Case Report
Volume 2 Issue 2 - 2018
An Unprovoked Case of Pityriasis Rosea: A Unique Report
1Neonatal and Children’s Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran
2North Khorasan University of Medical Sciences, Bojnurd, Iran
2North Khorasan University of Medical Sciences, Bojnurd, Iran
*Corresponding Author: Seyyed-Mohsen Hosseininejad, Neonatal and Children’s Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran. E-mail: hosseininejad.s.mohsen@gmail.com
Received: July 26, 2018; Published: August 11, 2018
Abstract
Pityriasis rosea is an itchy skin condition which frequently appears at the ages of 10 to 35 year-old. We report an Iranian case suffering from pityriasis rosea, whose etiology was questionable and differed from reported cases in terms of lesion distributial pattern and evident etiology; we declare that our case is new to the literature. The patient was successfully treated with a combination of oral cetirizine, a topical cream.
Key word: Pityriasis rosea; Etiology; Iran
Introduction
Pityriasis rosea is an itchy papulosquamous skin condition which arises in people usually between the ages of ten to thirty-five years old. Typically, it starts with a single “herald patch” lesion, followed by the onset of secondary encrusted, pink skin eruptions within two weeks. Though its etiology and nature is still unclear, immunologic reactions are usually blamed. Pityriasis rosea may impose significant discomfort and cosmotic challenges in affected cases. If a pregnant women develops pityriasis rosea, it may result in some serious consequences in her neonates, such as stillbirth, low gestational weight and premature delivery [1-3]. Reports have disclosed the incidence of pityriasis rosea is about 0.5–2% [2] there presentation varies but usually are the same in general [4-6].
But here, we introduce a 27-year-old male patient with pityriasis rosea who is unique in terms of skin lesion distribution and associated symptoms with interesting clean etiology and risk factors as well.
Case Presentation
A 27-year-old Iranian healthy man presented with a chif complaint of trunk itchy rashes for 5 days. The rashes started while he had no illness and no other prodromal symptoms. Below the neck and his anterior and posterior trunk were just involved. Though, there were no eruptions on his lims or buttocks; the palm and sole were not affected neither.
Physical examination exposed a herald patch on his trunk near to the neck with an approximate size of 0.5.1.5-cm oval to circular, thin plaque with encrusted erythema (Figure 1 and 2). There were secondary multiple oval lesions with a peripheral collaret scale which were erythematosquamous too; Laboratory analysis showed that his total count blood cells was normal, with a normal erythrocyte sedimentation rate of 11 mm/h (normal range: 0–15 mm/h); C-reactive protein level was 15.3 mg/L (normal range: 0-3 mg/L), and his anti-nuclear antibody and anti-neutrophil cytoplasmic antibodies were negative. Syphilis and human immunodeficiency virus (HIV) serological tests for him were negative, and microscopic examination for fungal infection was also negative. His past medical history was unremarkable. He had no history of allergy to any food or drugs.

Figure 1 and 2: Papulpsquamous skin lesions on the anterior
and posterior and below the neck besides herald patches.
He was not smoker nor alcohol abuser. Her social condition in terms of high risk sexual contacts and Intravenous injection or custody incarceration was negative and safe. He did not take any medication nor vaccination within last 6 months. The family history was negative for any rashes and none of his family members had the same skin lesions like him.
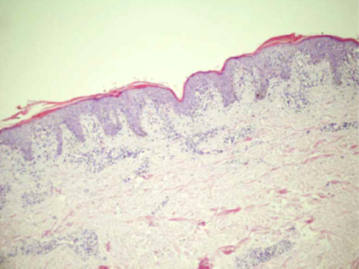
In histopathological skin biopsy, slight hyperkeratosis and a granular cell layer, which was reduced, was noticed in borders of patchs. Superficial dermis biopsy showed a mild intercellular edema (Figure 3). The biopsy of the epidermis revealed minor par keratosis, hyperkeratosis and a slight intercellular edema, besides few lymphocytes infiltration. There was a mild infiltration of perivascular lymphocytes and extravascular erythrocytes in the superficial dermis (Figure 4).
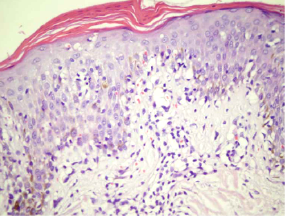
Figure 4: Par keratosis, hyperkeratosis and a slight intercellular edema,
besides lymphocytes infiltration and mild infiltration of perivascular
lymphocytes and extravascular erythrocytes in the superficial dermis.
Considering all the clinical and histopathological features, the diagnosis of pityriasis rosea was stabilized; he was treated with oral antihistamine to releive his allergic symptoms, like pruritus and a topical steroid cream. His symptomatic itch was slowly releived, and the lesions disappeared within 14 days. One month later, on follow up visit, he was fuly free of symptoms and skin lesion and no scar was remained.
Discussion
Pityriasis rosea is a clinical condition which at was termed in 1860 by Gibert. It is sudden-onset, self-limiting with pruritic papulosquamous skin lesion. The particular reason for occurring pityriasis rosea is not understood well, but lots of factors, including viruses, bacteria, fungi, and some no infective origins, could induce this condition. Latest evidence proposes that reactivation of HHV-6 may cause the development of the skin lesions, [7-9] and some drugs, like acyclovir, besides biological agents, [10,11] have been stated to be linked with developing pityriasis rosea. Some reports also settled pityriasis rosea post-vaccinatioally such as after receiving pneumococcal vaccine or human papillomavirus vaccination [10-12].
Interestingly, few reports about pityriasis rosea with no prodromal or associated symptoms and signs like fever, nausea and also oral ulcers maybe presented. One report revealed pityriasis rosea was accompanied with coryzal illness and fever [6] and the other one reported pityriasis rosea allied with oral ulcers [7].
Our patient had no allergy history to food and reported no records of receiving medicines (tablets, capsules or injections), and his serum analysis was negative for antibodies to syphilis or HIV, and a microscopic analysis showed negative result for fungal involvement. He had no history of receiving vaccination as well. Hence, it was challenging than what might have been contributed to the development of pityriasis rosea for him. So as described, Our patient differs from previous cases with pityriasis rosea or recurrent cases of that who was introduced in the literature [4-8] First, his rashes were linked with nothing evident or at lrast we coud not find a reliable source. We think that either a silent environmental stimulant of the immune system or an endogenous immune system alteration might have resulted in the skin eruptions. Second, his rashes were just located on his trunk and a part of his neck, as opposed to other reported pityriasis rosea cases whose rashes normally found on one’s extremities, limbs, trunk, abdomen and buttocks. As we know so far, a case report like what we introduced, has not been pronounced in the English language literature sources.
Conclusion
So, we have introduced a clinical case of pityriasis rosea which characterizes a rare report of pityriasis rosea so that its etiology was not clarified and none of the present data for the etiology was not positive for him. Maybe deeper and new investigations to find other origins and inducing factors for the condition “Pytriasis rosea” is need. We consider such a case is interesting and new to the literature. The patient was successfully cured with a combination of oral antihistamines, a topical steroid cream.
Statement
The authors declare that there is no conflict of interest. The informed consent was obtained from the patient.
The authors declare that there is no conflict of interest. The informed consent was obtained from the patient.
Acknowledgments
We are thankful for the cooperation from our patient.
We are thankful for the cooperation from our patient.
References
- ALoh TY and Cohen PR. “Ptityriasis rosea in pregnancy: report of a spousal occurrence and craniosynostosis in the healthy newborn”. Dermatology Practical & Conceptual 6.3 (2016): 39-46.
- AMahajan K., et al. “Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects”. Indian Journal of Dermatology 61.4 (2016): 375-384.
- ADrago F., et al. “Relapsing pityriasis rosea”. Dermatology 229.4 (2014): 316-318.
- AHalkier-Sørensen L. “Recurrent pityriasis rosea. New episodes every year for five years”. Acta Dermato-Venereologica 70.2 (1990): 179-180.
- Singh SK., et al. “Recurrent pityriasis rosea”. Indian journal of dermatology, venereology and leprology 64.5 (1998): 237.
- AZawar V and Kumar R. “Multiple recurrences of pityriasisrosea of Vidal: a novel presentation”. Clinical and Experimental Dermatology 34.5 (2009): e114-116.
- AChuah SY., et al. Recurrent and persistent pityriasisrosea: an atypical case presentation. Singapore medical journal 55.1 (2014): e4-6.
- ASankararaman S and Velayuthan S. Multiple recurrences in pityriasis rosea – a case report with review of the literature. Indian Journal of Dermatology 59.3 (2014): 316.
- ADrago F., et al. “Pityriasis rosea: an update with a critical appraisal of its possible herpesviral etiology”. Journal of the American Academy of Dermatology 61.2 (2009): 303-318.
- AMavarkar L. “Pityriasis rosea occurring during acyclovir therapy”. Indian journal of dermatology, venereology and leprology 73.3 (2007): 200-201.
- ADrago F., et al. “Pityriasis rosea following human papillomavirus vaccination”. Brazilian Journal of Infectious Diseases 19.2 (2015): 224-225.
- ASasmaz S., et al. “Pityriasis rosea-like eruption due to pneumococcal vaccine in a child with nephrotic syndrome”. The Journal of Dermatology 30.3 (2003): 245-247.
Citation:
Kourosh Kharkan Ghamsari and Seyyed-Mohsen Hosseininejad. “An Unprovoked Case of Pityriasis Rosea: A Unique Report”.
Medical Research and Clinical Case Reports 2.2 (2018): 197-200.
Copyright: © 2018 Kourosh Kharkan Ghamsari and Seyyed-Mohsen Hosseininejad. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.