
Oral Health and Dentistry
ISSN: 2573-4989
Research Article
Volume 7 Issue 1
A Retrospective Clinical Evaluation of Direct and Indirect Aesthetic Restorations with Cuspal Replacement
-
1DDS, MSc - Federal University of Rio Grande do Sul
2DDS, MSc, PhD - Federal University of Rio Grande do Sul
*Corresponding Author: Carolina Berwanger, Rua Ramiro Barcelos,2492, Porto Alegre/RS, Brazil. Zip Code 90035-003.
Abstract
Introduction: The increasing demand for aesthetic restorations had enabled new treatment choices to restore posterior teeth with extensive cavities. The treatments of these teeth involve direct composite restoration or indirect onlays, made with ceramic or composite. However, clinical data on the longevity of cuspal restorations comparing direct and indirect techniques and the restorative materials are rare.
Purpose: To perform a retrospective clinical evaluation of direct restorations (composite resin) and indirect restorations (composite resin and ceramics) with cuspal involvement, using the FDI criteria.
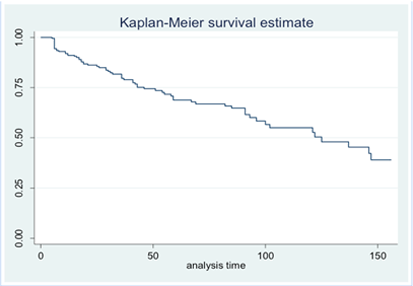
Materials and Methods: 229 restorations were evaluated in 121 patients (37 men and 84 women) who received at least one direct composite restoration with involvement of at least one cusp or ceramic/composite onlays among the years 2003 and 2016. The visual evaluation was done by an examiner previous calibrated by Cohen’s Kappa coefficient, using the FDI criteria. Data were analyzed by Kaplan-Meier, multivariated Cox regression analysis and Kruskal-Wallis test (p<0.05).
Results: Among the evaluated restorations, 69 failures were detected. The average evaluation time was 4.3 years. Restorations achieved a survival rate of 69.9%, with annual failure rate (AFR) of 8.0%. Direct composite restorations presented 34.1% of failure, with AFR of 9.6%. Composite onlays presented 27.3% of failure, with AFR of 7.1%. Ceramic onlays showed a 28.8% failure rate with AFR of 7.6%. Restorations in men have failed more than in women. The most common reason for failure was fracture of the material and retention, occurring in 48 cases (69.56% of the failures).
Conclusion: Direct and indirect restorations showed similar longevity, regardless of the number of cusps involved. Indirect restorations had lower annual failure rate than direct restorations, presenting better performance in the qualitative analysis. Female patients presented lower risk of failure, and the most prevalent type of failure in restorations with cusp involvement was fracture and retention.
Keywords: Dental restoration; survival rate; longevity; composite resins; ceramics
Introduction
The necessity of an alternative treatment to substitute amalgam restorations and the increasing demand for aesthetic restorations in the last decades has changed modern Dentistry. Esthetic and minimally invasive treatments, instead of traditional metallic materials, are the new trend to restore posterior teeth with extensive cavities [1]. The good performance of adhesive systems and the principles of conservative dentistry allow these teeth to be rehabilitated through the adhesive techniques, which present as advantages restorative material retention and bond strength without the need of tissue removal when preparing a tooth [2].
Posterior teeth that have lost a substantial amount of dental structure as a result of caries injuries, cavity preparation, fractures, detrition, endodontic treatments or any combination of these factors frequently represent a dilemma for dentists in relation to the best treatment strategy for these restorations. Fragile or structurally compromised cusps can be reduced and/or covered by restoration material in indirect restorations [1]. Restorations with cuspal coverage can increase fracture resistance of restored teeth that can be compared to the resistance of a sound tooth [2, 3].
The treatment of teeth with extensive cavities involve direct composite restoration [4, 5] or indirect onlays [1, 6], made with ceramic or composite resin [1, 3]. Direct composite resin restorations have been used on a large scale due to its low cost, small amount of sound dental tissue removal [7-10], positive physical, mechanical, adhesive, and aesthetical properties and the possibility of repair when necessary. Composite resins are currently the chosen material for posterior teeth conservative aesthetic restorations [11, 12], which present proven clinical longevity by several studies [9, 10, 13].
On the other hand, issues such as elevated C-Factor, polymerization srhinkage, the difficulties to reestablish proximal contacts and reproduce dental anatomy and the incomplete curing on the deepest parts of the cavity are some of the challenges regarding the extensive direct restorations built ups [5, 8].
Indirect restorations (onlays) aim to cover at least one dental cusps with a reduced cavity preparation [1, 5], when compared to a traditional crown. The use of the onlays has increased significantly due to the evolution of adhesive systems, luting cements and ceramics, that promotes efficient sealing, fracture strength and retention of the restorations [1, 2, 3].
To restore extensive cavities, the use of onlays presents some advantages when compares to the direct technique. Among these advantages, we can highlight its ease to achieve a satisfactory anatomic shape, better proximal contact getting, predictable occlusion parameters and polishing, with improved physical and mechanical properties of the material [3, 14]. Further, onlays keep the polymerization srhinkage restricted to the composite luting cement line [2, 14] and demonstrate a positive longterm clinical performance [14, 15], presenting a survival rate up to 92.4% in 12 years [6]. The development of etched ceramic systems, such as leucite and lithium disilicate, allow partial ceramic restorations adhesively cemented to recover tooth structure [1].
Nonetheless, onlay restorations also present a few disadvantages when compares to direct restorations, like a more invasive tooth removal and the complexity of luting process [16], as well as the greater cost to the patient due to laboratorial phase and number of dental appointments.
The importance of the knowledge about direct and indirect restorations with cuspal involvement is undeniable. The constant need for more clinical data regarding the performance and longevity of restorations with cuspal involvement is clear. Longitudinal clinical studies comparing direct and indirect restorations are rare. Also, composites and ceramic onlays comparison is still unclear [1, 16]. Ultimately, retrospective studies could evaluate the quality and longevity of the restorations with cuspal involvement, reflecting the clinical reality [11].
Thus, the purpose of the present study was to perform a retrospective clinical evaluation of direct restorations (composite resin) and indirect restorations (composite resin and ceramics) with cuspal involvement, using the FDI criteria.
Materials and Methods
Study Type and Ethical Considerations
The present research consists in a blind clinical retrospective study of direct composite resin restorations with cuspal involvement and indirect restorations (onlays) made of composite resin and ceramic. The study was performed in the school of Dentistry of the Federal University of Rio Grande do Sul (UFRGS) and was evaluated and approved by the Ethics Committee (protocol number 24358/1.202.537). All patients have signed a consent term before participating in the study.
Sample Calculation
The sample size needed for the study was calculated based on a 90% confidence interval, presumed error of 10% and an outcome of secondary caries of 22.4% [9]. The minimum value found for n was 47 patients.
Patient Selection
Patients were selected according to pre-determined inclusion criteria:
- Patients who were treated with composite resin or ceramic onlays.
- Patients who received posterior direct composite restorations with total cuspal involvement.
- Adult patients of both genders.
- Restorations with or without a liner of calcium hydroxide cement or glass ionomer cement.
- Restorations on vital or non-vital teeth.
A research was conducted among the patients’ records of the school of Dentistry of UFRGS. Patients who received at least one direct composite restoration with cuspal involvement or one composite or ceramic onlay between 2003 and 2016 were included in this study. Restorations should be at least for 06 months in service before evaluation.
Among 1500 patients’ records analysed, 135 patients were selected and invited to participate in the study by phone calls. 121 patients were included (37 men and 84 women), and 229 restorations were evaluated. Patients who agreed with the study terms signed written informed consent and were evaluated in the clinics of the school of Dentistry, by an examiner blind for the study objectives, calibrated by Cohen’s Kappa coefficient. All restorations were placed by a final year under graduation dental students of UFRGS.
Restorative Procedures
Patients selected had direct composite restorations built of ten different brands of composite resin. Indirect restorations were made of either composite Sinfony (Ceromer - 3M) or ceramic IPS Empress II/ e.max Press (Ivoclar Vivadent). Direct restorations were built by incremental technique and received finishing and polishing immediately. All restorations were placed using a total etch 3-step adhesive system Scotchbond Multipurpose (3M), and all indirect restorations were cemented with dual composite luting cement RelyXTM ARC (3M). Information about restorative materials can be checked on table 1.
| Resin | Manufacturer | Inorganic Particles Classification | E-module (GPa) | Percentage of Inorganic Particles | Average size of Particles | N Restorations |
| Charisma | Heraeus Kulzer | Micro hybrid | 14,06 | 59.4vl | 0.7μL | 17 |
| Z350 XT | 3m/ESPE | Nanoparticulate | 13.3 | 63.3vl | 20-75nm | 23 |
| Opallis | FGM | Nano hybrid | 9.1 | 58vl | 0.5 μm | 20 |
| Amelogen Plus | Ultradent | Micro hybrid | 7.6 | 76wt | 0.7 μm | 9 |
| Esthet –X HD | Dentsply | Nano hybrid | 12.3 | 77wt | 0.6-0.8 μm | 5 |
| Solitaire | Heraeus Kulzer | Highly Filled | 6.0 | 66wt | 2-20 μm | 3 |
| 4Seasons | Ivoclar Vivadent | Nano hybrid | 9.05 | 76wt | 0.6 μm | 2 |
| Amaris | VOCO | Fine Hybrid | - | 80wt | 0.6-1 μm | 1 |
| IPS Empress | Ivoclar Vivadent | Nano hybrid | 10.4 | 75-79wt | 0.6-1 μm | 1 |
| TPH3 | Dentsply | Hybrid | 9.6 | 74wt | 0.6-1 μm | 1 |
| Sinfony | 3M/ESPE | Micro hybrid | 12.3 | 45wt | 0.6-1 μm | 88 |
| Empress II/ e.max Press | Ivoclar Vivadent | Vitreous ceramic with lithium disilicate | 96 | 70vl | 3-6 μm | 59 |
Table 1: Characteristics and properties of restorative materials evaluated
Evaluation Procedures
Clinical evaluation was conducted with exploratory probe, mirror and odontologic light reflector, using the FDI criteria, including aesthetic, funcional and biological properties. When the restoration failed before clinical evaluation, date and reasons for failure were registered according to patient’s records or reports. Patients were asked about bruxism, if there was a habit of clenching or grinding their teeth, pain or muscular fatigue, teeth wearing or if they had a bruxism diagnosis before. All patients were subjected to an interproximal radiographic examination.
Data Evaluation
Data obtained from clinical evaluation of restorations were subjected to statistical analisys. Kaplan-Meier and Log-Rank tests were used to make a comparision among different restorations. Cox Regression was used to check independent variables and the risk of restorations’ failures and Kruskal-Wallis was used to compare the FDI criteria of the qualitative analysis. For all tests, the significance level was set at 5% (0.05). Annual failure rates were calculated for the three types of restorations.
Results
Distribution of restorations according to the independent variables is presented in table 2. Overall, 229 restorations were evaluated in 121 adult patients (mean age 50.7 years), with a survival rate of 69.9% (69 failures, annual failure rate (AFR) of 8.0%). The follow-up time ranged from 6 months to 13 years, with an average observation time of 4.3 years.
| Independent Variables | n | % | |
| Gender | Male | 37 | 16.1 |
| Female | 84 | 36.6 | |
| Total | 221 | 100 | |
| Tooth | Premolar | 67 | 29.2 |
| Molar | 162 | 70.7 | |
| Total | 229 | 100 | |
| Material | Direct Composite | 82 | 35.8 |
| Indirect Composite | 88 | 39.4 | |
| Ceramic | 59 | 25.7 | |
| Total | 229 | 100 | |
| Tooth Vitality | Vital | 161 | 70.3 |
| Non-Vital | 68 | 29.6 | |
| Total | 229 | 100 | |
| Bruxism | Yes | 94 | 41.0 |
| No | 135 | 58.9 | |
| Total | 229 | 100 | |
| Technique | Direct | 82 | 35.8 |
| Indirect | 147 | 64.1 | |
| Total | 229 | 100 | |
| Number of Cusps | One | 87 | 44.6 |
| Two | 67 | 34.3 | |
| Three | 8 | 4.10 | |
| Four | 14 | 7.17 | |
| Five | 19 | 9.74 | |
| Total | 195 | 100 | |
| Time in mouth (years) | 05-1.9 | 84 | 36.7 |
| 2-3.9 | 57 | 4.9 | |
| 4-5.9 | 23 | 10.1 | |
| 6-7.9 | 29 | 12.6 | |
| More than 8 | 36 | 15.7 | |
| Total | 229 | 100 | |
Table 2: Distribution of restorations according to independent variables
Table 3 shows the qualitative evaluation of the restorations using the FDI criteria. In the Figures 1, 2, 3, 4 and 5 Kaplan-Meier survival curves demonstrate the clinical behavior of different material restorations, techniques, dental vitality, and number of substituted cusps.
| Direct Composite Resin | Indirect Composite Resin | Indirect Ceramic | Kruskal-Wallis p | |||||
Scores N(1/2/3/4/5) |
Clinically Acceptable Restorations | Scores n(1/2/3/4/5) | Clinically Acceptable Restorations | Scores n(1/2/3/4/5) | Clinically Acceptable Restorations | |||
| Esthetic Properties | Surface Luster | 76(20/50/6/0/0)A | 100% | 72(50/21/1/0/0)B | 100% | 44(42/1/1/0/0)B | 100% | 0.001 |
| Manchamento Superficial | 76(27/40/9/0/0)A | 100% | 72(47/20/5/0/0)B | 100% | 44(42/1/1/0/0)C | 100% | 0.001 | |
| Marginal Staining | 76(5/41/29/1/0)A | 98.6% | 72(10/53/9/0/0)B | 100% | 44(24/17/3/0/0)C | 100% | 0.001 | |
| Color Match/ Transfucency | 76(53/21/2/0/0)A | 100% | 72(68/2/2/0/0)B | 100% | 44(43/1/0/0/0)B | 100% | 0.001 | |
| Esthetic Anatomic Form | 76(13/34/29/0/0)A | 100% | 72(43/24/5/0/0)B | 100% | 44(40/2/2/0/0)C | 100% | 0.001 | |
| Fracture and Retention | 82(63/0/5/10/4)A | 82.9% | 88(68/0/1/3/16) | 78.4% | 59(43/1/0/0/15) | 74.5% | 0.551 | |
| Marginal Adaptation | 76(8/55/11/2/0)AB | 97.3% | 72(15/49/8/0/0)B | 100% | 44(10/32/2/0/0)A | 100% | 0.048 | |
| Functional Properties | Occlusal Wear | 76(17/43/16/0/0)A | 72(35/34/3/0/0)B | 100% | 44(39/3/2/0/0)C | 100% | 0.001 | |
| Contact Point | 57(19/14/7/17/0)A | 70.1% | 62(30/19/9/4/0)AB | 93.5% | 43(26/5/10/2/0)B | 95.3% | 0.008 | |
| Radiographic Examination | 76(62/6/2/0/6)A | 92.6% | 88(60/10/1/0/17)B | 80.6% | 59(38/4/1/0/16)AB | 74.5% | 0.015 | |
| Patient’s View | 76(76/0/0/0/0) | 100% | 72(67/2/3/0/0) | 100% | 44(44/0/0/0/0) | 100% | 0.080 | |
| Biological Properties | Postoperative Sensitivity | 76(74/2/0/0/0) | 100% | 72(71/1/0/0/0)A | 100% | 44(42/2/0/0/0) | 100% | 0.586 |
| Recurrence of Caries, Erosion, Abfraction | 76(71/0/3/2/0) | 97.3% | 72(68/0/1/3/0) | 95.8% | 44(43/0/0/1/0) | 97.7% | 0.600 | |
| Tooth Integrity | 76(73/0/2/1/0) | 98.6% | 72(71/0/1/0/0) | 100% | 44(44/0/0/0/0) | 100% | 0.301 | |
| Peridontal Response | 68(60/0/5/3/0)AB | 95.5% | 72(70/0/1/1/0)B | 98.6% | 44(44/0/0/0/0)A | 100% | 0.013 |
Each criteria was evaluated in scores of 1-5: 1-3 when the restoration is clinically acceptable, while 4 e 5 designate failure (Kappa=0.87). Dunn’s Test- Equal letters in the same line do not differ
Table 3: Clinical evaluation of restorations according to FDI criteria
In the Table 4, Cox regression analysis showed that restorations made in women had a 58% of protection against failure when compared to men (HR = 0.416; p = 0.001). In addition, there was no association among material, technique, tooth type, number of cusps, dental vitality and bruxism with risk of failure of the restorations.
| Independent Variables | HR | Confidence Interval 95% | p-value |
| Gender | 0.416 | 0.245-0.706 | 0.001 |
| Tooth | 0.843 | 0.468-1.521 | 0.572 |
| Material | 1.229 | 0.633-2.385 | 0.542 |
| Tooth Vitality | 0.981 | 0.587-1.639 | 0.943 |
| Bruxism | 1.430 | 0.840-2.435 | 0.187 |
| Technique | 0.441 | 0.147-1.323 | 0.144 |
| N cusps | 1.152 | 0.933-1.423 | 0188 |
Table 4: Cox regression analysis with Hazard Ratio (HR) adjusted for independent variables and restoration failures.
Direct composite restorations presented a 34.1% of failure, with AFR of 9.6%. Composite onlays (ceromer) presented 27.3% of failure, with AFR of 7.1%. Ceramic onlays showed 28.8% of failure rate with AFR of 7.6%. Restorations performed in men presented a 45% failure, with AFR of 13%, whereas for women there were 24.9% of failure, with AFR of 6.4%, in an average of 4.3 years of follow-up. The most common reason for failure was fracture and retention, occurring in 48 cases (69.56% of the failures).
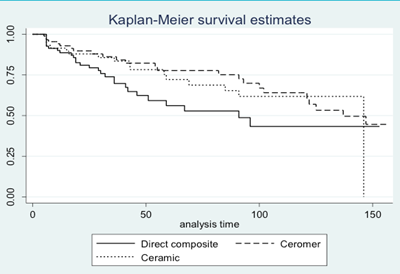
Figure 2: Kaplan-Meier survival curves for restorations with different materials (log-rank: p = 0.110) (time in months)
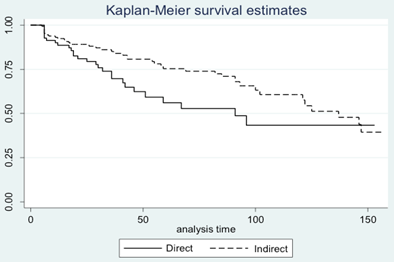
Figure 3: Kaplan-Meier survival curves for restorations with different techniques (log-rank: p = 0.045) (time in months)
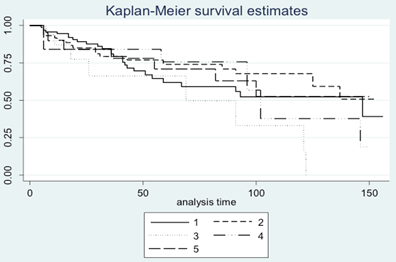
Figure 4: Kaplan-Meier survival curves for restorations with different numbers of involved cusps (log-rank: p = 0.257)(time in months)
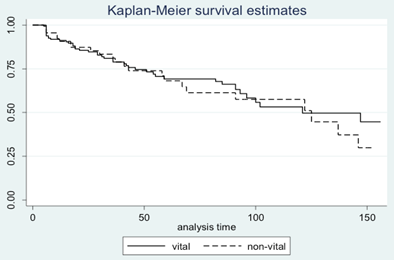
Figure 5: Kaplan-Meier survival curves for restorations on vital and non-vital teeth (log-rank: p = 0.678) (time in months)
Discussion
The present retrospective study evaluated the performance of indirect onlay restorations made of composite resin and ceramic and direct composite restorations with cusp involvement, using the FDI evaluation criteria.
According to some authors [7, 14], the longevity of direct restorations can be influenced by factors such as: operator, material, location and size of the restoration, caries risk and bruxism. In the present study, according to the Cox Regression, the independent variables that included material, tooth type, dental vitality, bruxism, technique and number of restored cusps had no association with the failures observed in the restorations. Other authors also found no correlation between location, size and class type in the longevity of the restorations [17, 18]. Other studies [9, 12, 13, 14, 19] concluded that restorations with a greater number of faces involved and in molar teeth tend to fail more.
According to Demarco., et al. (2012) [7], bruxism influences the development of fatigue in tooth-restoration interface, resulting in long-term fracture. In the present study, the fact of bruxism has not demonstrated an association with failure and the high incidence of fractures can be related to the occurrence of this parafunction that was self-reported by the patient and not diagnosed by the dentist at the time of the clinical evaluation. 31.4% of the patients reported suffering with the bruxism symptoms. Manfredini et al. (2013) [20] showed similar results in a systematic review that evaluated the prevalence of bruxism in adults.
Among the independent variables, only gender presented significant statistical differences, revealing that in female patients there was a lower prevalence and a lower risk of failure of restorations. In a clinical evaluation [21] with 3 years of follow-up of extensive composite resin restorations involving cusps in molars, it was observed that restoration failures were approximately 5 times more prevalent in men than in women, relating this outcome with differences in masticatory forces between gender.
There was no statistically significant difference between direct and indirect restorations in dental integrity, postoperative sensitivity, patient opinion, caries recurrence, erosion or abfraction, and fracture and retention criteria. The low incidence of caries found in this analysis corroborates with other evidence [18, 20, 22], although restorative material fracture and/or caries have been reported as the main reasons for failure of restorations in several other studies [4, 7, 9, 12, 14, 17, 19, 21, 22].
In the present research, fracture and retention criterion has been shown to be one of the main reasons of failure for both direct and indirect restorations. However, the failures found in direct restorations were mostly classified as repairable (Score 4), as opposed to the failures found in indirect restorations, which had mostly catastrophic fractures, demanding the replacement of it (Score 5). Cubas., et al. (2011) [2] observed a higher prevalence of material-restricted fractures in groups with ceramic restorations with cusps (onlays). Alshiddi and Aljinbaz (2016) [23] concluded that most of the fractures detected in composite onlays also occurred in the material, which has the characteristic of absorbing impacts and protecting the dental structure. Kujis et al. (2006) [24] concluded that restorations containing cusps (indirect composite, ceramics and direct composite restorations) have comparable resistance to fatigue and fracture. However, indirect restorations tend to suffer more cohesive fractures than direct restorations, pointing out that indirect materials do not necessarily perform better than direct in posterior restorations.
In the present study, direct restorations performed worse than indirect restorations in the qualitative analysis. Composite onlays seem to have better mechanical properties than direct composite restorations [22, 24, 25], having their increased hardness and wear resistance due to the additional polymerization and greater conversion of monomers to polymers. Besides, the technique allows the control of polymerization contraction, proximal contour and the contact point obtainment [15, 26]. Indirect restorations also show superior color stability, resulting in better characteristics when compared to direct composite restorations [22, 26]. In this research, indirect restorations presented better characteristics when compared to direct restorations in the following criteria: color match and translucency, surface luster, marginal staining, occlusal wear and esthetic anatomic form.
According to literature, indirect restorations have presented good survival rates and low annual failure rates [15, 27]. Although direct composite restorations presented inferior characteristics in some of the evaluated criteria, they have the advantages of not requiring an invasive tissue removal, being able to be built in only one session and demanding a lower cost [27, 28], revealing good clinical performance [7, 9, 10, 28, 29], with an annual failure rate of 1.5% in 22 years of follow-up [10] and a survival rate of 63% with annual failure rate of 1.1% with up to 30 years of follow-up [18] for restorations placed in dental schools. In the present study, the survival rate of restorations placed by students in a dental school was 69.9%.
In the marginal adaptation criterion, significant statistical differences were found between the direct and indirect techniques. However, when comparing composite onlays with ceramic onlays, the latter has better scores. The study by Fasbinder et al. (2005) [30], compared indirect ceramics and composite restorations with respect to marginal adaptation and found no statistical differences between them after three years of follow-up, classifying both materials as clinically excellent. The study by Van Dijken (2000) [4] also demonstrated that the marginal adaptation of the restorations remained clinically good after 11 years of evaluation.
No restoration was classified as clinically deficient (Score 5) in contact point criterion. However, many failures in score 4 were found for direct restorations in this criterion, which demands the need for intervention and repair in these restorations. Ceramic onlays presented better performance than direct composite restorations, but did not present statistical differences when compared to composite onlays. The latter group also had similar behavior when compared to the direct restorations, with no statistically significant differences between them. Lack of proximal contact was one of the main reasons for failure found in the clinical evaluation of 10-year composite restorations by Raskin et al. (1999) [28] and also in the study by Opdam et al. (2004) [29].
One limitation found in the present study was the incorrect filling of patients' records, where the students often did not detail the restoration that was performed, making it difficult to collect data and excluding the patient from the study. These disadvantages have also been reported by Opdam et al. (2004) [29], who considered the retrospective design and lack of information in the medical records encountered for the development of their study.
The three evaluated type of restorations (direct, ceromer and ceramic) demonstrated a good long-term clinical performance in the rehabilitation of posterior teeth with cusp recovers. Although direct restorations demonstrated the worst behavior in the qualitative analysis, they still remained in function, presenting clinical satisfactory properties during the evaluation period, emphasizing the importance of this material that also has its use consecrated in modern Dentistry and that did not present statistical differences in the longevity of the restorations when compared with indirect restorations.
Finally, when understood that both techniques present their advantages and disadvantages, the selection of the best treatment protocol for posterior teeth with cusp involvement becomes a subjective option by the dentist, who must consider the amount of tooth structure, clinical cost and time, as it is possible to reach a good clinical longevity of the restorations using both direct and indirect techniques. Further, long-term studies should be performed with the purpose of making comparisons, recommendations and confirming the findings of the present study on the direct and indirect techniques and their respective restorative materials.
Conclusion
Within the limitations of the present study, it is possible to conclude that:
- Restorations with cusp involvement have a survival rate of 69.9% in 4.3 years, with direct composite resin, indirect composite or ceramics showing similar longevity, regardless of the number of cusps involved.
- Indirect restorations had lower annual failure rate than direct restorations and presented better performance in the criteria of surface luster, marginal staining, surface staining, color match and translucency, esthetic anatomic form, occlusal wear, marginal adaptation, periodontal response and contact point.
- Female patients presented lower prevalence and lower risk of failure of restorations than male patients.
- The most prevalent type of failure in restorations with cusp involvement was fracture and retention.
References
- Lempel E., et al. “Clinical evaluation of lithium disilicate versus indirect resin composite partial posterior restorations - A 7.8-year retrospective study”. Dental Materials 39.12 (2023): 1095-1104.
- Gloria Beatriz de Azevedo Cubas., et al. “Fracture resistance of premolars restored with inlay and onlay ceramic restorations and luted with two different agents”. Journal of Prosthodontic Research 55.1 (2011): 53-59.
- PA Brunton., et al. “Fracture resistance of teeth restored with onlays of three contemporary tooth-colored resin-bonded restorative materials”. Journal of Prosthetic Dentistry 82.2 (1999): 167-171.
- Van Dijken JW. “Direct resin composite inlays/onlays: an 11 year follow-up”. Journal of Dentistry 28.5 (2000): 299-306.
- Camillo D'Arcangelo., et al. “Five-year retrospective clinical study of indirect composite restorations luted with a light-cured composite in posterior teeth”. Clinical Oral Investigations 18.2 (2014): 615-624.
- Ulrike Stephanie Beier., et al. “Clinical performance of all-ceramic inlay and onlay restorations in posterior teeth”. The International Journal of Prosthodontics 25.4 (2012): 395-402.
- Flávio F Demarco., et al. “Longevity of posterior composite restorations: not only a matter of materials”. Dental Materials 28.1 (2012): 87-101.
- Brunthaler A., et al. “Longevity of direct resin composite restorations in posterior teeth”. Clinical Oral Investigations 7.2 (2003): 63-70.
- Da Rosa Rodolpho PA., et al. “A clinical evaluation of posterior composite restorations: 17-year findings”. Journal of Dentistry 34.7 (2006): 427-435.
- Da Rosa Rodolpho PA., et al. “22-Year clinical evaluation of the performance of two posterior composites with different filler characteristics”. Dental Materials 27.10 (2011): 955-963.
- Opdam NJ., et al. “A retrospective clinical study on longevity of posterior composite and amalgam restorations”. Dental Materials 23.1 (2007): 2-8.
- Opdam NJ., et al. “Longevity of posterior composite restorations: a systematic review and meta-analysis”. Journal of Dental Research 93.10 (2014): 943-949.
- Manhart J., et al. “Three-year clinical evaluation of direct and indirect composite restorations in posterior teeth”. Journal of Prosthetic Dentistry 84.3 (2000): 289-296.
- Marcondes M., et al. “Clinical Evaluation of Indirect Composite Resin Restorations Cemented with Different Resin Cements”. The Journal of Adhesive Dentistry 18.1 (2016): 59-67.
- Hickel R and Manhart J. “Longevity of restorations in posterior teeth and reasons for failure”. The Journal of Adhesive Dentistry 3.1 (2001): 45-64.
- Scheibenbogen-Fuchsbrunner A., et al. “Two-year clinical evaluation of direct and indirect composite restorations in posterior teeth”. Journal of Prosthetic Dentistry 82.4 (1999): 391-397.
- Barkmeier WW., et al. “Localized and generalized simulated wear of resin composites”. Operative Dentistry 40.3 (2015): 322-335.
- Pallesen U and van Dijken JW. “A randomized controlled 30 years follow up of three conventional resin composites in Class II restorations”. Dental Materials 31.10 (2015): 1232-1244.
- Van de Sande FH., et al. “Patient risk factors' influence on survival of posterior composites”. Journal of Dental Research 92.7 (2013): 78S-83S.
- Manfredini D., et al. “Epidemiology of bruxism in adults: a systematic review of the literature”. Journal of Orofacial Pain 27.2 (2013): 99-110.
- Van Nieuwenhuysen JP., et al. “Long-term evaluation of extensive restorations in permanent teeth”. Journal of Dentistry 31.6 (2003): 395-405.
- Pallesen U and Qvist V. “Composite resin fillings and inlays. An 11-year evaluation”. Clinical Oral Investigations 7.2 (2003): 71-79.
- Alshiddi IF and Aljinbaz A. “Fracture resistance of endodontically treated teeth restored with indirect composite inlay and onlay restorations - An in vitro study”. Saudi Dental Journal 28.1 (2016): 49-55.
- Kujis RH et al. “A comparison of fatigue resistance of three materials for cusp-replacing adhesive restorations”. Journal of Dentistry 34.1 (2006): 19-25.
- Cetin AR., et al. “A five-year clinical evaluation of direct nanofilled and indirect composite resin restorations in posterior teeth”. Operative Dentistry 38.2 (2013): E1-11.
- Monaco C., et al. “Short-term clinical evaluation of inlay and onlay restorations made with a ceromer”. The International Journal of Prosthodontics 14.1 (2001): 81-86.
- Angeletaki F., et al. “Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis”. Journal of Dentistry 53: 12-21.
- Raskin A., et al. “Clinical evaluation of a posterior composite 10-year report”. Journal of Dentistry 27.1 (1999): 13-19.
- Opdam NJ., et al. “Five-year clinical performance of posterior resin composite restorations placed by dental students”. Journal of Dentistry 32.5 (2004): 379-383.
- Fasbinder DJ., et al. “The clinical performance of CAD/CAM-generated composite inlays”. Journal of the American Dental Association 136.12 (2005): 1714-1723.
Citation:
Carolina Berwanger., et al. “A Retrospective Clinical Evaluation of Direct and Indirect Aesthetic Restorations with Cuspal Replacement”. Oral Health and Dentistry 7.1 (2024): 12-21.
Copyright: © 2024 Dr. Carolina Berwanger., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.