gaps in management of asthma exacerbation at the Emergency Department. [12] Such treatment practices are common and related to low adherence to asthma Clinical Practice Guidelines (CPG). Despite numerous interventions implemented globally in various ED that aim to reduce the use of ED as crisis-oriented, asthma care still remains insufficient [13-17].
With support from ED physicians and hospital-based asthma nurses from the Singapore National Asthma Programme (SNAP), effective interventions were adapted and integrated in an institution in Singapore. Asthma nurses were assigned at the ED during office hours to implement the asthma programme (AP). The AP consisted of pre-discharge asthma education at the ED, with additional emphasis on the optimization of treatment protocol and coordination of follow-up appointments with primary care providers after ED discharge. In addition, patients with complex and multi-factorial problems that required integrated intervention with case-management and social service were also facilitated.
This follow-up study was conducted to evaluate the effectiveness of the intervention of AP in reducing ED re-attendance and hospital admissions at 6 months and 30 days and the impact of care practices of asthma at the ED.
Methods
Study design and setting
This was a retrospective pre-post study using a matched-group design. The intervention was delivered at the 1500 bedded restructured hospital, Tan Tock Seng Hospital (TTSH), which was - and remains - the second largest acute care public hospital in Singapore.
This was a retrospective pre-post study using a matched-group design. The intervention was delivered at the 1500 bedded restructured hospital, Tan Tock Seng Hospital (TTSH), which was - and remains - the second largest acute care public hospital in Singapore.
Data sources and subjects recruitment
The Cluster Patient Record System (CPRS) launched by TTSH in 2008 and the Chronic Disease Management System (CDMS) launched by the National Healthcare Group (NHG) in 2007 were used to identify eligible patients for this study. The inclusion criteria were: (1) Singapore residents aged 16 years and above, and (2) those with principal diagnosis of asthma (ICD 9 codes 49390 and 49390A01) at the index ED visit to TTSH, where index visit for the intervention group (AP group) was between January 2012 and December 2013, while that of the historical comparator group was between January 2008 and July 2010 (before the implementation of the AP). The first attendance at the ED during the respective study periods was indicated as the index visit.
The Cluster Patient Record System (CPRS) launched by TTSH in 2008 and the Chronic Disease Management System (CDMS) launched by the National Healthcare Group (NHG) in 2007 were used to identify eligible patients for this study. The inclusion criteria were: (1) Singapore residents aged 16 years and above, and (2) those with principal diagnosis of asthma (ICD 9 codes 49390 and 49390A01) at the index ED visit to TTSH, where index visit for the intervention group (AP group) was between January 2012 and December 2013, while that of the historical comparator group was between January 2008 and July 2010 (before the implementation of the AP). The first attendance at the ED during the respective study periods was indicated as the index visit.
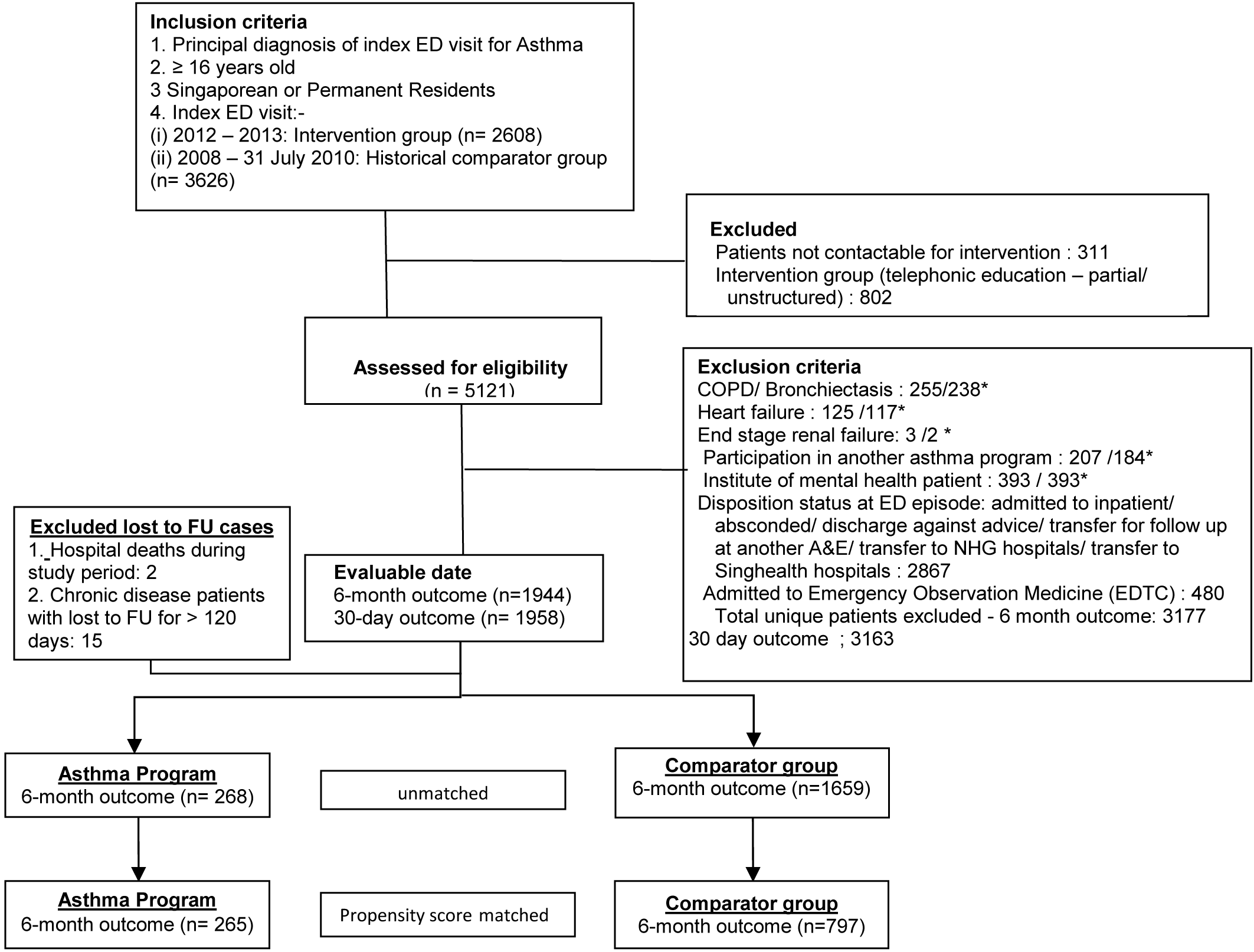
The exclusion criteria included patients with the following: (1) past medical history of Chronic obstructive pulmonary disease (COPD), bronchiectasis, heart failure, or end stage renal disease (ESRD); (2) previous visits to Institute of Mental Health; (3) concurrent participation in other asthma intervention programmes; (4) admission to hospital or short-stay-unit ward at index visit; and (5) index ED visit with disposition status of abscondment, discharged against medical advice or transferred to other hospital for further treatment (Figure 1).
Data on demographic profiles, past medical history, ED disposition status, healthcare visits, direct medical costs, ED re-attendance and hospitalization were retrieved for each patient from the CPRS and the CDMS.
The Asthma Programme at the Emergency Department
Certified asthma nurses were engaged to institute the AP during office hours. The AP comprised of three components which were drafted with references to GINA guidelines.
Certified asthma nurses were engaged to institute the AP during office hours. The AP comprised of three components which were drafted with references to GINA guidelines.
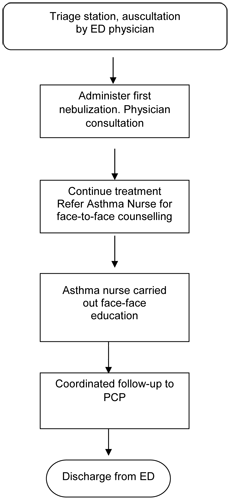
First component -Face-to-Face Asthma Education
The ED physicians referred patients to the asthma nurse to provide education on asthma (Figure 2). The face-to-face education on asthma was carried out through the use of a proforma. The nurse obtained the patients’ asthma history, frequency of healthcare utilisations, past near-fatal asthma episodes, triggers and adherence to medication. The asthma nurse also assessed patients’ inhaler techniques and identified possible barriers to their treatment. The asthma education programme involved discussion on the basic mechanisms of asthma, including common triggers and an explanation of the changes which occur to the airways resulting in the symptoms experienced by the patient. Lifestyle influences, such as occupation were discussed where appropriate with the individual. The need for `preventer' and `reliever' medication was also emphasized during this session.
The ED physicians referred patients to the asthma nurse to provide education on asthma (Figure 2). The face-to-face education on asthma was carried out through the use of a proforma. The nurse obtained the patients’ asthma history, frequency of healthcare utilisations, past near-fatal asthma episodes, triggers and adherence to medication. The asthma nurse also assessed patients’ inhaler techniques and identified possible barriers to their treatment. The asthma education programme involved discussion on the basic mechanisms of asthma, including common triggers and an explanation of the changes which occur to the airways resulting in the symptoms experienced by the patient. Lifestyle influences, such as occupation were discussed where appropriate with the individual. The need for `preventer' and `reliever' medication was also emphasized during this session.
The asthma nurse advocated proper prescription of preventers and recommended step-ups to their medications. Patients were provided post-emergency discharge plans and asthma first-aid advice to assist them in managing subsequent episodes of asthma attack. These sessions lasted on average 30 minutes.
Second component–Optimization of treatment protocol of asthma care at ED
Along with clinical assessments, peak expiratory flow (PEF) readings were monitored to assess the severity of the exacerbation and determine treatment responses. The asthma control test (ACT) score was used to assess the asthma control for 4 weeks preceding ED visit.
Along with clinical assessments, peak expiratory flow (PEF) readings were monitored to assess the severity of the exacerbation and determine treatment responses. The asthma control test (ACT) score was used to assess the asthma control for 4 weeks preceding ED visit.
The asthma nurse then discussed the patients’ asthma condition with the ED physicians and recommended the appropriate inhaler based on the stepwise approach to asthma management, following which, physicians carried out interventions closely guided by the evidence-based clinical protocol.
Third component–Coordination of follow-up care after ED discharge
The asthma nurse ensured that patients discharged from the ED were linked to follow-up care providers. Follow-up appointments, either to a specialist asthma clinic or a primary care provider (PCP), were arranged for patients according to the acuity of exacerbation and level of asthma control. Although patients’ preference of follow-up care was taken into consideration during discharge planning, the asthma nurse would advocate appropriate follow-up care as closely guided by the treatment protocol. Patients were scheduled with follow-up appointments to either a specialist asthma clinic in public hospitals, public primary care outpatient clinic or private general practitioners (GP) within 14 days of being discharged from ED. Patients were routinely monitored for re-attendance to ED and hospital admission for asthma at 30 days and then at 6 months.
The asthma nurse ensured that patients discharged from the ED were linked to follow-up care providers. Follow-up appointments, either to a specialist asthma clinic or a primary care provider (PCP), were arranged for patients according to the acuity of exacerbation and level of asthma control. Although patients’ preference of follow-up care was taken into consideration during discharge planning, the asthma nurse would advocate appropriate follow-up care as closely guided by the treatment protocol. Patients were scheduled with follow-up appointments to either a specialist asthma clinic in public hospitals, public primary care outpatient clinic or private general practitioners (GP) within 14 days of being discharged from ED. Patients were routinely monitored for re-attendance to ED and hospital admission for asthma at 30 days and then at 6 months.
Assessment of outcome
In this study, the 6-month ED re-attendance was used as the primary outcome. The ED re-attendance was defined as an unscheduled visit for an asthma exacerbation after discharge from the index ED visits. Hospital admission was defined as a hospitalization with asthma exacerbation after discharge from the index ED visits. The 30-day and 6-month ED re-attendance and hospital admission were monitored from the first index visit to the ED. To enhance outcome measurements, this study also tracked patients’ ED re-attendance and hospitalization beyond TTSH at both National University Hospital and Alexandra Hospital.
In this study, the 6-month ED re-attendance was used as the primary outcome. The ED re-attendance was defined as an unscheduled visit for an asthma exacerbation after discharge from the index ED visits. Hospital admission was defined as a hospitalization with asthma exacerbation after discharge from the index ED visits. The 30-day and 6-month ED re-attendance and hospital admission were monitored from the first index visit to the ED. To enhance outcome measurements, this study also tracked patients’ ED re-attendance and hospitalization beyond TTSH at both National University Hospital and Alexandra Hospital.
Data Management
Approval
An approval to conduct this study was obtained from the NHG Ethics Review Board.
Approval
An approval to conduct this study was obtained from the NHG Ethics Review Board.
Sample size computation
The minimum sample size computed for this study used the 6-month ED re-attendance as the primary outcome based on an inter-group patient ratio of 4:1 (comparator group: AP group). Based on the 0.4 standard deviation in outcome and 0.28 correlation in repeated measurements, an estimated sample size of 1415 patients in the AP group and 5660 patients in the comparator group were required to detect a 10% difference in the between-group outcome at 5% type 1 error and 80% power.
The minimum sample size computed for this study used the 6-month ED re-attendance as the primary outcome based on an inter-group patient ratio of 4:1 (comparator group: AP group). Based on the 0.4 standard deviation in outcome and 0.28 correlation in repeated measurements, an estimated sample size of 1415 patients in the AP group and 5660 patients in the comparator group were required to detect a 10% difference in the between-group outcome at 5% type 1 error and 80% power.
Propensity score matching
Propensity score matching was used for the selection of subjects in this study to minimize bias induced by the observable differences in characteristics between the intervention and comparator groups. The propensity score was derived from the multivariate logistic regression using 24 pre-intervention characteristics including demographic profiles, past medical history, patient acuity category at the index visit and healthcare utilization within 6 months and 30 days before the index visit, as well as interaction terms. The nearest neighbor matching within a caliper width of 0.2 of the pooled standard deviation of the propensity score was employed using variable ratio matching (N: 1), where N allowed selection of up to 4 patients in the comparator group to 1 in the intervention group. [18] Performance of the matching was assessed using an absolute standardized mean difference of <0.10 that denoted negligible imbalance between the 2 groups. [19] After the propensity score matching, the remaining residual differences in the observed baseline covariates between the AP and comparator groups were adjusted in the regression model to increase the precision of the outcomes. [20]
Propensity score matching was used for the selection of subjects in this study to minimize bias induced by the observable differences in characteristics between the intervention and comparator groups. The propensity score was derived from the multivariate logistic regression using 24 pre-intervention characteristics including demographic profiles, past medical history, patient acuity category at the index visit and healthcare utilization within 6 months and 30 days before the index visit, as well as interaction terms. The nearest neighbor matching within a caliper width of 0.2 of the pooled standard deviation of the propensity score was employed using variable ratio matching (N: 1), where N allowed selection of up to 4 patients in the comparator group to 1 in the intervention group. [18] Performance of the matching was assessed using an absolute standardized mean difference of <0.10 that denoted negligible imbalance between the 2 groups. [19] After the propensity score matching, the remaining residual differences in the observed baseline covariates between the AP and comparator groups were adjusted in the regression model to increase the precision of the outcomes. [20]
Statistical analysis
A binomial distribution with a logit link function in the Generalized Estimating Equation (GEE) was used to evaluate percent reduction in the number of patients who developed outcomes. A negative binomial distribution with a log link function in the GEE was used to evaluate the reduction in the average number of ED re-attendances and hospitalizations per patient. The “Difference-in-Difference” approach quantified the intervention effect using estimated marginal means. The intervention was considered effective if the interaction effect of the group assignment by time point (baseline- and ending-time points) had probability p < 0.05.
A binomial distribution with a logit link function in the Generalized Estimating Equation (GEE) was used to evaluate percent reduction in the number of patients who developed outcomes. A negative binomial distribution with a log link function in the GEE was used to evaluate the reduction in the average number of ED re-attendances and hospitalizations per patient. The “Difference-in-Difference” approach quantified the intervention effect using estimated marginal means. The intervention was considered effective if the interaction effect of the group assignment by time point (baseline- and ending-time points) had probability p < 0.05.
Statistical analysis was performed using the Statistical Packages for Social Sciences (SPSS) v21.0. For PS matching, the Match IT programme in R v3.1.3 was used.
Results
Patient Characteristics
During the study period,a total of 2608 and 3626 patients were recruited to the AP and comparator groups respectively. With exclusion of predetermined criteria, 268 and 1659 patients were selected from the AP and comparator groups respectively for propensity score matching (Figure 1). We analysed 265 patients in the AP group and 797 in the comparator group.
During the study period,a total of 2608 and 3626 patients were recruited to the AP and comparator groups respectively. With exclusion of predetermined criteria, 268 and 1659 patients were selected from the AP and comparator groups respectively for propensity score matching (Figure 1). We analysed 265 patients in the AP group and 797 in the comparator group.
Both groups of patients were matched according to the 24 covariates. The baseline characteristics of the study population are shown in Table 1.
| After 1-to-N matching | ||
| Covariates | Asthma Programme (n = 265) % |
Comparator (n = 797) % |
| Socio-Demographics
Age (years) * Gender (Female) Ethnic group - Chinese - Indian - Malay |
39.5 ± 16.7 56.6 38.9 20.8 27.2 |
36.9 ± 16.4 53.7 41.0 20.5 27.5 |
| Region in Singapore - Central - East - North - North east - West |
38.5 8.7 9.4 38.5 4.9 |
37.3 9.3 11.4 36.6 5.4 |
| National Service (Yes) | 8.3 | 9.7 |
| Medical history Asthma duration (years) Chronic Kidney Disease (Yes) Coronary heart disease (Yes) Diabetes (Yes) Hypertension (Yes) Stroke (Yes) Obesity (BMI > 27.5) (Yes) |
3.7 ± 5.4 5.7 3.4 9.4 15.1 1.5 39.2 |
2.6 ± 4.5 3.9 2.8 8.2 12.0 1.4 22.6 |
| Conditions at index ED visit
PAC Status at index ED visit P1 P2 P3 |
57.4 30.2 12.5 |
57.1 30.2 12.5 |
| Healthcare Utilisation (Number) | ||
| *ED visits within 30D before index visit | 0.03 ± 0.17 | 0.02 ± 0.19 |
| *ED visits within 6M before index visit | 0.12 ± 0.43 | 0.09 ± 0.57 |
| Admission within 30D before index visit | 0.01 ± 0.11 | 0.01 ± 0.09 |
| Admission within 6M before index visit | 0.05 ± 0.24 | 0.03 ± 0.28 |
| **SOC visits within 30D before index visit | 0.09 ± 0.31 | 0.10 ± 0.38 |
| **SOC visits within 6M before index visit | 0.63 ± 1.48 | 0.58 ± 1.34 |
| ***NHGP visits within 30D before index visit | 0.11 ± 0.38 | 0.08 ± 0.34 |
| ***NHGP visits within 6M before index visit | 0.26 ± 0.73 | 0.23 ± 0.78 |
*Emergency Department
**Specialist Outpatient Clinic
***National Healthcare Group Polyclinic
Table 1: Characteristics of patients after matching.
**Specialist Outpatient Clinic
***National Healthcare Group Polyclinic
Table 1: Characteristics of patients after matching.
ED re-attendance
Table 2a illustrated the adjusted differences in outcomes at 6 months and 30 days. At 6 months, the AP group showed a 3.8% increase in ED re-attendance, compared to 9.5% in the comparator group. This reflected a difference-in-difference of 5.8% reduction, suggesting that 5.8% of the potential increase in ED re-attendance at 6 months could be averted if patients in the AP group followed the same trend as patients in the comparator group. Correspondingly, there was also a difference-in-difference of 0.107 reduction in the average number of ED re-attendances per patient at 6 months after the intervention (Table 2b). This translated to a reduction of 29 ED re-attendances in the AP group. Similarly, there was a difference-in-difference of 3.9% reduction in the 30-day ED re-attendance, and 0.049 reduction in the average number of 30-day ED re-attendances per patient (Table 2a and 2b).
Table 2a illustrated the adjusted differences in outcomes at 6 months and 30 days. At 6 months, the AP group showed a 3.8% increase in ED re-attendance, compared to 9.5% in the comparator group. This reflected a difference-in-difference of 5.8% reduction, suggesting that 5.8% of the potential increase in ED re-attendance at 6 months could be averted if patients in the AP group followed the same trend as patients in the comparator group. Correspondingly, there was also a difference-in-difference of 0.107 reduction in the average number of ED re-attendances per patient at 6 months after the intervention (Table 2b). This translated to a reduction of 29 ED re-attendances in the AP group. Similarly, there was a difference-in-difference of 3.9% reduction in the 30-day ED re-attendance, and 0.049 reduction in the average number of 30-day ED re-attendances per patient (Table 2a and 2b).
| Outcomes | Asthma Programme (n=265) |
Comparator (n= 797) |
Difference-in-difference (AP – Comparator) |
||||
| Baseline (%) | Follow- up (%) | Difference (%) |
Baseline (%) | Follow- up (%) | Difference (%) | ||
| ED visit 6M | 14.5 | 18.3 | + 3.8 | 9.6 | 19.1 | + 9.5 | - 5.8 |
| ED visit 30D | 4.3 | 6.1 | + 1.8 | 2.6 | 8.3 | + 5.7 | - 3.9 |
| Admission 6M | 6.7 | 6.0 | - 0.7 | 5.0 | 6.6 | + 1.6 | - 2.2 |
| Admission 30D | 1.4 | 2.3 | + 0.9 | 1.5 | 3.7 | + 2.2 | - 1.3 |
Using Generalised Estimating Equation model with the logit link function, binomial distribution, and adjusted for
Group, time, group x time and propensity score, with covariates fixed at the mean of the propensity score
Table 2a: Adjusted differences in outcomes (estimated marginal means) at 6 months and 30 days.
Table 2a: Adjusted differences in outcomes (estimated marginal means) at 6 months and 30 days.
| Outcomes | Asthma Programme (n=265) |
Comparator (n= 797) |
Difference-in-difference (AP – Comparator) |
||||
| Baseline(mean) | Follow-up (mean) | Difference (mean) |
Baseline (mean) | Follow- up (mean) | Difference (mean) |
||
| ED visit 6M | 0.196 | 0.292 | 0.096 | 0.167 | 0.370 | 0.203 | -0.11 |
| ED visit 30D | 0.041 | 0.062 | 0.021 | 0.039 | 0.109 | 0.07 | -0.049 |
| Admission 6M | 0.072 | 0.071 | -0.001 | 0.069 | 0.085 | 0.016 | -0.017 |
| Admission 30D | 0.015 | 0.023 | 0.008 | 0.015 | 0.040 | 0.025 | -0.015 |
Using Generalised Estimating Equation model with the log link function, negative binomial distribution, and adjusted
for Group, time, group x time and propensity score, with covariates fixed at the mean of the propensity score
Table 2b:
Table 2b:
In comparison with the comparator group, the odds of having an ED re-attendance within 6 months and 30 days in the AP group were smaller at 0.590 (95% CI: 0.316–1.101) and 0.429 (95% CI: 0.144-1.275) respectively (Table 4). Nevertheless, the intervention effects of the AP, as indicated by the interaction of group assignment and time point, were statistically insignificant despite having lower healthcare utilization.
Hospital admissions
There was a difference-in-difference of 2.2% and 1.3% reductions in hospitalizations at 6 months and 30 days respectively (Table 2a), corresponding to difference-in difference of 0.017 and 0.015 reductions in the average number of hospitalizations per patient within 6 months and 30 days respectively (Table 2b). These represented that potential increases of 5 and 4 hospitalization’s at 6 months and 30 days respectively could be averted if patients in the AP group followed the same trend as patients in the comparator group.
There was a difference-in-difference of 2.2% and 1.3% reductions in hospitalizations at 6 months and 30 days respectively (Table 2a), corresponding to difference-in difference of 0.017 and 0.015 reductions in the average number of hospitalizations per patient within 6 months and 30 days respectively (Table 2b). These represented that potential increases of 5 and 4 hospitalization’s at 6 months and 30 days respectively could be averted if patients in the AP group followed the same trend as patients in the comparator group.
In comparison with the comparator group, the odds of 6 months and 30 days hospitalization’s in the AP group were smaller at 0.668 (95% CI: 0.272–1.643) and 0.650 (95% CI: 0.118-3.570) respectively. Despite these results, intervention effects of the AP were statistically insignificant compared with the comparator group (Table 3).
| Outcome (%) | Adj. OR | 95% CI | P value |
| ED visits within 6M | |||
| Group | 1.608 | 0.947 – 2,731 | 0.079 |
| Time | 2.229 | 1.650 – 3.010 | < 0.001 |
| Propensity score* | 2.298 | 1.004 – 5.259 | 0.049 |
| Group x Time | 0.590 | 0.316 – 1.101 | 0.097 |
| ED visits within 30D | |||
| Group | 1.672 | 0.657 – 4.258 | 0.281 |
| Time | 3.379 | 2.023 – 5.642 | < 0.001 |
| Propensity score* | 1.361 | 0.374 – 4.955 | 0.640 |
| Group x Time | 0.429 | 0.144 – 1.275 | 0.128 |
| Hospital admission within 6M | |||
| Group | 1.370 | 0.680 – 2.762 | 0.378 |
| Time | 1.333 | 0.893 - 1.990 | 0.160 |
| Propensity score* | 6.632 | 2.364 – 18.607 | <0.001 |
| Group x Time | 0.668 | 0.272 – 1.643 | 0.380 |
| Hospital admission within 30D | |||
| Group | 0.939 | 0.234 – 3.770 | 0.929 |
| Time | 2.525 | 1.297 – 4.918 | 0.006 |
| Propensity score* | 6.732 | 1.528 – 29.656 | 0.012 |
| Group x Time | 0.650 | 0.118 – 3.570 | 0.620 |
Using Generalised Estimating Equation model with the logit link function, binomial distribution.
*To adjust for remaining differences in the observed baseline covariates between the AP and comparator groups
Group: reference = comparator group
Table 3: Adjusted Odds Ratio of healthcare utilisation at 6 months and 30 days post ED discharge.
*To adjust for remaining differences in the observed baseline covariates between the AP and comparator groups
Group: reference = comparator group
Table 3: Adjusted Odds Ratio of healthcare utilisation at 6 months and 30 days post ED discharge.
Patients with more than 5 years of asthma benefited more from the intervention
This study showed that patients with asthma histories of over 5 years benefited more from the intervention. Patients in the AP group with asthma histories of >5 years had a significantly lower ED re-attendance at 6 months (OR: 0.250; 95% CI: 0.077–0.809; p = 0.021) compared to patients in the comparator group. For patients with asthma histories of less than 5 years, the reduction in the outcome was not statistically different from the comparator group (Table 4), despite having lower adjusted odds of ED re-attendance at 6 months.
This study showed that patients with asthma histories of over 5 years benefited more from the intervention. Patients in the AP group with asthma histories of >5 years had a significantly lower ED re-attendance at 6 months (OR: 0.250; 95% CI: 0.077–0.809; p = 0.021) compared to patients in the comparator group. For patients with asthma histories of less than 5 years, the reduction in the outcome was not statistically different from the comparator group (Table 4), despite having lower adjusted odds of ED re-attendance at 6 months.
| 6M ED re-attendance (%) Asthma Duration: | Adj. OR | 95% CI | P value |
| Up to 5 years | |||
| Group | 1.019 | 0.482–2.154 | 0.962 |
| Time | 2.347 | 1.720–3.201 | < 0.001 |
| Propensity score* | 1.774 | 0.476–6.607 | 0.393 |
| Group x Time | 0.598 | 0.217–1.648 | 0.320 |
| More than 5 years | |||
| Group | 6.975 | 2.376–19.432 | < 0.001 |
| Time | 8.316 | 3.195–21.645 | < 0.001 |
| Propensity score* | 1.800 | 0.397–8.160 | 0.446 |
| Group x Time | 0.250 | 0.077 – 0.809 | 0.021 |
*To adjust for remaining differences in the observed baseline covariates between the AP and comparator groups
Note: Analyses were carried out for the following numbers of AP and comparator group patients: >0 to 5 years (80 vs 298); >5 years (92 vs 172)
Group : reference = comparator group
Table 4: Adjusted Odds Ratio of 6-month ED re-attendance by duration of asthma.
Note: Analyses were carried out for the following numbers of AP and comparator group patients: >0 to 5 years (80 vs 298); >5 years (92 vs 172)
Group : reference = comparator group
Table 4: Adjusted Odds Ratio of 6-month ED re-attendance by duration of asthma.
Practices of care delivery
Table 5 compares the extent of delivery of the 6 interventions in the AP and the comparator groups at the index ED visit. Two components of the AP-related to discussions with physicians on patients’ asthma status and face-to-face education - were delivered to 100% of patients in AP group. 77.7% of the patients in the AP group had PEF measurements done, while none of the comparator group received PEF measurements. 93.6% of the patients in the AP group had their ACT scores assessed, compared to 29.9% in the comparator group. In terms of prescription of inhaled corticosteroids (ICS), 58.9% of patients in AP were prescribed ICS compared to 25.4% in the comparator group. Upon ED discharge, 92.8% of the AP group patients received coordinated follow-up care, while only 45.6% of comparator group received the same.
Table 5 compares the extent of delivery of the 6 interventions in the AP and the comparator groups at the index ED visit. Two components of the AP-related to discussions with physicians on patients’ asthma status and face-to-face education - were delivered to 100% of patients in AP group. 77.7% of the patients in the AP group had PEF measurements done, while none of the comparator group received PEF measurements. 93.6% of the patients in the AP group had their ACT scores assessed, compared to 29.9% in the comparator group. In terms of prescription of inhaled corticosteroids (ICS), 58.9% of patients in AP were prescribed ICS compared to 25.4% in the comparator group. Upon ED discharge, 92.8% of the AP group patients received coordinated follow-up care, while only 45.6% of comparator group received the same.
| Asthma Programme Content | Asthma programme (n = 265) |
Comparator (n=797) |
| 1. Discussion with ED physician on patient’s asthma control and treatment | 100.0% | 0% |
| 2. Assessment of patient’s Peak Flow rate | 77.7% | 0% |
| 3. Assessment of patient’s ACT score | 93.6% | 29.9% |
| 4. Face-to-face education and self-management | 100.0% | 0 % |
| 5. Prescription of ICS* upon discharge from ED | 58.9% | 25.4% |
| 6. Coordinated care on outpatient follow up for asthma control | 92.8% | 45.6% |
*Beclomethasone, Budesonide & Formoterol, Fluticasone & Salmeterol
Table 5: Extent of delivery of Asthma programme intervention at index ED visit.
Table 5: Extent of delivery of Asthma programme intervention at index ED visit.
Discussion
Healthcare utilization
This study demonstrated that implementing an AP led to the reduction of post-discharge ED re-attendance by 5.8% and 3.9% at 6 months and 30 days respectively, translating to potential reductions of 29 and 13 ED attendances at 6 months and 30 days respectively. Similarly, the reduction of 2.2% and 1.3% in patient hospitalization at 6 months and 30 days respectively also translated to potential reductions of 5 and 4 hospital admissions at 6 months and 30 days respectively. Although the financial cost of implementing the programme was not evaluated, it would be logical to extrapolate that a significant portion of direct medical costs could be reduced through this programme. This assumption is supported by the reports of similar education programs in other countries. [17,21]
This study demonstrated that implementing an AP led to the reduction of post-discharge ED re-attendance by 5.8% and 3.9% at 6 months and 30 days respectively, translating to potential reductions of 29 and 13 ED attendances at 6 months and 30 days respectively. Similarly, the reduction of 2.2% and 1.3% in patient hospitalization at 6 months and 30 days respectively also translated to potential reductions of 5 and 4 hospital admissions at 6 months and 30 days respectively. Although the financial cost of implementing the programme was not evaluated, it would be logical to extrapolate that a significant portion of direct medical costs could be reduced through this programme. This assumption is supported by the reports of similar education programs in other countries. [17,21]
Impact of asthma duration on ED re-attendance rate
Patients with asthma diagnosis of more than 5 years had lower ED re-attendance rates at 6 months compared to patients with a shorter duration of disease.
Patients with asthma diagnosis of more than 5 years had lower ED re-attendance rates at 6 months compared to patients with a shorter duration of disease.
This may be explained by the fact that patients with longer asthma histories had established care by the primary care team and/or the asthma specialist clinic. These patients were more likely to possess adequate asthma knowledge, exhibit competency on inhaler techniques and practice self-management skills to better cope with asthma symptoms.
Practice Care delivery at ED
Assessment of PEF Clinical practice guidelines recommended early PEF measurement during treatments of asthma exacerbation. [9, 22] Likewise, many studies recommended the use of PEF for assessing the severity of an exacerbation and the response to treatment. [4,16,23]
Assessment of PEF Clinical practice guidelines recommended early PEF measurement during treatments of asthma exacerbation. [9, 22] Likewise, many studies recommended the use of PEF for assessing the severity of an exacerbation and the response to treatment. [4,16,23]
On the other hand, others did not find the measurement of PEF useful during acute management of exacerbation of asthma at ED. [24,25] Despite the inconsistent evidence on the usefulness of PEF during asthma exacerbation, TTSH continued to follow the guidelines on using PEF measurement during asthma exacerbation at ED. [9]
78% of our study population had previously had a PEF performed, which suggests that PEF cannot be measured in all patients presenting asthma exacerbation. The inability to perform PEF for all patients present at the ED was likely due to patients experiencing breathlessness, refusing to perform peak-flow or exhibiting poor technique during peak-flow. Therefore, the decision to perform PEF should be made based on the individual’s severity of asthma when presenting to the ED. It should not be a blanket application for all.
Assessment of control using Asthma Control Test
The ACT score reflects the patient’s asthma control and can be used to monitor treatment progress. [26] Although ACT is freely available to all doctors, it is not routine practice to assess patients’ asthma control by using ACT scores at the ED. (12) In this study, only 29.9% in the comparator group had been assessed with the ACT. Following implementation of the AP, there was a substantial increase (93.6%) on the use of ACT for asthma patients at the ED. Assessment of the patient’s level of asthma control could help determine if the patient’s current asthma controller medications needed to be augmented.(27) Although the ACT score was predominantly used as a tool to assess asthma control during routine review, an understanding of the patient’s asthma control preceding ED visit also enabled appropriate optimisation of the controller prior to discharge. However, we did not further associate the level of asthma control with the usage of ICS.
The ACT score reflects the patient’s asthma control and can be used to monitor treatment progress. [26] Although ACT is freely available to all doctors, it is not routine practice to assess patients’ asthma control by using ACT scores at the ED. (12) In this study, only 29.9% in the comparator group had been assessed with the ACT. Following implementation of the AP, there was a substantial increase (93.6%) on the use of ACT for asthma patients at the ED. Assessment of the patient’s level of asthma control could help determine if the patient’s current asthma controller medications needed to be augmented.(27) Although the ACT score was predominantly used as a tool to assess asthma control during routine review, an understanding of the patient’s asthma control preceding ED visit also enabled appropriate optimisation of the controller prior to discharge. However, we did not further associate the level of asthma control with the usage of ICS.
The minority of patients with no ACT scores might have faced difficulties relating to the questionnaires used in the study. A previous study on ACT suggests that patients who are illiterate, poor historians and who are unable to comprehend the questionnaires may have difficulties completing it. [28]
The prescription of ICS upon discharge from ED
In this study, the prescription rate for ICS at discharge was higher in the AP group (58.9%) than in the comparator group (25.4%). One key feature of the AP was active case discussion between ED physicians and the asthma nurse on the patient’s asthma control and treatment adherence. This facilitated appropriate treatment adjustment and discharge planning. This suggests that implementation of the AP led to an increase in the awareness of asthma treatment guidelines among physicians, leading to better prevalence of the use of ICS. However, further improvement would still be needed to achieve increased prescription of ICS for all patients presenting to ED for acute asthma exacerbation.
In this study, the prescription rate for ICS at discharge was higher in the AP group (58.9%) than in the comparator group (25.4%). One key feature of the AP was active case discussion between ED physicians and the asthma nurse on the patient’s asthma control and treatment adherence. This facilitated appropriate treatment adjustment and discharge planning. This suggests that implementation of the AP led to an increase in the awareness of asthma treatment guidelines among physicians, leading to better prevalence of the use of ICS. However, further improvement would still be needed to achieve increased prescription of ICS for all patients presenting to ED for acute asthma exacerbation.
Studies have shown that the use of ICS on patients with asthma at the time of discharge from ED was associated with a lower relapse rate and improved health-related quality of life. [4,23,29]
Further, GINA guidelines recommended that patients with severe exacerbation should be prescribed regular on-going ICS treatment at ED discharge as ICS significantly reduced the risk of asthma-related death or hospitalization. [30,9] A recent study on asthma mortality in Singapore showed a reduction of mortality rates from 7 to 2 per million population. The authors postulated that the reduction in asthma death might be associated with the increase in the usage of ICS. [10,17] Thus, more effort would need to be taken to increase the prescription of ICS after an acute exacerbation of asthma. Patients who were discharged without ICS in this study might have presented with a mild exacerbation at discharge. That said, however, it should be noted that the association of the severity of asthma exacerbation with the prescription of ICS was not the immediate focus of this study.
Follow-up care after ED discharge
Another major component of the AP was the coordination of follow-up appointments by asthma nurses while the patient was being prepared for discharge from the ED. This enhancement of service aimed to bridge the gap between hospital care and primary care providers, as highlighted by the previous study. [12] Patients were tasked to continue with follow-ups by respiratory physicians in the hospital and/or the primary care team for the continuation of care. After an acute asthma exacerbation, an asthma nurse was on hand to present the range of available primary care options to the patients, and subsequently connect said patients to their preferred PCP with a scheduled appointment. Patients who chose to continue follow-up treatment at their private doctors’ clinics were advised to do so within 14 days of discharge. Patients who preferred subsidized primary care at the public polyclinicswere also given scheduled appointments. Thus, 92.8% of patients in the AP group were successfully connected to their PCPs.
Another major component of the AP was the coordination of follow-up appointments by asthma nurses while the patient was being prepared for discharge from the ED. This enhancement of service aimed to bridge the gap between hospital care and primary care providers, as highlighted by the previous study. [12] Patients were tasked to continue with follow-ups by respiratory physicians in the hospital and/or the primary care team for the continuation of care. After an acute asthma exacerbation, an asthma nurse was on hand to present the range of available primary care options to the patients, and subsequently connect said patients to their preferred PCP with a scheduled appointment. Patients who chose to continue follow-up treatment at their private doctors’ clinics were advised to do so within 14 days of discharge. Patients who preferred subsidized primary care at the public polyclinicswere also given scheduled appointments. Thus, 92.8% of patients in the AP group were successfully connected to their PCPs.
Limitations
This study was limited by its small sample size, which therefore limited the generalizability of its results to the general population. The low statistical power of this study reduced the chance of detecting a true intervention effect. Data was collected exclusively from National Healthcare Group (NHG) hospitals (Tan Tock Seng Hospital, National University Hospital, and Alexandra Hospital) and NHG primary care clinics. We were not able to obtain information on the patients’ subsequent follow-up status at other public or private hospitals and private GP practices.
This study was limited by its small sample size, which therefore limited the generalizability of its results to the general population. The low statistical power of this study reduced the chance of detecting a true intervention effect. Data was collected exclusively from National Healthcare Group (NHG) hospitals (Tan Tock Seng Hospital, National University Hospital, and Alexandra Hospital) and NHG primary care clinics. We were not able to obtain information on the patients’ subsequent follow-up status at other public or private hospitals and private GP practices.
Despite propensity score matching being performed for this study, the matching only balanced the distribution of measured baseline variables between the two groups; the balance may not be similarly achieved for unobserved variables that were not examined in this study. Three patients and 862 patients were excluded from the AP and comparator groups respectively for the analysis due to unsuccessful matching. Although the impact of this incomplete matching was minimal to the AP group, the exclusion of a large number of patients from the comparator group had more significant consequence in reducing the generalizability of the results. Lastly, misclassification bias due to the use of secondary database and selection bias arising from the exclusion of patients with missing data, was inevitable in this study due to the retrospective nature of the study design.
Conclusion
The implementation of an AP has improved the practice of care by ED physicians in areas such as prescribing ICS, enforcing objective measurements (ACT and PEF monitoring), and coordinating discharge planning and follow-up care for asthma patients seen at the ED. This study showed that the AP group had lower rates of ED re-attendance and hospital admissions at 6 months and 30 days. However, the intervention effects were not statistically significant, which could be due to the low statistical power of this study. A study with a larger sample size would be required to further quantify the benefits of the AP.
Acknowledgment
The authors wish to thank Professor Lim Tow Keang, Director of Singapore National Asthma Program and Madam Wong Wai Mun for their support; Ms Lee Lin Jen, National Healthcare Group, Singapore for support in data extraction; Ms Tham Lai Mei, Adjunct Associate Professor Tay Seow Yian, Head of Department, ED and all ED staffs for their support and corporation with the asthma nurse.
The authors wish to thank Professor Lim Tow Keang, Director of Singapore National Asthma Program and Madam Wong Wai Mun for their support; Ms Lee Lin Jen, National Healthcare Group, Singapore for support in data extraction; Ms Tham Lai Mei, Adjunct Associate Professor Tay Seow Yian, Head of Department, ED and all ED staffs for their support and corporation with the asthma nurse.
References
- Masoli M., et al. “The global burden of asthma: executive summary of the GINA Dissemination Committee Report”. Allergy (2004): 469-478.
- Chronic diseases. Health Hub. (2017).
- Lim S., et al. “Frequent attenders to the ED: patients who present with repeated asthma exacerbations”. American Journal of Emergency Medicine 32.8 (2014): 895-899.
- Hodder R., et al. “Management of acute asthma in adults in the emergency department: Nonventilatory management”. Canadian Medical Association Journal 182.2 (2010): E55-67.
- Robichaud P., et al. “Evaluation of a program aimed at increasing referrals for asthma education of patients consulting at the emergency department for acute asthma”. Chest 126.5 (2004): 1495-1501.
- Baren JM., et al. “Randomized controlled trial of emergency department interventions to improve primary care follow-up for patients with acute asthma”. Chest 129.2 (2006): 257-265.
- Boulet LP., et al. “Characteristics of subjects with a high frequency of emergency visits for asthma”. American Journal of Emergency Medicine 14.7 (1996): 623-628.
- Partridge MR., et al. “A national census of those attending UK accident and emergency departments with asthma. The UK National Asthma Task Force”. Journal of accident & emergency medicine 14.1 (1997): 16-20.
- Global Strategy for Asthma Management and for Asthma (2015).
- Lim TK and Chay OM. “Fatal asthma in Singapore”. Annals of the Academy of Medicine 41.5 (2012): 187-188.
- Tan NC., et al. “Factors influencing family physicians’ drug prescribing behaviour in asthma management in primary care”. Singapore Medical Journal 50.3 (2009): 312-319.
- Prabhakaran L., et al. “The current care delivery practice for asthma at the emergency department in a tertiary hospital in Singapore”. Journal of Asthma & Allergy Educators 4.1 (2013): 15-21.
- Tapp S., et al. “Education interventions for adults who attend the emergency room for acute asthma”. The Cochrane Database of Systematic Reviews 18.3 (2007): CD003000.
- Smith S., et al. “Standard versus patient-centred asthma education in the emergency department: a randomised study”. The European Respiratory Journal 31.5 (2008): 990-997.
- Schatz M., et al. “Follow-up after acute asthma episodes: what improves future outcomes?” Proceedings of the American Thoracic Society 6.4 (2009): 386-393.
- Reid J., et al. “Asthma management in the emergency department”. Canadian Respiratory Journal 7.3 (2000): 255-260.
- PharmacoEconomics & Outcomes News. 2000 Nov; 287 Education-Programme-Worthwhile. (2017).
- Silman AJ and Macfarlane GJ. Epidemiological Studies: A Practical Guide. 2nd ed. Cambridge University Press; (2004).
- Rosenbaum PR and Rubin DB. “Constructing a control group using multivariate matched sampling methods that incorporate the propensity score”. American Statistical Association 39.1 (1985): 33-38.
- Steyerberg EW. “Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating”. Springer (2009).
- Barnes PJ., et al. “The costs of asthma”. The European Respiratory Journal 9.4 (1996): 636-642.
- British Guidelines on the Management of Guidelines Network. British Thoracic Society (2017).
- Adams JY., et al. “The patient with asthma in the emergency department”. Clinical Reviews in Allergy & Immunology 43.1-2 (2012): 14-29.
- Abisheganaden J., et al. “Peak expiratory flow rate guided protocol did not improve outcome in emergency room asthma”. Singapore Medical Journal 39.11 (1998): 479-484.
- Brusasco V. “Usefulness of peak expiratory flow measurements: is it just a matter of instrument accuracy”? Thorax 58.5 (2003): 375-376.
- Nathan RA., et al. “Development of the asthma control test: a survey for assessing asthma control”. Journal of Allergy and Clinical Immunology 113.1 (2004): 59-65.
- Cyedulka R. Managing Acute Exacerbations and Influencing Future Outcomes in the Emergency Department Update on the National Asthma Education and Prevention Program Guidelines. In: American College of Emergency Physician (2016).
- Prabhakaran L., et al. “Was it easy to use an Asthma Control Test (ACT) in different clinical practice settings in a tertiary hospital in Singapore?” Annals of the Academy of Medicine 38.12 (2009): 1064-1069.
- Beckert L Moran A. “Asthma management in the Asia-Pacific region”. Respirology 19.1 (2014): 1-2.
- Cazzola M and Curradi G. “How to prevent relapse after acute exacerbation of asthma?” Polish Archives of Internal Medicine 117.11-12 (2007): 487-490.
Citation:
Neo Lay Ping., et al. “Implementation and Impact of Asthma Programme at Emergency Department.” Pulmonary Research and
Respiratory Care 1.1 (2017): 31-43.
Copyright: © 2017 Neo Lay Ping., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.