Oral Health and Dentistry
ISSN: 2573-4989
Case Report
Volume 4 Issue 3
Telescopic Double Crown Overdenture: A Case Report
-
Department of Prosthodontics at the Centre of Dentistry, Oral Medicine, and Maxillofacil Surgery with Dental School, Tuebingen University Hospital
*Corresponding Author: Abdulaziz Alduwaisan, Department of Prosthodontics at the Centre of Dentistry, Oral Medicine, and Maxillofacial Surgery with Dental School, Tuebingen University Hospital, Osianderstr. 2-8, 72076, Tuebingen, Germany.
Abstract
Patients with insufficient restorative and prosthodontic treated teeth seek additional treatment to restore their appearance and regain confidence. In this case report, a 64- year-old female patient received overdentures for aesthetic and chewing improvement. The process is described starting from the diagnostic cast and discussion of treatment options to temporary bridges, preparation and trying in of crowns and casts, and final trying in of the telescopic dentures. The success of the procedure and the importance of regular follow-ups are discussed.
Introduction
Different treatment options exist for patients with numerous missing teeth, such as removable partial dentures (RPD). Telescopic dentures are types of prosthesis that are retained or attached by double crowns [1, 2]. The remaining teeth are thereby used to stabilize the prosthesis [3]. The aim of the present article was to report a clinical case in which telescopic dentures were fabricated and tried in on both jaws in order to improve aesthetics and mastication in a female patient without RPD.
Case Report
Assessment and Diagnosis
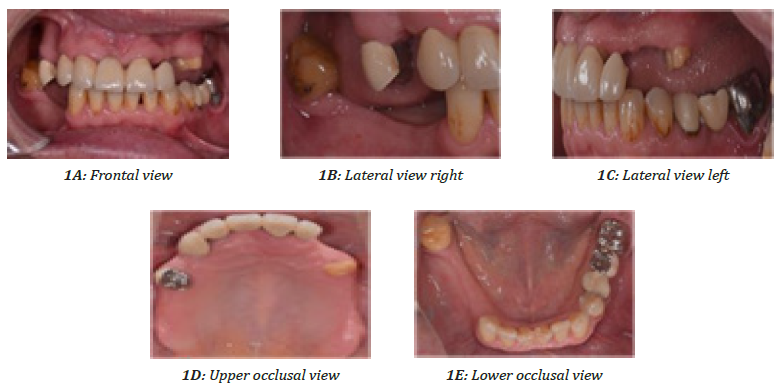
A 64-year old female retiree was referred to our departmental prosthodontic clinic after surgical treatment for further prosthodontics management and treatment. The patient wished for aesthetic and chewing improvement. The medical history included high blood pressure (hypertension), for which she reported taking 5 mg Ramipril daily. In terms of her dental history, the patient had multiple extracted teeth but had no RPD. She had restorations and old porcelain-fused-to-metal (PFM) bridges in the lower left 3 unit and the upper anterior 5 unit, and teeth number 37 and 24 were crowned and endodontically treated. The patient was motivated to receive the treatment. The extra- oral examination showed no muscle pain or temporomandibular joint pain upon palpation, and no temporomandibular joint noise was audible. Figure 1 shows different views of the intra-oral examination. The retromolar pad was well marked on both sides (Figure 1E) and the tuberosity well-defined. Oral hygiene was moderate. A cross bite of the right posterior teeth and multiple restorations were noted. An open margin crown had been placed on tooth number 37 due to caries (Figure 1C). In terms of migration, the midline shifted to the right, there was an unstable occlusion in the molar region, and tooth number 48 tilted mesial.The patient was diagnosed with insufficient restorative and prosthodontic-treated teeth and loss of the vertical dimension.
First Appointment
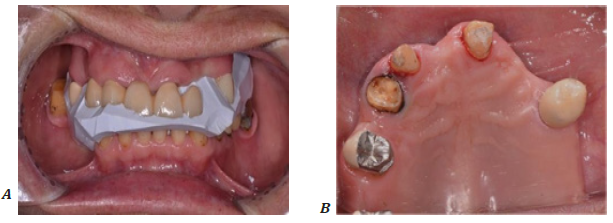
During the first appointment, the patient’s medical history and her chief complaint were assessed, and the extra- and intra-oral examinations were conducted. The treatment options were discussed with the patient and the selected treatment plan explained. System build-up as well as restoration for teeth number 13, 15, 33, and 34 was done with Ti-CoreTM (Essential Dental Systems, S. Hackensack, NJ, USA). A temporary bridge and crown were fabricated with temporization material (ProtempTM 4, 3M ESPE, Neuss, Germany). The upper and lower primary impressions were taken with alginate, and the primary jaw relation with silicon (SilaplastTM, DETAX, Ettlingen, Germany, Figure 2A). A diagnostic cast was generated to fabricate a thermoplastic vacuumed moulded template for a provisional bridge. The anterior bridge present in the upper jaw was removed (Figure 2B). Prefabricated unimetric post (11.5 mm length, Maillifer, Dentsply Sirona, Bensheim, Germany) was prepared for tooth number 24 and cemented with Flexi-FlowTM and then Ti-CoreTM (Essential Dental Systems, S. Hackensack, NJ, USA)
Second Appointment
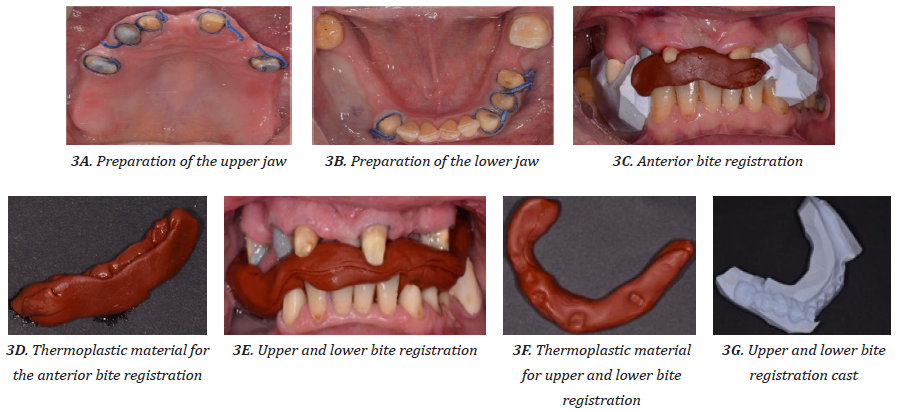
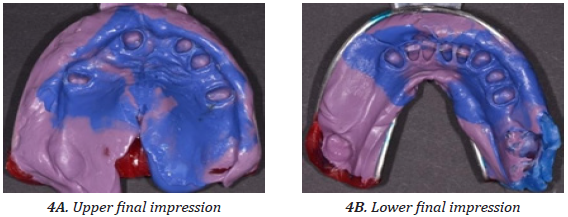
During the second appointment, the fine preparation was performed and bite registration using a thermoplastic material (Brown KerrTM, Kerr Dental, Brea, CA, USA) done. The anterior teeth were prepared first, followed by anterior bite registration (Figure 3A, 3C, 3D). After that, the posterior teeth number 15 and 24 were prepared, followed by the lower left side and tooth number 43 (Figure 3B). The anterior bridge was removed first and bite registered (Figure 3C), and then a bite registration was done for both the anterior and posterior teeth to maintain the vertical dimension (Figure 3E − 3G). The final impression was made with polyether impression material (ImpregumTM and PermadyneTM, 3M ESPE, Neuss, Germany, Figure 4). Figure 5 shows the temporary bridge in different views.
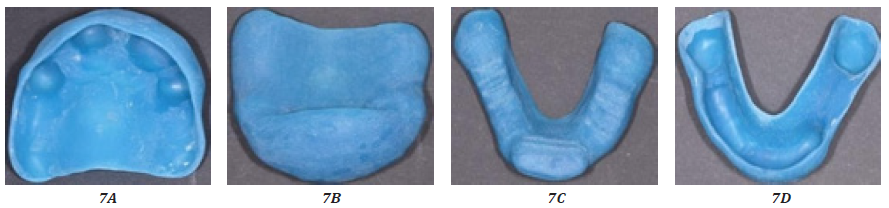
Third Appointment
The primary crowns were tried in (Figure 6 A and B) and their fitting checked (Figure 6C and 6D) during the third appointment. Fixation impressions with the primary crowns in the mouth were taken, using a polyether impression material (ImpregumTM and PermadyneTM, 3M ESPE, Neuss, Germany) (Figure 6E − 6H). The custom trays were also tried during this appointment (Figure 7).
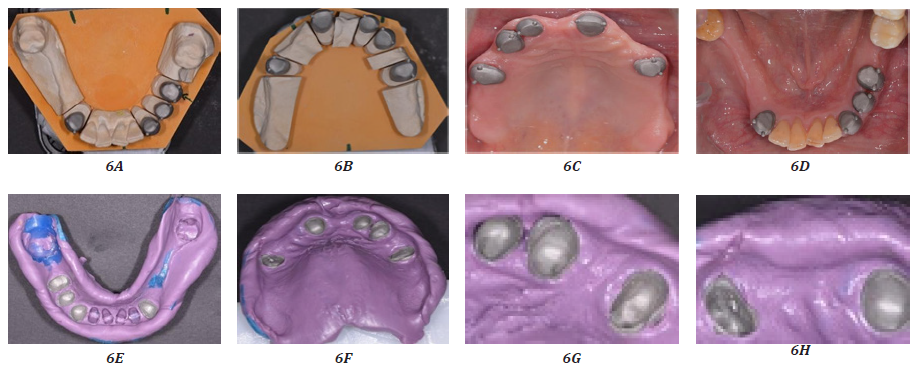
Figure 6: Trying in and fitting of the primary crowns
6A: Lower primary crowns, 6B: Upper primary crowns, 6C: Upper primary crowns tried in, 6D: Lower primary crowns tried in, 6E: Fixation impressions for the lower primary crowns, 6F – 6H: Fixation impressions for the upper primary crowns
Fourth Appointment
Only one procedure was carried out during the fourth appointment. The upper acrylic record block (Figure 8A and 8B) and the lower wax record block (Figure 8C and 8D) were tried in the patient’s mouth separately and together. The clinical information following the basic protocol for removable dentures for the orientation of the antero- superior occlusion rim in parallel with the bipupillary plane was recorded. The support of the lips was checked and the orientation of the postero-superior occlusion rim in parallel with the camper plane was carried out. Finally, the occlusal vertical dimension was oriented on the rest position and the centric relation bite registration for anterior teeth was done using FutarTM bite registration material (Kettenbach GmbH, Eschenburg, Germany) (Figure 8E). The face bow was recorded. The mid-line, close lip line, smile line, and canine lines were marked in the record block for the second wax try-in.
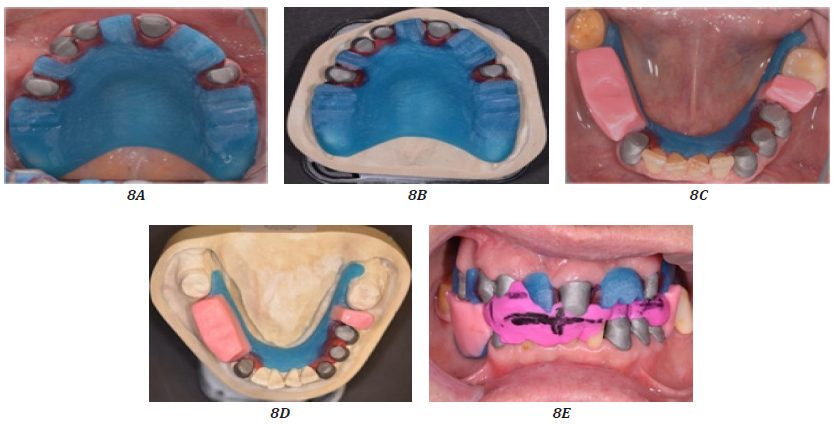
Figure 8: Trying in of the upper acrylic record block and the lower wax record block
A and B: Upper acrylic record block, C and D: Lower acrylic record block, E: Fixation impression
Fifth Appointment
Tooth number 37 was extracted. In the wax-up try-in appointment, the framework and wax-up telescope RPD for the upper (Figure 9A − 9C) and lower (Figure 9D – 9F) jaw were tried in separately and together. Figures 9G – 9I and 9J – 9L show the left and right framework and lateral view, respectively. The occlusion was adjusted, and aesthetic, phonetic, and smile lines were checked (Figures 9M – 9O). The patient’s opinion on the form and color of the teeth was taken, and a new bite registration was done with hard beauty pink wax (Integra Miltex Gmbh) in the front and posterior teeth (Figure 9P and 9Q).
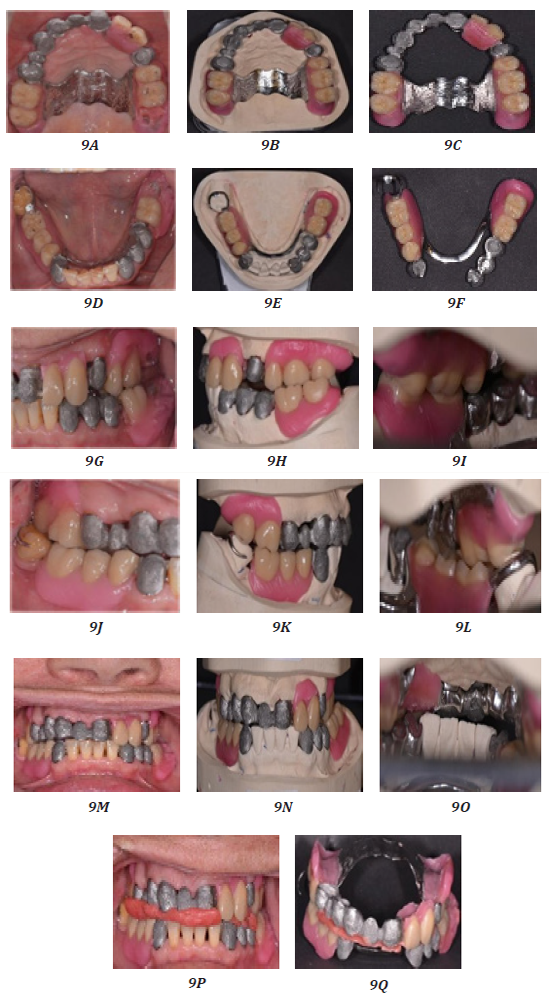
Figure 9: Wax-up trying-in
A – C: Upper framework and wax-up occlusal view, D – F: Lower framework and wax-up occlusal view,
G – H: Left framework and wax-up lateral view, J – L: Right framework and wax-up lateral view,
M – O: Frontal view framework and wax-up, P and Q: New bite registration
Final Appointment
During the final appointment, the finished prostheses were tried in and the fitting, occlusion and aesthetics were checked (Figure 10). The primary crowns in the upper and lower jaw were cemented with zinc phosphate cement (Harvard cement). Wearing the prostheses and taking them out were practised with the patient. The patient was provided with oral hygiene instructions, and a recall appointment date after one week was scheduled. The patient was requested to come for regular check-ups every 6 months.

Figure 10: Final fitting of the telescopic dentures
A – C: Upper telescopic denture occlusal, D – F: Lower telescopic denture occlusal,
G – I: Telescopic denture frontal view, J – L: Telescopic denture lateral view (left side),
M – O: Telescopic denture lateral view (right side)
The final results are shown in frontal view as before and after pictures in Figure 11.
Discussion
The present case report summarizes the aesthetic procedure of overdenture and crown fixtures in a patient diagnosed with insufficient restorative and prosthodontic treated teeth and a loss of vertical dimension. The patient suffered from her aesthetics before the treatment and sought treatment primarily to improve her appearance with dentures. With the improvement of the aesthetics and the restorage of the chewing ability and oral hygiene, the patient regained confidence in herself and her quality of life increased.
In a stepwise approach during multiple appointments, a diagnostic cast was prepared to identify treatment options, followed by fitting of a temporary bridge, preparation and fitting of the crowns, trying in of the crowns and the impressions, and finally fitting of the telescopic dentures. With this approach, the dentures provided an obvious improvement in the patient’s appearance (Figure 10).
In patients who have spent an extended period of time without teeth or prosthesis (in this case, about 7 years), the orthodontist faces difficulties with recording of the jaw relation. Therefore, more than one method of recording the relation should be used to find the right position in such cases. In the present case, the rest position, speaking distance and concept of thirds of face were used to establish the jaw relation. In particular, the bridge was sectioned in the lower left side at tooth number 35 and teeth were used as an abutment for a telescopic denture. A telescopic prosthesis was done, as this type of restoration offers better guidance, fixture and support compared to removable partial dentures. In addition, it offers the advantage of better aesthetics (e.g., no brackets, bone defects) and hygiene.
The telescopic denture success rate is higher than that of removable partial dentures [4]. For patients with free ends in the upper jaw, it is recommended to use a large connector (transverse band) for increased stability. In order to guarantee long-term success with telescopic prostheses, the patient should receive hygiene instructions and regular controls [5]. Follow-up care is of importance to maintain oral hygiene, ensure appropriate positioning and fixture of the dentures, and improve the long-term success of the dentures [5, 6].
In summary, the present case report demonstrates successful restauration of the oral appearance in a patient with insufficient prosthodontics and loss of vertical dimension. It corroborates the need for multiple recordings of the jaw relation to ensuring correct fitting and optimal aesthetics.
References
- Tushar Vitthalrao Bhagat and Ashwini Nareshchandra Walke. “Telescopic Partial Dentures-Concealed Technology”. Journal of International Oral Health 7.9 (2015): 143-147.
- Mohammad Ayham Hakkoum and Ghassan Wazir. “Telescopic Denture”. The Open Dentistry Journal 12 (2018): 246-254.
- Laxman Singh Kaira and Rakesh Mishra. “Telescopic denture a treatment modalitity of preventive prosthodontics”. International Journal of Oral Health Sciences 3.2 (2013): 121-124.
- C S Shruthi., et al. “Telescopic Overdenture: A Case Report”. International Journal of Biomedical Science 13.1 (2017):43-47.
- Wöstmann B., et al., “Long-term analysis of telescopic crown retained removable partial dentures: survival and need for maintenance”. Journal of Dentistry 35.12 (2007): 939-945.
- Bergman B., et al. “Long-term clinical results after treatment with conical crown-retained dentures”. The International Journal of Prosthodontics 9.6 (1996): 533-538.
Citation:
Abdulaziz Alduwaisan. “Telescopic Double Crown Overdenture: A Case Report”. Oral Health and Dentistry 4.3 (2020): 103-110.
Copyright: © 2020 Abdulaziz Alduwaisan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.