Case Report
Volume 2 Issue 2 - 2018
Transtentorial Herniation: Wartenberg Reflex
1MD, Department of Clinical Neurophysiology, Neurology, Dokuz Eylül University Faculty of Medicine, İzmir, Turkey
2Associate professor, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Department of Neurology, University of Health Sciences, Ankara, Turkey
2Associate professor, Dışkapı Yıldırım Beyazıt Training and Research Hospital, Department of Neurology, University of Health Sciences, Ankara, Turkey
*Corresponding Author: Dilara Mermi Dibek, MD, Department of Clinical Neurophysiology, Neurology, Dokuz Eylül University Faculty
of Medicine, İzmir, Turkey.
Received: July 06, 2018; Published: July 17, 2018
The corneomandibular reflex, also known as Wartenberg reflex, is contralateral deviation of the jaw when the cornea is stroked with a cotton wisp. This clinical sign is extremely rare, and the pathophysiological basis is unclear. It is probably result of provoking the relationship between the orbicularis oculi and the lateral pterygoid muscle after supranuclear lesion of the trigeminal nerve [1]. The ophthalmic part of the trigeminal nerve form the reflex afferent fibers, which is triggered by the stimulation of conjunctiva and light touch receptors in the cornea. The fibers from the ophthalmic branch of the trigeminal nerve reach the trigeminal ganglion through superior orbital fissure, and then to main sensory nucleus of the trigeminal nerve [2].
The efferent fibers reach the facial nerve motor nucleus with the intraneurons and as a reflex it provides the eyelid closure. The inhibitory neurons, located near ipsilateral trigeminal nerve motor nucleus in mesencephalic trigeminal nucleus, inhibits massive trigeminal motor neuronal activity. In the presence of a cortico-pontin lesion, or less likely lesions in the brainstem, this inhibitory effect is lost, resulting the activation of the entire trigeminal motor nucleus by corneal stimulation, leading masseter contraction, thus cornea mandibular reflex [3-5]. According to Wartenberg, there is no more valuable test showing the supranuclear lesion of the trigeminal nerve [6]. Presence of the reflex shows the brain stem lesion and supratentorial event; transtentorial herniation is also an indicator. The reflex may also occur in the acute coma state, especially if the coma is related to the structural lesion, and may also be seen in elevated intracranial pressure , brain stem pressure secondary to large cerebral hemispheric lesion, intrinsic lesion of upper brain stem or diencephalon and involvement of the corticobulbar pathways in multiple sclerosis or amyotrophic lateral sclerosis [1,8].
A reflex develops in the contralateral side of the lesion by the unilateral lesion of the brain stem pressure. The reflex may occur bilaterally in most of the cases also it may occur more on one side and reflexes may occur temporarily [8].
CASE
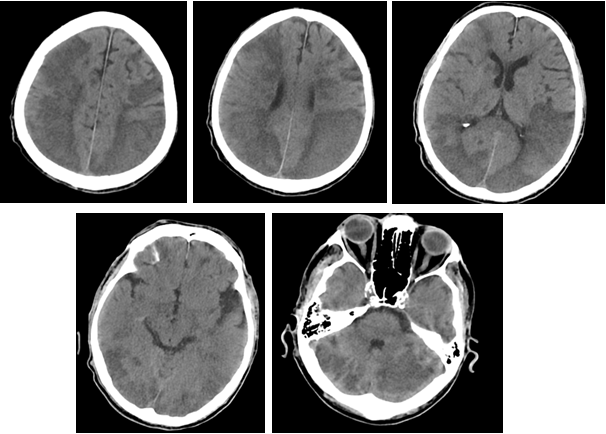
A 63-year-old male patient was consulted to neurology because of unable to regain consciousness postoperatively following an open heart surgery operation. The patient was not taking a sedative agent, general condition was poor and was on mechanical ventilatation. He was stuporous, grimacing to painful stimuli, isocoric pupils with slight reaction to light, oculocephalic reflexes were bilaterally present, corneal reflexes observed bilaterally, jerky movement was noted during the stimulation of the cornea. This observation is evaluated as bilateral corneamandibular reflex (video 1). The extremities did not respond to painful stimulus, plantar reflexes were bilateral extensor; bilateral hemispheric and cerebellar hypodense areas were seen in the brain computerized tomography of the patient, these were evaluated as subacute infarction (Figure 1). The patient died on the 5th day of the surgery.
It was thought that bilateral cornea-mandibular reflex in the patient developed due to transtentorial herniation caused by extensive hemispheric involvement. The disappearance of the corneamandibular reflex and the light reflex in the next day, supported the diagnosis.
References
- Guberman A. “Clinical significance of the corneomandibular reflex”. Archives of neurology 39.9 (1982): 578-580.
- Hinrichsen CF and Larramendi LM. “The trigeminal mesencephalic nucleus. II.electron microscopy”. American journal of anatomy 127.3 (1970): 303-319.
- Valls- Solé J. “Neurophysiological assessment of trigeminal nerve reflexes in disorders od central and peripheral nervous system”. Clinical Neurophysiology 116.10 (2005): 2255-2265.
- Ren K and Dubner R. “The role of trigeminal interpolaris-caudalis transition zone in persistent orofacial pain”. International Review of Neurobiology 97 (2011): 207-225.
- Aramedih M and Ongerboer de Visser BW. “Brainstem reflexes: Electrodiagnostic techniques, physiology, normotive data, and clinical application”. Muscle Nerve 26.1 (2002): 14-30.
- Wartenberg R. Diagnostic tests in neurology a selection for office use Chicago, Year books Publishers (1953): 228.
- Gordon RM and Bender MB. “The Corneamandibular reflex”. Journal of Neurology, Neurosurgery, and Psychiatry 34 (1971): 236-242.
- Schott JM and Rossor MN. “The grasp and other primitive reflexes”. Journal of Neurology, Neurosurgery, and Psychiatry 74.5 (2003): 558-560.
Citation:
Dilara Mermi Dibek and Mehmet Fevzi Öztekin. “Transtentorial Herniation: Wartenberg Reflex”. Medical Research and Clinical
Case Reports 2.2 (2018): 161-163.
Copyright: © 2018 Dilara Mermi Dibek and Mehmet Fevzi Öztekin. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.