Case Report
Volume 2 Issue 2 - 2018
Pulmonary Aspergillosis: A Rare Presentation as Chronic Necrotizing Pulmonary Aspergillosis (CNPA).
1Director and Head of Department of Pulmonary Medicine, Ruby Hall Clinic, Pune, India
2Senior Resident, Department of Pulmonary Medicine, Ruby Hall Clinic, Pune, India
2Senior Resident, Department of Pulmonary Medicine, Ruby Hall Clinic, Pune, India
*Corresponding Author: Amir M. Khoja, Director and Head of Department of Pulmonary Medicine, Ruby Hall Clinic, Pune, India.
Received: May 29, 2018; Published: September 27, 2018
Abstract
Aspergillus is a fungus which may lead to a variety of infectious, allergic diseases of lungs depending upon host’s immune status & pulmonary structure [1]. Chronic necrotizing pulmonary aspergillosis is a locally invasive subacute infection most commonly seen in patients with altered local defense from preexisting chronic lung disease.
We are presenting a case of 66 year male patient reformed smoker, case of COPD who was on regular treatment with inhaled bronchodilator & corticosteroids for last 15 yrs. He presented with c/o breathlessness, cough with expectoration, hemoptysis, fever, weight loss since one month. Chest x-ray initially showed left sided midzone and lower zone consolidation with synpneumonic effusion which progressed to hydropneumothorax & treated with chest tube drainage. Brown coloured pus with persistent bronchopleural fistula was seen. Bronchoscopic aspirates grown Aspergillus Flavus. Treated with Tab. Voriconazole 200 mg for 6 months. ICD was removed after 3 months.
Keywords: Aspergillosis; Necrotizing Pneumonia
Abbreviations: CNPA: Chronic necrotizing pulmonary aspergillosis; ICD: Intercostal Drain
Introduction
Aspergillus species are ubiquitous fungi that are widespread in the environment and commonly isolated. From both outdoor (soil, plant debris) and indoor environment, including hospitals. Aspergillosis refers to the spectrum of disease caused by aspergillus species acquired by inhalation of airborne spores. The Presentation of aspergillosis is ranging from allergic reactions to colonization of pre-existing pulmonary. Cavities to invasion and destruction of lung tissue with pyaemic spread to the brain, skin and other organs [1-3]. They may initiate exaggerated immune response as seen in hypersensitivity pneumonitis [1] & Allergic Broncho pulmonary aspergillosis [2]. In contrast, in immune deficient hosts aspergillus invades the Airways causing invasive pulmonary aspergillosis [2].
Case History
66 year male patient, case of COPD & was on irregular treatment with inhaled bronchodilator & corticosteroids for last 15 years, was a reformed smoker with 30 pack year, alcoholic for 30 years. He was nondiabetic and not immunocompromised. He presented with cough with expectoration & progressive shortness of breath, since three months. Sputum was initially mucopurulent, later thick, and brown. He also had left sided chest pain more on deep inspiration & increases on coughing. He had high grade fever, anorexia & weight loss of six kgs in three months.
Admitted in outside hospital and treated as community acquired pneumonia. He underwent pleural tapping around 850cc, it was exudative. Chest x-ray showed right mid zone and lower zone consolidation. CT thorax initially was showing lingula, left lower lobe & right middle consolidation [figure 2(A)]. He received multiple IV antibiotics before coming to us.
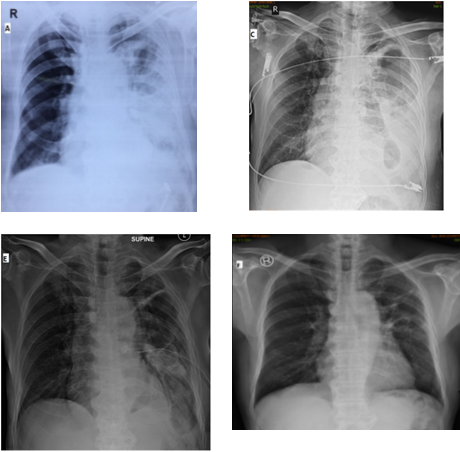
On admission he was tachypneic with respiratory rate of 24/min and heart rate of 98/min. Examination findings suggestive of decreased respiratory movements on left side; on auscultation coarse crepetations in left mammary, axillary and interscapular area with decreased air entry in infraaxillary area; & ronchi on right hemithorax. Routine labs corresponding to leukocytosis with WBC count 24300/cc & Hb 13 gm%, urea 53 mg/dl, creatinine was 0.8 mg/dl, serum albumin 1.9gm/dl. Chest x-ray showed left midzone thick walled cavity with mid & lower zone consolidation with pleural effusion. Repeat CT thorax after 15 days showed left necrotizing pneumonia with hydro-pneumothorax [figure 2 (B)]. USG thorax suggestive of left pleural effusion with internal echos. Chest tube insertion was done, which drained initially necrotic, thick brown coloured semisolid material [figure 3]. There was persistent bronchopleural fistula of grade three.
Bronchoscopy showed left upper lobe, lingula & lower lobe inflamed mucosa with thick purulent secretions plus stenosis of lower lobe bronchus. Gram stain of bronchial aspirates showing gram negative bacilli & ZN stain of the same was negative. Fungal Culture grown Aspergillus Flavus.
He started on Tab. Voriconazole 200mg, twice a day for 4 months followed by once a day for 2 months. ICD was kept for 3 months after which it was removed when drain was <10cc/day & after confirming closure of BPF. On follow up patient improved clinically as well as radiologically [figure 1].
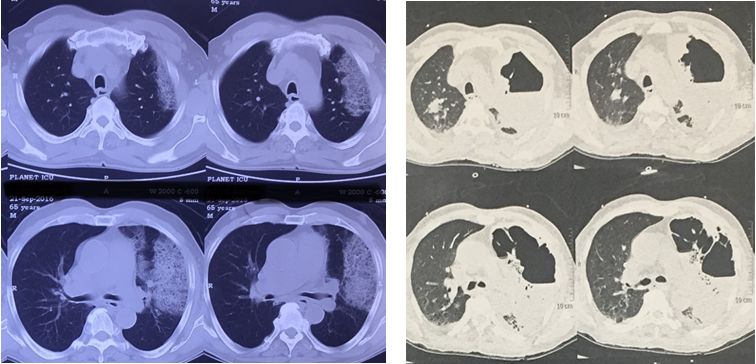
Figure 2A: CT thorax on showing consolidation in lingula & left lower lobe.
Figure 2B: repeat CT thorax after 15 days shows left side necrotizing pneumonia with hydropneumothorax.
Figure 2B: repeat CT thorax after 15 days shows left side necrotizing pneumonia with hydropneumothorax.
Discussion
In 1981, Gefter., et al. [2] described a locally invasive form of disease that he called semi-invasive pulmonary aspergillosis. A few months later, Binder., et al. [1] described similar locally invasive form of disease that he called Chronic necrotizing pulmonary aspergillosis (CNPA). It corresponds to an indolent process of lung destruction caused by the Aspergillus fungus, generally A. fumigates [4]. This is different from an aspergilloma, as a pre-existing cavity is not needed, although a cavity may develop in the lung as a secondary phenomenon due to destruction by the fungus. In contrast to invasive aspergillosis, CNPA occurs over a period of months to years and there is no vascular invasion or dissemination to other organs. The mainstay of treatment is antifungal agents like Amphoterecin B, Itraconazole or Voriconazole. Surgical resection has limited role.
CNPA is an indolent, cavitary and infectious process of the lung parenchyma secondary to local invasion by Aspergillus species, usually A. fumigatus [4]. CNPA is associated with considerable morbidity and mortality [8, 9]. Often, the diagnosis is not made early in the course of illness [9]. Even when promptly diagnosed, the pulmonary and systemic abnormalities and potentially toxic therapy combine to make medical treatment only variably effective. Most patients are poor candidates for pulmonary resection, and postoperative complications are common.
Risk factors: CNPA usually affects middle-aged and elderly patients with altered local defences, associated with underlying chronic lung diseases such as COPD, previous pulmonary tuberculosis, thoracic surgery, radiation therapy, pneumoconiosis, cystic fibrosis, lung infarction or sarcoidosis [4]. It may also occur in patients who are mildly immunocompromised due to diabetes mellitus, alcoholism, chronic liver disease, low-dose corticosteroid therapy, malnutrition, or connective tissue diseases such as rheumatoid arthritis and ankylosing spondylitis [9]. Mannose-binding lectin polymorphism may play a role in the pathogenesis of CNPA.Diagnostic criteria for CNPA [5]
- Clinical:Chronic (>1 month) pulmonary or systemic symptoms, including at least one of: weight loss, productive cough or haemoptysis. No overt immunocompromising conditions (e.g. haematological malignancy, neutropenia, organ transplantation)
- Radiological: Cavitary pulmonary lesion with evidence of paracavitary infiltrate New cavity formation, or expansion of cavity size over time
- Laboratory: Elevated levels of inflammatory markers eg. CRP, ESR; Isolation of Aspergillus spp. from pulmonary or pleural cavity; positive serum Aspergillus precipitin test. Histopathology examination which is not always positive. Exclusion of other pulmonary pathogens, by results of appropriate cultures and serological tests, that are associated with similar disease presentation, including mycobacteria and endemic fungi.
Treatment
The mainstay of treatment for CNPA is the antifungal therapy. Amphotericin B was initially used in doses of 0.5– 1 mg /kg/day (4–5 mg/kg/day for the lipid formulation) with favourable results [9-11]. Itraconazole later became an effective alternative to the relatively toxic amphotericin B [5-11]. More recently, Voriconazole has emerged as a primary therapy for CNPA.
The mainstay of treatment for CNPA is the antifungal therapy. Amphotericin B was initially used in doses of 0.5– 1 mg /kg/day (4–5 mg/kg/day for the lipid formulation) with favourable results [9-11]. Itraconazole later became an effective alternative to the relatively toxic amphotericin B [5-11]. More recently, Voriconazole has emerged as a primary therapy for CNPA.
The recent statement of the American Thoracic Society favours giving either Voriconazole or Itraconazole for mild to moderate disease until resolution or stabilization of the clinical and radiographic manifestations, while in patients with severe disease, initial therapy with intravenous amphotericin B or intravenous Voriconazole should be considered [5].
Surgical resection has a minor role in the treatment of CNPA, being reserved for healthy young patients with focal disease and good pulmonary reserves, patients not tolerating antifungal therapy and patients with residual localised but active disease despite adequate antifungal therapy. BINDER., et al. [9] reported that 90% of patients who underwent surgical resection had good responses, but surgery was associated with significant post-operative complications.
The reported mortality of CNPA varies widely and may be limited by incomplete follow-up [11]. Mortality was 39% in American reports, but less than 10% in European reports using itraconazole [11-16].
Conclusion
In chronic lung disease patients Aspergillosis in the form of chronic necrotizing pneumonia can occur. It presents as consolidation followed by cavitation. In such scenario we should consider CNPA.
Conflict of interest: Nil
References
- Kousha M., et al. "Pulmonary aspergillosis: a clinical review." European Respiratory Review20.121 (2011): 156-174.
- Soubani., et al. "The clinical spectrum of pulmonary aspergillosis." Chest 121.6 (2002): 1988-1999.
- Zmeili., et al. "Pulmonary aspergillosis: a clinical update." Journal of the Association of Physicians100.6 (2007): 317-334.
- Thompson., et al. "Pulmonary aspergillosis." Seminars in Respiratory and Critical Care Medicine New York: Thieme Medical Publishers 1994 (2008).
- Seabury JH., et al. "The pathogenic spectrum of aspergillosis.” American Journal of Clinical Pathology 40 (1963): 21-33.
- Rosenberg., et al. "Clinical and immunologic criteria for the diagnosis of allergic bronchopulmonary aspergillosis." Annals of Internal Medicine 86.4 (1977): 405-414.
- Gerson., et al. "Prolonged granulocytopenia: the major risk factor for invasive pulmonary aspergillosis in patients with acute leukemia." Annals of internal medicine100.3 (1984): 345-351.
- Gefter., et al. "Semi-invasive" pulmonary aspergillosis: a new look at the spectrum of aspergillus infections of the lung." Radiology 140.2 (1981): 313-321.
- Binder., et al. "Chronic necrotizing pulmonary aspergillosis: a discrete clinical entity." Medicine 61.2 (1982): 109.
- Sánchez CD., et al. "Aspergillus y pulmón.” Archivos de Bronconeumología 40 (2004): 114-122.
- Saraceno., et al. "Chronic Necrotizing Pulmonary Aspergillosis*: Approach to Management." Chest 112.2 (1997): 541-548.
- Grahame-Clarke., et al. "Chronic necrotizing pulmonary aspergillosis and pulmonary phycomycosis in cystic fibrosis." Respiratory medicine 88.6 (1994): 465-468.
- Crosdale., et al. "Mannose-binding lectin gene polymorphisms as a susceptibility factor for chronic necrotizing pulmonary aspergillosis." The Journal of infectious diseases184.5 (2001): 653-656.
- Denning., et al. "Chronic cavitary and fibrosing pulmonary and pleural aspergillosis: case series, proposed nomenclature change, and review." Clinical infectious diseases 37.Supplement_3 (2003): S265-S280.
- Caras., et al. "Chronic necrotizing pulmonary aspergillosis: pathologic outcome after itraconazole therapy." Mayo Clinic Proceedings Elsevier (1996).
- Limper., et al. "An official American Thoracic Society statement: treatment of fungal infections in adult pulmonary and critical care patients." American journal of respiratory and critical care medicine 183.1 (2011): 96-128.
Citation:
Amir M. Khoja., et al. “Pulmonary Aspergillosis: A Rare Presentation as Chronic Necrotizing Pulmonary Aspergillosis (CNPA).”
Pulmonary Research and Respiratory Care 2.2 (2018): 169-173.
Copyright: © 2018 Amir M. Khoja., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.