Case Report
Volume 1 Issue 2 - 2018
HAEMATOCERVIX: Case Report and Review of Literature
1Specialist Registrar, Kings College Hospital, London
2Conultant Gynaecologist, Kings College Hospital, London
2Conultant Gynaecologist, Kings College Hospital, London
*Corresponding Author: Prashant Purohit, Specialist Registrar, Kings College Hospital, London. Email: prashant.purohit@nhs.net.
Received: March 02, 2018; Published: March 16, 2018
Keywords: Haematocervix; Hematometra; Haematotrachelos; CIN; LLETZ; Cervical stenosis
Introduction
Obstruction to the lower genital outflow track in normally menstruating women results in back pressure and accumulation of menstrual blood in the upper genital track. Cryptomenorrhea in these women presents as haematocolpos (blood accumulating in vagina) or haematometra (blood accumulating in uterus). Haematocervix (blood accumulating in cervical canal) is a rare condition caused by obstruction of the lower female genital tract at the level of the external cervical os resulting in accumulation of menstrual fluid in the uterine cervix. These conditions arising in younger patients are usually due to congenital genital tract abnormalities [1] whereas in older women, the obstruction is usually acquired, commonly after cervical surgery or trauma. [2]
A literature search was carried out in Pubmed, Google Scholar and Medline using the keywords Hematotrachelos, haematocervix, haematometra, LLETZ and Cervical stenosis. A total of 16 cases were identified. We present an interesting case who presented in A & E with late onset haematocervix 3 years after her repeat LLETZ procedure.
Case Report
We report a case of a , 51 year old lady who presented to the Accident and Emergency Department with a two day history of feeling unwell, vomiting and lower abdominal pain radiating down both legs and to the back. She previously had five spontaneous term vaginal deliveries and was using Depo Provera injections for contraception. She discontinued this 12 months prior to her presentation and had not experienced any menstrual periods following discontinuation. Prior to that, she had regular periods. She gave a history of cervical intraepithelial neoplasia (CIN) for which she underwent three large loop excisions of the transformation zone procedures (LLETZ). The last of these was 3 years before this presentation. On presentation, she had marked supra pubic tenderness with no guarding or rigidity. No abdominal or pelvic masses where palpable. A speculum examination revealed a bulge in the vagina with no discernible external cervical os. Here initial bloods tests were unremarkable apart from a raised white blood cell (WBC) count (13.86x109/L). Her abdominal and chest X-rays were unremarkable.
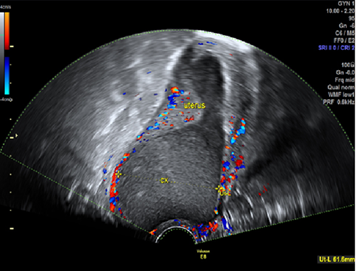
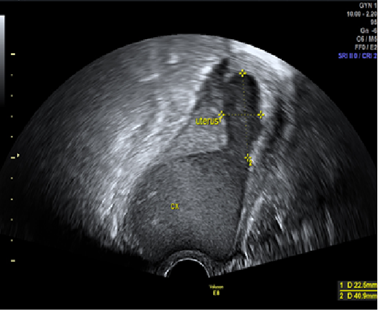
A transvaginal ultrasound scan showed a normal sized uterus with mild haematometra (22 x 40 mm). However, just under the uterine cavity and within the cervical canal, a 65 mm x 62 mm x 57 mm (volume 120 ml) homogeneous hypoechoic mass was seen. The internal os was dilated to approximately 20mm. Both ovaries and the pouch of Douglas appeared normal. Bimanual examination failed to locate the external os opening. . The patient underwent examination under anaesthesia, cervical dilatation, hysteroscopy to assess and drain the collected blood. The cervix was successfully dilated to Hegar number 10 dilator and the haematoma was drained. Hysteroscopy revealed a normal appearance of the endometrium. A copper IUCD was inserted in the uterine cavity at the end of the procedure and the woman was discharged home the following day with antibiotic cover. The patient subsequently had normal monthly periods without any abdominal discomfort and a follow up pelvic ultrasound scan after 12 weeks showed a normal appearance of the cervical canal and the IUCD was subsequently removed.
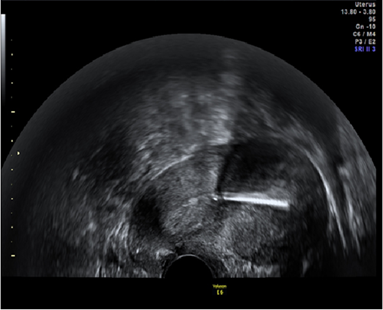
Figure 3: Post-operative 12 week Follow up pelvic ultrasound scan showing complete resolution of the haematocervix and haematometra. Cooper IUCD noted in the uterine cavity.
Discussion
Haematocervix is a rare and potentially troublesome clinical problem that usually follows surgical treatment for CIN, cervical trauma or laceration, following dilation and curettage, cervical or endometrial carcinoma and from radiation therapy. It has also been reported to occur due to presence of congenital lower genital tract anomalies. [1,3] In UK, the 2014-15 NHS cervical screening programme reported an incidence of 25.8% for CIN 2 and 46.1% for CIN 3 amongst the non-diagnostic biopsies taken at colposcopy and the standard treatment for these abnormalities is now is large loop excision of the transformation zone (LLETZ ) [4]. The commonest site of obstruction in such cases is in the lower genital tract in the region of the external cervical os resulting in accumulation of the menstruating blood in the uterine cavity. In addition to this , rarely as in our case there might be some further degree of stenosis at the level of the internal os leading to accumulation of the majority of the menstrual blood in the cervical canal with only a smaller amount of blood noted in the uterine cavity.
Very few cases of haematocervix have been described as compared to haematometra. We reviewed the published literature to identify cases. A search was carried out on PubMed, Medline and Google Scholar to identify cases using keywords like haemaotmetra/cervical stenosis/haematocervix/haematotrachelos/genital tract obstruction. We identified a total of 16 cases.
Most of the cases reported are following cervical conisation and cautery. [5-8 ] Pschera., et al. described a case of a 30 year old women with progressive haematocervix following cold knife biopsy of cervix done for CIN3. [9] The women presented with amenorrhea 3.5 months after the procedure and an ultrasound confirmed the diagnosis of haematocervix with the cervix measuring 80x80x80 mms. This was treated with incision over the external os and insertion of copper IUCD. [9] In our case, the lag period between the cervical trauma and presentation was four years. A similar case was describe by Sherer 2009 where the women presented with spontaneous haematocervix 5 years after cryosurgery for cervical dysplasia. [7] Apart from our case, there is only one report of haematorachelos reported following LLETZ procedure by Perino., et al. [2]
Another case of haematocervix was reported by Sherer., et al. presented as acute urinary retention, occurred following surgical repair of a cervical laceration during labour. This case was treated with abdominal hysterectomy. [10]
Any length of amenorrhoea after conservative lower genital tract surgery needs investigated. Appropriate counselling of the patients is necessary regarding complications and symptoms associated with it. The pressure building up inside the uterine cavity in turn causes chronic pelvic pain and compression effects like urinary retention due to increase in uterine size. In our case, the patient presented with acute lower abdominal pain radiating to back and both legs which can be attributed to distension of uterine cervix and compression on pelvic nerves causing referred pain. Some degree of endometriosis also contributed to her pain and raised white cell count.
One of the reason for delayed diagnosis in our case was that her amenorrhoea was attributed to the fact that she was perimenopausal and using depot Provera injections .However, this rare condition of haematocervix needs to be considered in such cases who have risk factors for developing this condition. Pansini., et al. described a case of haematocervix in a menopausal lady on cyclical HRT treated conservatively by dilatation of the atrophic external os. [11] Sauer., et al. reported a case of spontaneous haematocervix in a 66 year old asymptomatic women with no previous cervical surgery who later was diagnosed to have adenocarcinoma of the endometrium. [12] Lin Y-h also described a case of spontaneous haematocervix in a perimenoupausal women. [13] Sherer., et al. has also described a case a spontaneous haematocervix in 17 year old girl with dysfunctional uterine bleeding. [14]
Management options differ depending on the cause and patients desire to conserve the uterus. In a case reported by Perino., et al. haematocervix resulting from loop biopsy was treated using manual vacuum aspiration and cervical catheter. [2]
A case of haematotrachelos was also described following a routine dilatation and curettage procedure was treated by dilatation and curettage and use of nasopharyngeal airway as a temporary stent. [15]
Haematocervix can also present very late after the initial insult. Tannus., et al. reported a case of haematocervix in a 67 year old women 15 years following a cervical cautry. [16] However, in this particular case, her post-menopausal status might have also contributed to the development of haematocervix.
Two cases of haematocervix reported by Clark., et al. had hysterectomy as the 1st line of manangement. [6] In our case, we successfully were able to dilate the cervix and get access into the cervical canal using Hegar dilators and a hysteroscopy was subsequently carried out and endometrial biopsy was obtained. Re-stenosis of the cervical os and re-occurrence of symptoms is common and frustrating for the patient and the clinician. Keeping this in mind we left an intrauterine copper IUCD which was removed after 12 weeks. At the follow-up, she remains asymptomatic with average menstrual flow and her transvaginal pelvic ultrasound showed a normal appearance of the endometrial cavity and cervical canal.
Management of this rare condition can be challenging and raising awareness of this is important to allow appropriate assessment and management of such cases
References
- Sherer DM and Beyth Y. “Ultrasonographic diagnosis and assisted surgical management of hematotrachelos and hematometra due to cervical atresia with associated vaginal agenesis”. Journal of Ultrasound in Medicine8.6(1989): 321-323.
- Perino., et al. “Management of Hematocervix After Loop Electrosurgical Excision Procedure.” Obstetrics & Gynecology 118. 2 Part 2 (2011): 484-486.
- E H Ritchie and JP MacCarron. “Primary dysmenorrhoea due to unilateral haematotrachelos.” Irish Journal of Medical Science 142.1 (1973): 323-328.
- Cervical Screening Programme, England: Statistics for 2014-2015.
- Konstantoulas M. “Ultrasonic diagnosis of haematocervix following cone biopsy of the cervix”. The British Journal of Radiology 51.601 (1978): 56-57.
- Clark A., et al. “Haematocervix following cone biopsy of the cervix”. Journal of Obstetrics and Gynaecology of the British Commonwealth 80.9 (1973): 858-861.
- David M Sherer., et al. “Acute Spontaneous Hematotrachelos Following Methotrexate Treatment of a Suspected Tubal Pregnancy.” Journal of Ultrasound in Medicine 25.8 (2006): 1091-1093.
- Tannus S and Atlas I. “Endometrial cancer presenting as acute urinary retention: a case report and review of the literature”. Cases Journal 2 (2009): 9382.
- Pschera H1 and Kjaeldgaard A. “Haematocervix after conization diagnosed by ultrasonography”. Gynecologic and Obstetric Investigation 29.4 (1990): 309-310.
- David M Sherer., et al. “Transvaginal Sonography of Hematotrachelos and Hematometra Causing Acute Urinary Retention after Previous Repair of Intrapartum Cervical Lacerations.” Journal of Ultrasound in Medicine 25.2 (2006): 269-271.
- F Pansini., et al. “Haematocervix during hormonal replacement therapy.” European Journal of Obstetrics & Gynecology and Reproductive Biology 51.2 (1993): 167-169.
- Sauer CM and Israel GM. “Edometrial Adenocarcinoma presenting as a Hematotrachelos.” The American College of Obstetrician and Gynaecologists 124.2 Part 2, (2014): 448-451.
- Lin YH., et al. “Perimenopausal amenorrhea with cervical atresia and hematotrachelos.” Journal of Medical Sciences 30.4 (2010): 173-176.
- Sherer D., et al “Acquired haematometra and haematotrachelos in a Adolescent with Dusfunctional uterine Bleeding.” JUM 25.12 (2006): 1599-1602.
- Witt BR. Treatment of hematotrachelos after dilatation and curettage: a case report. The Journal of Reproductive Medicine 44.1 (1999): 68-70.
- Samer Tannus and Ilan Atlas. “Endometrial Cancer Presenting as Acute Urinary Retention: a Case Report and Review of the Literature.” Cases Journal 2 (2009): 9382.
Citation:
Prashant Purohit., et al. “HAEMATOCERVIX: Case Report and Review of Literature”. Medical Research and Clinical Case Reports
1.2 (2018): 53-57.
Copyright: © 2018 Prashant Purohit., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.