Case Report
Volume 1 Issue 1 - 2018
Incidental Massive Pulmonary artery Tumour Thrombus Associated with Malignancy- an Anaesthetic Encounter
1Department of Anaesthesiology, Regional Cancer Centre, Trivandrum 695 011, India
2MBBS, Post graduate, Department of Anaesthesiology, Regional Cancer Centre, Trivandrum 695 011, India
3MD ,PDCC, Professor and Head, Department of Anaesthesiology, Regional Cancer Centre, Trivandrum 695 011, India
2MBBS, Post graduate, Department of Anaesthesiology, Regional Cancer Centre, Trivandrum 695 011, India
3MD ,PDCC, Professor and Head, Department of Anaesthesiology, Regional Cancer Centre, Trivandrum 695 011, India
*Corresponding Author: Dr. Jithumol Thankam Thomas, Department of Anaesthesiology, Regional Cancer Centre, Trivandrum 695 011, India.
Received: August 20, 2017; Published: February 28, 2018
Abstract
Malignancy is an hypercoagulable state. Tumour thrombus in the pulmonary artery have been reported found at autopsy in up to 30% of patients of certain malignancies. Massive tumour thrombus in the pulmonary artery carries a high risk of sudden cardiopulmonary decompensation. We present a case-report highlighting the anaesthetic management of a case of pulmonary metastases invading the PA causing in situ (PA)thrombosis in a known patient of metastatic malignant spindle cell sarcoma. Before planning the surgical procedures, adequate anticoagulation must be achieved to prevent further complication of DVT, thromboembolism, and pulmonary embolism. The risk of stopping the anticoagulation prior to surgery must be considered and adequately discussed with the patient and surgeons. The anaesthetic plan must be selected keeping in mind the coagulation status and the need of anticoagulation in the postoperative period.Hemodynamic stability, adequate pain relief and close monitoring will help to tide over the perioperative period in such patients.
Keywords: Pulmonary thrombus; Anaesthesia; Spindle cell sarcoma; Tumour emboli
Introduction
Pulmonary tumor thrombus refers to the identification of tumor within pulmonary arteries and/or capillaries. [1] Patients with malignancy have an increased tendency to develop pulmonary thromboembolism due to their hypercoagulable state. [2] Patients with massive pulmonary thrombus are prone to undergo sudden cardiopulmonary decompensation, hence anaesthetic management of such patients can be very challenging. [3] Our concerns in this case included problems due to anticoagulation, potential sudden cardiovascular collapse, right heart failure and even death
Case Report
A 32 year old male patient presented with a swelling on the lateral aspect of left wrist which grew in size rapidly over 3 months. A similar swelling on the right wrist was operated 2 years back and was diagnosed as malignant spindle cell sarcoma of possible neural origin on tissue biopsy. Patient was posted for wide excision with left thumb amputation. A preoperative routine examination revealed suspicious bilateral pulmonary lesions in the chest Xray. This warranted further investigation and hence a CT thorax was done which revealed enlarged ipsilateral axillary nodes, bilateral pulmonary metastasis and a hidden killer- a massive partially occluding saddle thrombus at the pulmonary artey bifurcation extending to segmental branches- possibly tumour thrombus [Figure 1&2]. Preoperative electrocardiogram showed normal sinus rhythmn. Patient was asymptomatic and had no other comorbid conditions.
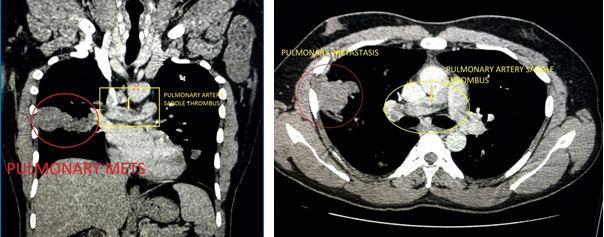
Figures 1&2: Massive partially occluding saddle thrombus at the
pulmonary artery bifurcation extending to segmental branches.
Preoperatively, patient was started on unfractioned heparin infusion targeting APTT of 75-100. After 4 days of heparin infusion patient was taken up for the surgery. Since patient refused regional anaesthesia and insisted on general anaesthesia, patient was provided the same. Our concerns in this case included problems due to anticoagulation, potential sudden cardiovascular collapse, right heart failure and even death.
He was premedicated with Inj Midazolam 1 mg IV and Fentanyl 2 mcg/kg and pre-oxygenated for 3 minutes. He was induced with Inj Etomidate 0.3 mg/kg and tracheal intubation was facilitated with Inj Vecuronium 0.1 mg/kg. Anaesthesia was maintained with Oxygen Air mixture and Sevoflurane. Our anaesthetic goals in this patient were to maintain systemic vascular resistance and optimal preload to the heart, to maintain sinus rhythm and to avoid rise in mean pulmonary artery pressure due to hypoxaemia, hypercarbia and pain.
Dexmedetomidine infusion was started after a bolus dose to provide analgesia and sedation with hemodynamic stability. Beside the routine ASA monitoring, radial arterial line was cannulated and peripherally inserted central venous catheter was inserted. Patient was ventilated with low tidal volume of 6 ml/kg and respiratory rate was adjusted to maintain normocarbia. Plateau pressure of less than 30 cm H2O was maintained. Care was taken to avoid hypoxia, hypercarbia and wide fluctuations in blood pressure. For postoperative pain relief, radial nerve, lateral cutaneous nerve of forearm and median nerve were anesthetized at the elbow under ultrasound guidance with 0.2% ropivacaine using a 22G iv cannula which was then left in situ at the site of the radial nerve for intermittent boluses in the postoperative period [Figure 3]. Intra operative period was uneventful and patient was extubated. He was restarted on low molecular weight heparin 12 hours after surgery. Boluses of 5-6 ml of 0.2% ropivacaine was administered every 6th hourly through the cannula left at the radial nerve site at the elbow. Patient was comfortable, pain free and hemodynamically stable postoperatively.

Figures 3: IV cannula left at radial nerve site at the elbow for
intermittent boluses of local anaesthetic.
Discussion
Malignancies such as carcinoma of the breast, hepato-cellular carcinoma, renal cell carcinoma, choriocarcinoma, carcinoma of stomach, and malignant melanoma are known to have PA tumour emboli in almost up to one-third of cases. Pulmonary arteries may be involved by contiguous extension of tumour thrombus from a known malignancy at a distant site. [1,3] Pulmonary tumour emboli is an end stage manifestation of a malignancy with poor prognosis
Because of its unique anatomy with rich capillary network and central location in the circulatory system, lungs are the most frequent sites for haematogenous metastases from a variety of malignant tumours. Also, pulmonary arteries offer less resistance to neoplastic invasion as compared to systemic vessels, possibly because of a lower pressure gradient across the vessel wall. [1]
Pulmonary arterial obstruction causes elevation in pulmonary vascular resistance (PVR), increase in alveolar dead space and redistribution of blood flow impairing gas exchange. As right ventricular afterload increases, tension rises in the right ventricular wall and this may lead to dilatation, dysfunction, and ischemia of the right ventricle. Sudden cardiovascular collapse and right heart failure can occur. [4] As soon as massive PE or thrombus is suspected, anticoagulation with high-dose unfractionated heparin should be started with a bolus dose followed by infusion along with simultaneous haemodynamic support with fluid, inotropes and vasopressors as indicated by the clinical situation.
Anesthetising a patient with massive pulmonary thrombus can be challenging especially when general anaesthesia has to be administered. Intraoperative fluctuations in blood pressure, hypoxia, hypercarbia, increase in pulmonary vascular resistance can be deleterious and may precipitate sudden right heart failure. [5] Anaesthetic technique of choice in such patients should be regional wherever possible. Direct laryngoscopy during general anaesthesia causes increased sympathetic outflow leading to increased pulmonary vascular resistance and thereby precipitating acute right heart failure. Over use of narcotics, inhalational agent or muscle relaxants to control sympathetic response can inadvertently reduce cardiac output and hence coronary perfusion. [6] Hence if general anaesthesia has to be provided, a balanced general anaeshesia technique with adequate pain relief and hemodynamic stability must be planned for such patients. That was the reason why Dexmedetomidine infusion was used so that analgesia and sedation are provided so that other agents such as narcotics, inhalational agents and muscle relaxants were used sparingly rather than liberally.
The use of peripheral neural blockade in an anticoagulated patient was done carefully using ultrasound guidance. This is a very cost effective method of providing continuous peripheral nerve blockade and no other analgesic was required to keep the patient comfortable
Conclusion
Vigilant and meticulous anaesthesia with attention to detail, adequate monitoring help to tide over perioperative period even in patients who have life threatening co morbidities. Dexmedetomidine and regional nerve blocks are useful adjuncts in providing balanced anaesthesia for patients with life threatening co morbidities such as massive pulmonary thrombus. Thrombus in Pulmonary artery need not make a patient unfit for anaesthesia!
References
- Roberts KE., et al. “Pulmonary tumor embolism: a review of the literature”. The American Journal of Medicine 115.3 (2003): 228-232.
- J Debnath., et al. “Pulmonary metastases: a rare cause for pulmonary artery invasion and in situ pulmonary artery thrombosis-demonstration with multidetector computed tomography”. Medical Journal Armed Forces India 68.1 (2012): 65-67.
- Engelke C., et al. “High resolution CT and CT angiography of peripheral pulmonary vascular disorders”. RadioGraphics 22.4 (2002): 739–764.
- Wood KE. “Major pulmonary embolism: Review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary Embolism”. Chest 121.3 (2002): 877–905.
- Blaise G., et al. “Pulmonary Arterial Hypertension. Pathophysiology and anesthetic approach”. Anesthesiology 99.6 (2003): 1415-1432.
- Chidananda Swamy MN., et al. “Anaesthetic management of a patient with severe pulmonary arterial hypertension for renal transplantation”. Indian Journal of Anaesthesia 61.2 (2017): 167-169
Citation:
Jithumol Thankam Thomas., et al. “Incidental Massive Pulmonary artery Tumour Thrombus Associated with Malignancy- an
Anaesthetic Encounter”. Anaesthesia, Critical Care and Pain Management 1.1 (2018): 63-66.
Copyright: © 2018 Jithumol Thankam Thomas., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.