Editorial
Volume 1 Issue 2 - 2018
Palmitoylethanolamide Formulations in Chronic Pain, Which to Select?
1Institute Neuropathic Pain, the Netherlands
2Joyce McSwan, Managing Director Pain WISE Pty Ltd; Clinical Director - GCPHN Persistent Pain Program Queensland, Australia
2Joyce McSwan, Managing Director Pain WISE Pty Ltd; Clinical Director - GCPHN Persistent Pain Program Queensland, Australia
*Corresponding Author: Jan M Keppel Hesselink, Institute Neuropathic Pain, the Netherlands.
Received: July 30, 2018; Published: August 17, 2018
Abstract
Palmitoylethanolamide (PEA) is increasingly popular as a compound with analgesic and anti-inflammatory properties. Anno 2018
nearly 700 PubMed indexed publications can be found, and since 2005 an increasing number of publications have discussed and
presented clinical data. Two different companies, Epitech Srl. and Russell Science Ltd. introduced innovative formulations of PEA,
containing fine and ultra-fine PEA particles (micro-PEA) some years ago. Since these formulations were developed, various me-too
formulations of unknown quality have entered the market, containing mostly unprocessed PEA. Therefore there is confusion about
which PEA formulation to choose from. As it currently stands, only the two first formulations introduced in the market, prepared
via patented procedures, have given rise to sufficient plasma levels and have been clinically assessed by medical doctors, with its
results published in peer reviewed Journals. Unprocessed PEA is highly unlikely to lead to measurable increases in plasma levels. It
is therefore recommended to use PEA formulations containing micro-PEA formulations, such as ultra-micronized (PEA-um) and the
optimized (PEA-opt) formulations.
Key words: Endocannabinoids; Neuropathic; Analgesia; Micronized; Optimized
Introduction
PEA as analgesic and anti-inflammatory compound
PEA was discovered in the middle of the last century, by scientists of Merck. [1] During some decades the compound was known for its prophylactic properties in respiratory disorders, and was marketed under two different brand names in the period between 1980 to 2015, Palmidrol and Impulsion. These formulations are no longer available. Palmidrol was a drinkable suspension, and Impulsion was a tablet containing 500 mg PEA. The indication for both formulations was respiratory infection, and in the 70s and 80s a number of clinical studies supported the efficacy and safety of PEA in this field, especially in the prophylaxis and treatment of the flu. [2] However, due to the absence of insight in the exact mechanism of action, PEA did become a mainstream treatment. PEA belongs to the class of autacoids, local tissue-hormones, with broad clinical applications, from glaucoma to neuropathic pain. [3,4]
PEA was discovered in the middle of the last century, by scientists of Merck. [1] During some decades the compound was known for its prophylactic properties in respiratory disorders, and was marketed under two different brand names in the period between 1980 to 2015, Palmidrol and Impulsion. These formulations are no longer available. Palmidrol was a drinkable suspension, and Impulsion was a tablet containing 500 mg PEA. The indication for both formulations was respiratory infection, and in the 70s and 80s a number of clinical studies supported the efficacy and safety of PEA in this field, especially in the prophylaxis and treatment of the flu. [2] However, due to the absence of insight in the exact mechanism of action, PEA did become a mainstream treatment. PEA belongs to the class of autacoids, local tissue-hormones, with broad clinical applications, from glaucoma to neuropathic pain. [3,4]
In the early 90s it was the Nobel laureate Rita Levi-Montalcini who first discovered indicators for the mechanism of action, and it
seemed that PEA as an autacoid regulated and inhibited the mast cell. [5-7] Various animal models supported PEA’s analgesic effects.
[6] Later, along the lines of her work, it was recognized that PEA could inhibit many immune-competent cells, such as the glia. The key
characteristics of PEA appears therefore to target some new non-neuronal targets, the glia and other immune-competent cells such as
the mast cells. [7] In the beginning of this century the first data were published on the clinical efficacy of a PEA formulation containing
ultrafine PEA particles, produced via a patented procedure. [8] Some years later a new mechanism of action was presented, based on the
high affinity of PEA for the ‘master-anti-inflammatory nuclear switch’, the nuclear receptor peroxisome proliferator‐activated receptor‐α
(PPAR-alpha). [9] The first pivotal sand supportive studies however, evaluating such formulation, appeared in a Spanish Journal and was
therefore not widely read. [10,11]
PEA as an effective and safe analgesic
Since the early 2000s, the analgesic properties of PEA were realized over a wide range of chronic pain states. [12-17] Serious adverse events have never been documented to date. In 2012 the clinical analgesic effects of many hundreds of patients, suffering from chronic pain syndromes, who were treated with PEA in a special micro-PEA formulation was summarized in the first clinical review. [13] This paper was instrumental to introduce the PEA concept to a broader audience, as most studies and papers up to that date were published in the Italian and Spanish literature. Western physicians were at that time not aware of the clinical relevance of PEA in the treatment of chronic pain disorders in general, and more specific in neuropathic pain. Soon after the publication of the first review paper a case series was presented, where PEA was effective in treating pain in chronic idiopathic axonal neuropathy and related painful neuropathies. [14] Other studies and meta-analysis supporting PEA’s role as an analgesic compound followed. [15]
Since the early 2000s, the analgesic properties of PEA were realized over a wide range of chronic pain states. [12-17] Serious adverse events have never been documented to date. In 2012 the clinical analgesic effects of many hundreds of patients, suffering from chronic pain syndromes, who were treated with PEA in a special micro-PEA formulation was summarized in the first clinical review. [13] This paper was instrumental to introduce the PEA concept to a broader audience, as most studies and papers up to that date were published in the Italian and Spanish literature. Western physicians were at that time not aware of the clinical relevance of PEA in the treatment of chronic pain disorders in general, and more specific in neuropathic pain. Soon after the publication of the first review paper a case series was presented, where PEA was effective in treating pain in chronic idiopathic axonal neuropathy and related painful neuropathies. [14] Other studies and meta-analysis supporting PEA’s role as an analgesic compound followed. [15]
In addition to its anti-inflammatory properties, these target sites may be a reason for its success in treating various types of neuropathic
pain. In a number of clinical studies involving nerve compression syndromes, such as sciatic pain, a micro-PEA formulation proved
to be safe and effective. [16] Some studies however, assessed a dose-range that was probably too low (600 mg/day). In one of the more
recent studies for instance, in carpal tunnel syndrome, it was stipulated that dose might need to be around 1200 mg/day. [17] This is in
line with our clinical impression, and as the safety margin of the compound proved to be excellent, we always recommend to use the initiating
dose of 1200 mg/day, and in case of insufficient effect, to double the dose after some weeks. However, formal dose-finding studies
in the higher dose-range are still absent.
The dose-range selected for studies in humans is between 5 mg/ kg bodyweight (BW) to 100 mg/kg BW. In most studies 600 or 1200
mg daily has been administered. Since 2011, collaborations with the two patented PEA formulations have enabled us to provide more
accurate dosing schedules that have achieved faster dose escalations. A minimal dose of 1200 mg/day is now recommended and in the
case of insufficient effect, the dose can also be doubled rafter 6-8 weeks and reassessed for effectiveness during the next 2-3 months of
its use. Recent studies support faster dose escalations and a higher dose-range. Low doses (below 600mg/day) are discouraged.
Micro-PEA: measurable and therapeutic relevant plasma levels
Micro-PEA formulations are scarce in the world, and are characterized by a sufficient amount of fine and ultrafine particles. The clinical articles so far published have all been conducted with formulations containing micro-PEA, and the two main producers are the Italian company Epitech, and the Cypriote company Russell Science. Both these companies have prepared their formulations based on patented production procedures. These specialized patented procedures have resulted in formulations containing micro-PEA (Epitech) and in the case of Russell Science, excipient free formulations containing micro-PEA. [18] Such formulations have been developed based on pharmaceutical indications that lipid compounds might be compromised in the absorption by for instance magnesium stearate; furthermore, its genotoxic potential is still unexplored. [19,20]
Micro-PEA formulations are scarce in the world, and are characterized by a sufficient amount of fine and ultrafine particles. The clinical articles so far published have all been conducted with formulations containing micro-PEA, and the two main producers are the Italian company Epitech, and the Cypriote company Russell Science. Both these companies have prepared their formulations based on patented production procedures. These specialized patented procedures have resulted in formulations containing micro-PEA (Epitech) and in the case of Russell Science, excipient free formulations containing micro-PEA. [18] Such formulations have been developed based on pharmaceutical indications that lipid compounds might be compromised in the absorption by for instance magnesium stearate; furthermore, its genotoxic potential is still unexplored. [19,20]
There are clear indicators that formulations containing micro-PEA, such as ‘PEA-um’ (ultramicronised) and ‘PEA-opt’ (optimized),
lead to measurable and therapeutically relevant plasma levels. We will present some of these data. As animal data are published in more
detail in various papers, we will review only one of the more recent studies, where naïve unprocessed PEA has been compared to a
micro-PEA version. Subsequently we will present and discuss some new data from the University of Wageningen, the Netherlands, where
plasma levels have been measured in 3 volunteers, using a micro-PEA formulation containing PEA-opt.
It was clear in a recent animal study, that micro-PEA, ‘PEA-um’, containing ultrafine particles and produced according to a patented
procedure, lead to considerably higher levels of PEA in the blood than unprocessed PEA. [21] More specifically the administration of
an ultrafine PEA formulation led to clear plasma level increases in a rat model, while unprocessed PEA did not lead to a rise in plasma
levels. The micro PEA formulation was also more active in pain- and inflammation models, and was capable of down-regulating spinal
inflammatory and oxidative pathways. These recent findings also suggest that spinal mechanisms are involved in the anti-hyperalgesic
effect of PEA in inflammatory pain. However, these mechanisms of action were only achieved with the use of the patented formulations
which contain sufficient ultrafine PEA. In light of a number of recent PEA formulations, mostly low priced, containing only coarsely
grinded PEA, these data point out that to achieve the full beneficial effects of PEA, one should select the patent-protected micronization
techniques.
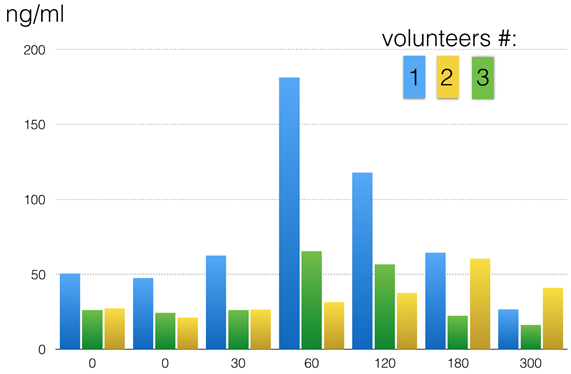
Figures 1: Plasma levels of 3 volunteers after intake of 800 mg PEA-opt (2 x 400 mg PEA-opt capsules): clearly this formulation leads to a clinical relevant rise in plasma levels of PEA, and the peak (C-max) is at least more than double of the base-line levels, which are around 25 ng/ml. There is an individual difference in time-to peak, for instance volunteer 1 reaches Cmax after 60 minutes, while volunteer 2 reaches Cmax after 180 minutes.
The pharmacokinetic properties of the micro-PEA formulation of the PEA-opt formulation were explored in a first pilot study by
professor Renger Wit Kamp at the University of Wageningen, the Netherlands (personal communication, data on file). [22] The aim of
this pilot study was to investigate if PEA-opt is taken up in the blood and to collect some first indications related to the kinetics of PEAopt.
PEA-opt is a specific micro PEA formulation free of any excipients which has been known to increase plasma PEA levels. In a pilot
study three healthy volunteers (see diagram, volunteers #1,2 and 3) gave consent to take part in this pilot, evaluating the kinetics of
PEA-opt capsules. It was decided that blood would be drawn at seven different time points, from baseline up to 10 hours after ingestion
of the supplement. The subjects came in fasted and at T = 0 minutes, 800 mg of PEA (2x 400mg PEA Pure, JP Russell Science Ltd) was
taken orally. The subjects remained fasted up to T=180 minutes. The blood was centrifuged and the plasma was isolated and frozen at
-80-degree C until further analysis of the samples. At baseline (fasted): 10ml blood was drawn for measuring the level of PEA in the blood without supplement. In one volunteer the baseline level was twice as high as in the other 2 (50 ng/ml versus 25 ng/ml). This volunteer
clearly showed the highest rise in PEA blood levels, and after 60 minutes after intake the plasma level was around 180 ng/ml. The other
2 volunteers showed a slower absorption, but after 60-180 minutes the PEA levels were more than doubled.
Conclusion
Studies so far have confirmed that oral micro-PEA formulations enters the blood and is capable of increasing plasma levels whilst
coarsely processed PEA does not enter the blood stream and is not able to achieve clinically effective plasma levels. Animal studies have
further demonstrated that micro-PEA formulations are superior when compared to unprocessed PEA, both from the pharmacokinetic as
well as from the pharmacodynamics perspective. To date, considerable increases in PEA plasma levels have been documented only for
patent protected micro-PEA formulations. The clinical data reviewed above further supports the clinical recommendation to start treating
with 1200 mg/day, and in case of insufficient effect after one month to double the dose.
Conflict of interest: Authors report no conflict of interest
References
- Kuehl FA., et al. “The identification of N-(2-hydroxyethyl)-palmitamide as a naturally occurring anti-inflammatory agent”. Journal of the American Chemical Society 79.20 (1957): 5577-5578.
- Keppel Hesselink JM., et al. “Palmitoylethanolamide: A Natural Body-Own Anti-Inflammatory Agent, Effective and Safe against Influenza and Common Cold”. International Journal of Inflammation (2013).
- Keppel Hesselink JM., et al. “Resolvins and aliamides: lipid autacoids in ophthalmology - what promise do they hold?” Drug Design, Development and Therapy (2016): 3133-3141.
- Keppel Hesselink JM. “Chronic idiopathic axonal neuropathy and pain, treated with the endogenous lipid mediator Palmitoylethanolamide: a case collection”. International Medical Case Reports Journal 13 (2013): 49-53.
- Aloe L., et al. “A proposed autacoid mechanism controlling mastocyte behavior”. Agents Actions 39 (1993): 145-147.
- Calignano A., et al. “Antinociceptive activity of the endogenous fatty acid amide, Palmitoylethanolamide”. European Journal of Pharmacology 419.2.3 (2001): 191-198.
- Keppel Hesselink JM. “Glia as a new target for neuropathic pain, clinical proof of concept for palmitoylethanolamide, a glia modulator”. Anaesthesia, Pain & Intensive Care 15 (2011): 143-145.
- Scarampella F., et al. “Clinical and histological evaluation of an analogue of palmitoylethanolamide, PLR 120 (comicronized Palmidrol INN) in cats with eosinophilic granuloma and eosinophilic plaque: a pilot study”. Veterinary Dermatology 12.1 (2001): 29-39.
- Lo Verme J., et al. “The nuclear receptor peroxisome proliferator‐activated receptor‐α mediates the anti‐inflammatory actions of Palmitoylethanolamide”. Molecular Pharmacology 2005: 15-19.
- Guida G., et al. “La palmitoilethanolamida (Normast®) en el dolor neuropático crónico por lumbociatalgia de tipo compresivo: estudio clínico multicéntrico”. Dolor 25 (2010): 35-42.
- Canteri L., et al. “Riducción del consumo di antiinfiammatorios y analgésicos en el tratamiento del dolor neuropático crónico en pacientes afectados por lombosciatalgia de tipo compresivo y en tratamiento con Normast® 300 mg”. Dolor 25 (2010): 227-234.
- Gatti A., et al. “Palmitoylethanolamide in the treatment of chronic pain caused by different etiopathogenesis”. Pain Medicine 13.9 (2012): 1121-1130.
- Keppel Hesselink JM. “New targets in pain, non-neuronal cells, and the role of palmitoylethanolamide”. Open Pain Journal 5 (2012): 12-23.
- Keppel Hesselink JM and Hekker TA. “Therapeutic utility of palmitoylethanolamide in the treatment of neuropathic pain associated with various pathological conditions: a case series”. Journal of Pain Research 5 (2012): 437-442.
- Paladini A., et al. “Palmitoylethanolamide, a special food for medical purposes, in the treatment of chronic pain: a pooled data meta‐analysis”. Pain Physician 19.2 (2016): 11-24.
- Keppel Hesselink JM and Kopsky DJ. “Palmitoylethanolamide, a neutraceutical, in nerve compression syndromes: efficacy and safety in sciatic pain and carpal tunnel syndrome”. Journal of Pain Research (2015): 729-734.
- Faig-Martí J and Martínez-Catassús A. “Use of palmitoylethanolamide in carpal tunnel syndrome: a prospective randomized study”. Journal of Orthopaedics and Traumatology 18.4 (2017): 451-455.
- Nestmann ER. “Safety of micronized palmitoylethanolamide (microPEA): lack of toxicity and genotoxic potential”. Food Science & Nutrition 5.2 (2016): 292-309.
- Chowhan and LH Chi. “Drug-excipient interactions resulting from powder mixing. III: solid state properties and their effect on drug dissolution”. Journal of Pharmaceutical Sciences 75.6 (1986): 534-541.
- Hobbs CA., et al. “Magnesium stearate, a widely-used food additive, exhibits a lack of in vitro and in vivo genotoxic potential”. Toxicology Reports 4 (2017): 554-559.
- Petrosino S., et al. “Oral Ultra micronized Palmitoylethanolamide: Plasma and Tissue Levels and Spinal Anti-hyperalgesic Effect”. Frontiers in Pharmacology 9 (2018): 249.
- Witkamp R. Wageningen University, the Netherlands, unpublished data on file. (2015).
Citation:
Jan M Keppel Hesselink and Joyce McSwan. “Palmitoylethanolamide Formulations in Chronic Pain, Which to Select?” Anaesthesia,
Critical Care and Pain Management 1.2 (2018): 93-97.
Copyright: © 2018 Jan M Keppel Hesselink and Joyce McSwan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.