Research Article
Volume 1 Issue 1 - 2018
Self-Blood (Immunotherapy), A New Hope for Psoriasis
1MD (Internal Medicine); DNB (E&M), Post graduate in Endocrinology & metabolism (AIIMS-Delhi) Chairman, National Institute of Health & Research, Warisaliganj (Nawada), 805130, India
2BAMS (BRABU); MHA, State Health Services, Government of Bihar, Director (Hon) Aarogyam Punarjeen, Are Garden Road Jagdeo path, Patna 14, India
3BAMS (BRABU), Director, Centre for Indigenous Medicine & Research, Warisaliganj (Nevada) Bihar, 805130, India
2BAMS (BRABU); MHA, State Health Services, Government of Bihar, Director (Hon) Aarogyam Punarjeen, Are Garden Road Jagdeo path, Patna 14, India
3BAMS (BRABU), Director, Centre for Indigenous Medicine & Research, Warisaliganj (Nevada) Bihar, 805130, India
*Corresponding Author: Avinash Shankar, MD (Internal Medicine); DNB (E&M), Post graduate in Endocrinology & metabolism (AIIMS-Delhi) Chairman, National Institute of Health & Research, Warisaliganj (Nawada), 805130, India.
Received: February 28, 2018; Published: March 14, 2018
Abstract
Psoriasis, a chronic non communicable, painful, disfiguring and disabling disease for which no cure and poses great negative impact on patient’s quality of life and can affect any age or sex. In the wake of commonly prescribed immunosuppressive or biologicals, in the present study self-blood and betamethasone injection intramuscular administration as per suggested schedule achieved beginning of improvement in all the cases by 6th month of therapy and complete absence of manifestation in all by 42 months without any adversity or withdrawal effect, considered as neutralization of generated protein responsible for increased rate of skin cell death and increased keratinocytes.
Keywords: Psoriasis; Communicable; Disabling; Immunosuppressive; Self-blood; Cell death, keratinocytes
Introduction
Psoriasis a non-contagious, non-infectious agonising auto immune disorder usually associated with immunological disorders [1-10], affects both sexes without any socio-economic variation and poses agonising encumbrance and progressively increasing in present scenario.
Its incidence varies worldwide i.e.- In European country USA has 1-3% of total population, 2-4% western world population and 7.5-8.5 million cases while in India 0.44-2.8% and affect > 10 million every year [11-13], rate of psoriasis incidence varies according to age, region, and ethinic & combination of environmental and genetic factor.
Commonly involved sites are knee, elbow, scalp, tarso, and palm, sole of feet but can appear and involve any part of the body and persons with inflammatory bowel disease are more prone Commonly offered therapeutics i.e. - modern molecule, Ayurveda, homeopath or any other, fails to ensure cure of the disease and only assure soothing effect and relieve dermal discomfort with recurrent flare up. [14-16]
Commonly used modern therapeutics are –
Synthetic retinoids, Immuno suppressor, Recombiant monoclonal antibody, Cholecalciferol orally
Topical use- = Allantoin, anthralin and Desonide
Synthetic retinoids, Immuno suppressor, Recombiant monoclonal antibody, Cholecalciferol orally
Topical use- = Allantoin, anthralin and Desonide
Aims and Objectives
Evaluation of immune boosting therapeutics i.e. Self-blood and betamethasone intramuscular to counter the antigen generated in the body and calm the antigen-antibody activity in patients of psoriasis and its sequel psoriatic arthritis
Evaluation of immune boosting therapeutics i.e. Self-blood and betamethasone intramuscular to counter the antigen generated in the body and calm the antigen-antibody activity in patients of psoriasis and its sequel psoriatic arthritis
Material & Methods
Material
Patients of psoriasis attending at the OPD of RA. Hospital & Research Centre, Warisaliganj (Nawada) Bihar and Aarogyam Punarjeevan, Ram Bhawan, Ara Garden Road, Jagdeopath, Baily Road Patna 14 with following presentation were selected. Bleeding on pulling of dry white flake of skin, a confirmatory sign of Psoriasis termed as AUSPETZ sign [17]
Patients of psoriasis attending at the OPD of RA. Hospital & Research Centre, Warisaliganj (Nawada) Bihar and Aarogyam Punarjeevan, Ram Bhawan, Ara Garden Road, Jagdeopath, Baily Road Patna 14 with following presentation were selected. Bleeding on pulling of dry white flake of skin, a confirmatory sign of Psoriasis termed as AUSPETZ sign [17]
Common presentation are [18-19]
- Plaques of red skin often covered with loose silvery scales
- Itching
- Pain
- Occasionally with cracks and bleed
- Plaques of scales or crust on the scalp
- May be associated with psoriatic arthritis (stiff, swollen and painful joint)
- Thickened, ridged and pitted nail
- Stiff and swollen joint
Types of lesion Characteristics
Pustular psoriasis : Red and scaly skin on the palms of the hands and/or feet
With tiny pustules
Guttate psoriasis: Often starts in childhood or young adulthood, small, red Spots, mainly on the torso and limbs. Triggers may be
Respiratory infections,
Strep throat, tonsillitis, stress, injury to the skin, and
Use of anti-malarial and beta-blocker medications.
Inverse psoriasis: bright red, shiny lesions that appear in
Skin folds, such as the armpits, groin area, and under
The breasts
Erythrodermic psoriasis: Periodic, fiery redness of the skin and shedding of
Scales in sheets;
Pustular psoriasis : Red and scaly skin on the palms of the hands and/or feet
With tiny pustules
Guttate psoriasis: Often starts in childhood or young adulthood, small, red Spots, mainly on the torso and limbs. Triggers may be
Respiratory infections,
Strep throat, tonsillitis, stress, injury to the skin, and
Use of anti-malarial and beta-blocker medications.
Inverse psoriasis: bright red, shiny lesions that appear in
Skin folds, such as the armpits, groin area, and under
The breasts
Erythrodermic psoriasis: Periodic, fiery redness of the skin and shedding of
Scales in sheets;
Duration of Study: April 2003-March 2005
Follow up Period: 2015-2018
Follow up Period: 2015-2018
Methods
Selected patients were interrogated for the history of diseases, drugs taken and their response, examined clinically and investigated for typing the lesion, base line biological status to adjudge the clinical effect or adversity
Selected patients were interrogated for the history of diseases, drugs taken and their response, examined clinically and investigated for typing the lesion, base line biological status to adjudge the clinical effect or adversity
Selected patients were classified in to various grade of severity as per clinical presentation [19-20]
Intensity
Erythema: Absent Mild Moderate Severe Very severe
Erythema: Absent Mild Moderate Severe Very severe
Induration (thickness)
Desquamation
Area
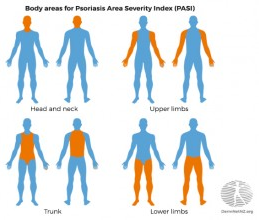
The percentage area affected by psoriasis is evaluated in the four regions of the body. In each region, the area is expressed as –
The percentage area affected by psoriasis is evaluated in the four regions of the body. In each region, the area is expressed as –
| Area involved | Grade of severity |
| Nil | (0), |
| 1-9% | (1), |
| 10-29% | (2), |
| 30-49% | (3), |
| 50-69% | (4), |
| 70-89% | (5) |
| 90-100% | (6). |
- Head and neck
- Upper limbs
- Trunk
- Lower limbs
Calculations for area
Each of the body area scores is multiplied by the area affected.
Each of the body area scores is multiplied by the area affected.
- B1 x (0 to 6) = C1
- B2 x (0 to 6) = C2
- B3 x (0 to 6) = C3
- B4 x (0 to 6) = C4
Other assessments
The Cardiff Dermatology Life Quality Index is a simple 10-question validated questionnaire to assess the impact of a skin disease on the patient's life. The same team have devised a specific assessment for the quality of life in psoriasis, the Psoriasis Disability Index.
The Cardiff Dermatology Life Quality Index is a simple 10-question validated questionnaire to assess the impact of a skin disease on the patient's life. The same team have devised a specific assessment for the quality of life in psoriasis, the Psoriasis Disability Index.
Based on these index patients were classified as-
Mild: Involved body surface area (BSA) < 10
Psoriasis Area severity index (PASI) < 10
Dermatology life quality index (DLQI) < 10
Moderate to
Severe: Involved body surface area (BSA) > 10
Psoriasis area severity index (PASI) > 10
Dermatology life quality index (DLQI) > 10
Mild: Involved body surface area (BSA) < 10
Psoriasis Area severity index (PASI) < 10
Dermatology life quality index (DLQI) < 10
Moderate to
Severe: Involved body surface area (BSA) > 10
Psoriasis area severity index (PASI) > 10
Dermatology life quality index (DLQI) > 10
In addition this can be categorised as -
Grades of severity Characteristics
Mild: Few scaly patch with itch
Moderate: Wide spread scaly lesion and associated
Bleeding on pulling scales.
Severe Wide spread silvery patch or scales with
generalised itch, swelling and agonising
Pain in joints.
Grades of severity Characteristics
Mild: Few scaly patch with itch
Moderate: Wide spread scaly lesion and associated
Bleeding on pulling scales.
Severe Wide spread silvery patch or scales with
generalised itch, swelling and agonising
Pain in joints.
After complete interrogation and clinical grading as per severity each patients were advocated the esteemed immune booster- Self-blood 2 ml with Betamethasone 1 ml (in non-diabetic cases as per following schedule in patients as adjuvant in tapering dose schedule and other continuing drugs are withdrawn.
Schedule of therapy
Every 4th day, week, 10th day, 15th day, monthly, 2 month, 3 months and 6 months for 10 injections each on competition of therapy therapeutic outcome is assessed as per following index of assessment.
Every 4th day, week, 10th day, 15th day, monthly, 2 month, 3 months and 6 months for 10 injections each on competition of therapy therapeutic outcome is assessed as per following index of assessment.
Clinical grades Characteristics
Grade I complete alleviation of clinical presentation without any residue, withdrawal or adjuvant or adversity
Grade II Marked relief in clinical presentation but recurrence on treatment withdrawal
Grade III No response of therapy except transient relief.
Grade I complete alleviation of clinical presentation without any residue, withdrawal or adjuvant or adversity
Grade II Marked relief in clinical presentation but recurrence on treatment withdrawal
Grade III No response of therapy except transient relief.
Observation
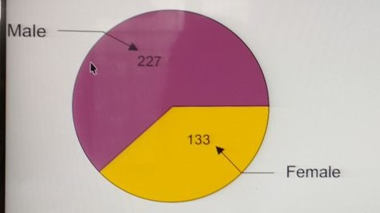
Selected patients were of age group 20-60 years and majority 186 were of age group 50-60 yrs. (T-1), Out of all 264 were male and 155 were female (Pie diagram)
Selected patients were of age group 20-60 years and majority 186 were of age group 50-60 yrs. (T-1), Out of all 264 were male and 155 were female (Pie diagram)
| Age group | Number of patients | |||
| (In yrs.) | Male | Female | Total | |
| 30-40 | 50 | 28 | 78 | |
| 40-50 | 94 | 48 | 142 | |
| 50-60 | 110 | 76 | 186 | |
| Total | 264 | 155 | 419 | |
Table 1: Distribution of patients as per age and sex.
As per distribution of lesion 164 were having lesion on extremity while 56 were having wide spread lesion and 90 presented with psoriasis sequel (Table 2)
| Area of distribution | Number of patients |
| Localised: | 273 |
| Face | 039 |
| Extremity | 164 |
| Abdomen | 070 |
| Wide spread | 056 |
| Sequel: | |
| Psoriatic arthritis | 090 |
Table 2: Distribution of patients as per distribution of lesion.
252 patients were suffering from 5-10 yrs. though 11 cases were suffering since more than 20 yrs. (Table 3)
|
Duration of illness (In years) |
Number of Patients | ||
| Male | Female | Total | |
| < 5 | 15 | 10 | 25 |
| 5-10 | 152 | 100 | 252 |
| 10-15 | 40 | 17 | 57 |
| 15-20 | 50 | 24 | 74 |
| > 20 | 07 | 04 | 11 |
Table 3: Distribution of patients as per duration of illness.
Out of all selected cases 50 cases have not taken any treatment while 57 cases have tried all sorts of medication (Table 4)
| Medication consumed | Number of patients | ||
| Male | Female | Total | |
| No treatment | 51 | 39 | 90 |
| Modern medication | 70 | 68 | 138 |
| Ayurvedic | 96 | 24 | 120 |
| Homeopath | 40 | 24 | 64 |
| All types | 32 | 26 | 57 |
Table 4: Distribution of patients as per therapeutic consumed.
Out of all 383 cases were qualified and middle upper class people (Table 5)
| Particulars | Number of patients | ||
| Male | Female | Total | |
| Qualified and middle-upper class | 237 | 146 | 383 |
| Illiterate & down trodden | 27 | 09 | 36 |
Table 5: Distribution of patients as per social and educational status.
Out of all 1.5% male and 4.5% female show altered hepatic function, 39.2% male and 24.6% female present with albuminuria, 37.1% male and 38.7% female are anaemic with Haemoglobin < 10gma%, 2.27% male and 4.5% female were hyperglycaemic (Table 6)
| Basic Profile | Number of patients | ||
| Male | Female | Total | |
| Hepatic Profile: | |||
| SGOT: | |||
| < 35 | 260 | 148 | 408 |
| > 35 | 04 | 07 | 11 |
| SGPT | |||
| < 35 | 260 | 148 | 408 |
| > 35 | 04 | 07 | 11 |
| Renal profile: | |||
| Blood urea: | |||
| < 26 | 264 | 155 | 419 |
| > 26 | None | None | None |
| Serum creatinine | |||
| < 1.5 | 264 | 155 | 419 |
| > 1.5 | none | none | none |
| Urine Albumin | |||
| Present | 104 | 65 | 169 |
| Absent | 160 | 90 | 250 |
| Hematology: | |||
| Hemoglobin (gm%) | |||
| < 10gm% | 98 | 60 | 158 |
| > 10gm% | 166 | 95 | 261 |
| Absolute eosinophil: | |||
| < 400/cc | 264 | 155 | 419 |
| > 400/cc | none | none | none |
| Blood Sugar | |||
| Fasting | |||
| < 100 mg% | 258 | 148 | 406 |
| > 100mg% | 06 | 07 | 13 |
Table 6: Shows basic bio status.
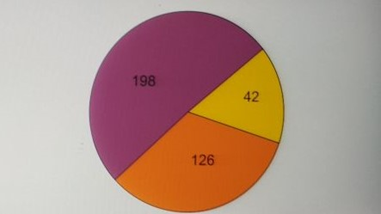
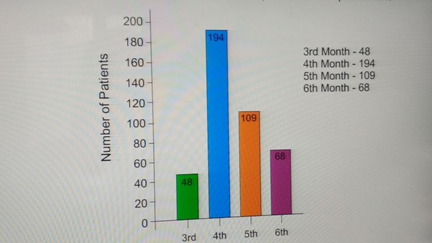
Out of all 10 % (42) were of mild grade while 34.9% (146) were of grade III severity (Bar diagram) Majority 46.3% (194) cases have taken 4 months to begin improvement in agonizing presentation whereas 48 cases shown improvement on 3 months completion of therapeutic regime and 68 case taken 6 months’ time (Bar diagram)
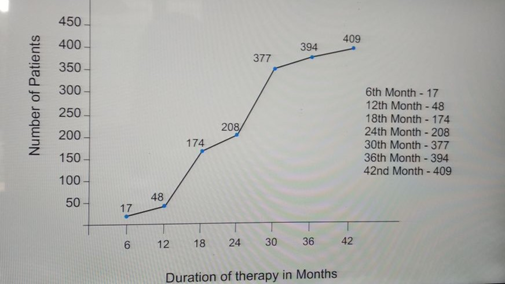
Complete cessation of agonizing presentation achieved after 6 months therapy and by 3 yrs majority patients 94.5% (396) had complete relief of presenting features and agonising itch (Graph showing achievement of recovery)
Out of all 94% (396) patient had grade I clinical response while rest grade II without any relapse or withdrawal reflex or any adversity related to therapeutic regime nor any disease related sequel during the vigil follow up.
Pie diagram showing distribution of patients as per degree of severity:
Bar diagram showing time lapse for onset of improvement
Graph showing therapeutic response
| Characteristics Number of patients Grade of therapeutic response: I 396 II 23 III Non Any untoward effects Non Bio status: Altered Non Drug related adversity Non |
Table 7: Showing outcome of therapy.
Result
94% patients of psoriasis of varied degree of severity had complete cessation of agonizing presentation in 3 years without any supplementation, drug adversity, therapy withdrawal sequel.
Discussion
Psoriasis, a result of abnormal excessive and rapid growth of epidermis layer of skin and premature maturation of keratinocyte inducing dermal inflammatory cascade involving dendritic cell, macrophages and T cells which move from the dermis to epidermis and secrete inflammatory chemical signals (Cytokine) i.e.- interleukin 36¥, tumour necrosis factor -α, interleukin and interleukin 6 and 22. [21-24]
DNA released from dying cells acts as an inflammatory stimulus and stimulate dendritic cell. The present study showing complete relief of presentation and non-had any recurrence, relapse or any drug or disease related untoward effects suggest immunological improvement by self-blood due to generation of specific antibody which binds with specific protein and check cell death rate, curb T cell, block Tumour necrosis factor (TNF-α) and stop release of chemical messenger and limit dendrite cell and favours Th2 cells Cytokine secretion pattern over a Th1/Th17cell cytokine profile Dendritic cell bridge the innate immune system and adaptive immune system . [25-32] Betamethasone calm the antigen and antibody reaction and alleviate the presentation.
References
- Kaur I., et al. “Epidemiology of psoriasis in a clinic from north India”. Indian Journal of Dermatology, Venereology and Leprology 52.4 (1986): 208-212.
- Bedi TR. “Psoriasis in north India. Geographical variations”. Dermatologica 155.5 (1977): 310-314.
- Christophers E. “Psoriasis-epidemiology and clinical spectrum”. Clinical and Experimental Dermatology 26.4 (2001):314-320.
- Lomholt G. “Prevalence of skin diseases in a population: a census study from the Faroe Islands”. Dan Med Bull 11 (1964): 1-7.
- Hellgren L. “Psoriasis: The prevalence in sex, age and occupational groups in total populations in Sweden. Morphology, inheritance and association with other skin and rheumatic diseases”. Stockholm: Almquist and Wiksell 1967
- Brandrup F and Green A. “The prevalence of psoriasis in Denmark”. Acta Dermato-Venereologica 61.4 (1981): 344-346.
- Farber EM and Nall L. “The Natural history of psoriasis in 5,600 patients”. Dermatologica 148.1 (1974): 1-18.
- Okhandiar RP and Banerjee BN. “Psoriasis in the tropics: An epidemiological survey”. Journal of the Indian Medical Association 41 (1963): 550-556.
- Bedi TR. “Clinical profile of psoriasis in North India”. Indian Journal of Dermatology, Venereology and Leprology 61.4 (1995): 202-205.
- Kaur I., et al. “Natural history of psoriasis: a study from the Indian subcontinent”. The Journal of Dermatology 24.4 (1997): 230-234.
- Amanda Oakley, PASI Score, Derm Net NZ /2009
- Global report on Psoriasis, WHO psoriasis 2016
- Moll JM and Wright V. “Psoriatic arthritis”. Seminars in Arthritis and Rheumatism 3.1 (1973): 55-78.
- Gladman DD, Rahman P. Psoriatic arthritis. In: Ruddy S, Harris ED, Sledge CB, editors. Kelly's textbook of Rheumatology. 6 th ed. Philadelphia W.B Saunders Company 2 (2001): 1071-1079.
- Rajendran CP., et al. “Psoriatic arthritis”. The Journal of the Association of Physicians of India 51 (2003): 1065-1068.
- Prasad PV., et al. “A clinical study of psoriatic arthropathy”. Indian Journal of Dermatology, Venereology and Leprology 73.3 (2007): 166-170.
- Ray SPC., et al. “Clinical profile of psoriatic arthropathy”. Indian Journal of Dermatology, Venereology and Leprology 56.3 (1990): 200-203.
- Shah NM., et al. “Psoriatic arthritis - a study of 102 patients”. Journal of Indian Rheumatology Association 3.4 (1995): 133-136.
- Nadkar MY., et al. “Clinical profile of psoriatic arthritis”. Journal of Indian Rheumatology Association 8 (2000): S40.
- Kononen M., et al. “An epidemiological survey of psoriasis in the Greater Helsiniki area”. Acta Dermato-Venereologica. Supplementum 124 (1986): 1-10.
- Kammer GM., et al. “Psoriatic arthritis: a clinical, immunologic and HLA study of 100 patients”. Seminars in Arthritis and Rheumatism 9.2 (1979): 75-97.
- Robert ME., et al. “Psoriatic arthritis - follow up study”. Annals of the Rheumatic Diseases 35.3 (1976): 206-219.
- Gisondi P., et al. “Prevalence of metabolic syndrome in patients with psoriasis: a hospital-based case-control study”. British Journal of Dermatology 157.1 (2007): 68-73.
- Takahashi H., et al. “Prevalence of metabolic syndrome in Japanese psoriasis patients”. Journal of Dermatological Science 57.2 (2010): 143-144.
- Wilczek A and Sticherling M. “Concomitant psoriasis and bullous pemphigoid: coincidence or pathogenic relationship?” International Journal of Dermatology 45.11 (2006): 1353-1357.
- Yasuda H., et al. “Two cases of subepidermal blistering disease with anti-p200 or 180-kD bullous pemphigoid antigen associated with psoriasis”. Dermatology 209.2 (2004): 149-155.
- Sandhu K., et al. “Psoriasis and vitiligo”. Journal of the American Academy of Dermatology 51.1 (2004): 149-150.
- de Arruda LH and De Moraes AP. “The impact of psoriasis on quality of life”. The British Journal of Dermatology 144 Suppl 58 (2001): 33-36.
- Ashcroft DM., et al. “Quality of life measures in psoriasis: a critical appraisal of their quality”. Journal of Clinical Pharmacy and Therapeutics 23.5 (1998): 391-398.
- Rakhesh SV., et al. “Quality of life in psoriasis: a study from south India”. Indian Journal of Dermatology, Venereology and Leprology 74.6 (2008): 600-606.
- Gaikwad R., et al. “Evaluation of functional impairment in psoriasis”. Indian Journal of Dermatology, Venereology and Leprology 72.1 (2006): 37-40.
- Matto SK., et al. “Psychiatric morbidity in vitiligo and psoriasis: A comparative study from India”. The Journal of Dermatology 28.8 (2001): 424-432.
Citation:
Avinash Shankar., et al. “Self-Blood (Immunotherapy), A New Hope for Psoriasis”. Medical Research and Clinical Case Reports
1.1 (2018): 29-39.
Copyright: © 2018 Avinash Shankar., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.