Research Article
Volume 1 Issue 1 - 2016
Prevalence and Patterns of Multimorbidity of Tuberculosis, Human Immunodeficiency Virus and Diabetes Mellitus in Anambra State, Nigeria
1Microbiology Department, Abia State University, P.M. B 2000, Uturu, Nigeria
1Food Science and Technology Department, Abia state university, P.M. B 2000, Uturu, Nigeria
1Food Science and Technology Department, Abia state university, P.M. B 2000, Uturu, Nigeria
*Corresponding Author: Nwachukwu ON, Microbiology Department, Abia State University, PM B 2000, Uturu, Nigeria.
Received: August 26, 2016; Published: November 21, 2016
Abstract
Background/purpose: The proportion of subjects with multiple medical conditions is increasing worldwide. Coexistence of tuberculosis (TB), human immunodeficiency virus (HIV) and diabetes mellitus (DM) in the same person was investigated.
Materials and Methods: A prospective survey was conducted among patients aged ≥ 15 years who presented at TB/directly observed treatment clinics of Nnamdi Azikiwe University Teaching Hospital, Nnewi, and St. Charles Borromeo Hospital, Onitsha. Diagnosis of pulmonary tuberculosis was based on National Tuberculosis Guidelines using Ziehl-Neelsen technique for acid fast bacilli in sputum. Fasting blood glucose concentration was performed using glucose oxidase method and diabetes diagnosed if fasting blood glucose concentration was ≥ 126 mg/dl. HIV sero-status was determined by a serial testing using three rapid test kits, including Determine, UniGold, and StatPak.
Results: A total of 1487 presumptive TB cases participated in the study. The concomitant occurrence of TB/HIV/DM in the same person was observed in 24 out of 1487 patients (1.6%). A higher prevalence (2.3%) was seen in males than females (1.1%) and in the age group of 25-34 years. Co-morbidity patterns revealed TB/HIV co-infection rate of 6.4% and TB/DM rate of 3.6%. In both cases, males and the age group of 25-34 years had a higher co-infection rate. HIV infection was the most common morbidity (52%) with infection higher in females.
Conclusion: The prevalence of multi-morbidity of TB/HIV/DM in Anambra State was 1.6%. Males and the age group of 25-34 years had higher morbidity. It is therefore important to integrate the management of TB/HIV/DM to improve early case detection and reduce their morbidities.
Keywords: Tuberculosis; Human immunodeficiency virus; Diabetes mellitus; Multi-morbidity
Abbreviations: MM-Multi: Morbidity; TB: Tuberculosis; PTB: Pulmonary Tuberculosis; HIV: Human Immunodeficiency Virus; DM: Diabetes Mellitus; AIDS: Acquired Immune Deficiency Syndrome; NAUTH: Nnamdi Azikiwe University Teaching Hospital; SCBH: St. Charles Borromeo Hospital.
Introduction
Multi-morbidity (MM) is defined as the co-existence of more than one chronic condition in the same person over a specific period [1-3]. Chronic conditions consist of non-communicable conditions, long term mental disorders, and ongoing physical/structural impairment, as well as persistent communicable conditions such as tuberculosis and human immunodeficiency virus infections [4].
Tuberculosis (TB), diabetes mellitus (DM) and human immunodeficiency virus infection (HIV) rank among the top ten causes of mortality all over the world [5]. Of the three, two are communicable diseases i.e TB and HIV, and diabetes is a chronic non-communicable condition. The association between communicable and non-communicable diseases has been recognized for centuries [6].
It has become clear that two of the most common infectious diseases in Africa, tuberculosis and HIV/AIDs may also be closely related to chronic communicable diseases [7]. Different studies have documented that diabetes predispose to tuberculosis and increase the risk of progression from latent tuberculosis infection to active tuberculosis [8-11]. Antiretroviral therapy for HIV infection, on the other hand may increase the risk of metabolic syndrome and thus predispose to Type 2 diabetes and cardiovascular [12-14]. The epidemic growth of diabetes occurs in the developing countries where tuberculosis is highly endemic [15].
Pulmonary tuberculosis remains the disease with the highest global mortality for a single infectious agent [16]. Nigeria is ranked high among the world’s 22 high TB burdened countries. Nigeria is also estimated to have the highest number of people with diabetes mellitus (approximately 1, 218, 0000 people affected) while Reunion has the highest prevalence of diabetes in the African Region [17].
Against this background, the burden of HIV and TB remains high in Nigeria. HIV prevalence in Nigeria stands at 4.6% in the general population [18]. How then will overburdened public health services in resource-poor countries that have high rates of infection with HIV, poor tuberculosis control infrastructures and crowded living conditions cope as the overlap between those with communicable and non-communicable disease increase?
We therefore aimed to study the patterns and prevalence of tuberculosis, HIV, and diabetes multi-morbidity in Anambra state, Nigeria.
Materials and Methods
This prospective study was carried out at Nnamdi Azikiwe University Teaching Hospital (NAUTH), Nnewi and St. Charles Borromeo Hospital (SCBH), Onitsha, all in Anambra state, Nigeria. NAUTH is the largest tertiary hospital and referral centre in Anambra state. SCBH is a foremost missionary hospital with state-of-the-art facilities. In both hospitals, anti-tuberculosis and anti-retroviral medicines are provided free.
Subjects
Individuals aged 15 years and older who were presumptive TB cases (had cough for ≥ 2 weeks) who either self presented to the TB/directory observed treatment clinic or referred from peripheral health centers for assessment were invited to participate and enrolled at the time of presentation to the clinic. A random sampling of the presumptive TB cases was adopted
Individuals aged 15 years and older who were presumptive TB cases (had cough for ≥ 2 weeks) who either self presented to the TB/directory observed treatment clinic or referred from peripheral health centers for assessment were invited to participate and enrolled at the time of presentation to the clinic. A random sampling of the presumptive TB cases was adopted
Methods
Diagnosis of smear positive pulmonary tuberculosis was based on the National TB Guidelines. Presumptive TB cases submitted two sputum specimens on the spot within 1 hour interval. Smears were stained using the Ziehl-Neelsen technique. In accordance with recent WHO policy change [19], all smears with one or more AFB/100 HPF were considered positive.
Diagnosis of smear positive pulmonary tuberculosis was based on the National TB Guidelines. Presumptive TB cases submitted two sputum specimens on the spot within 1 hour interval. Smears were stained using the Ziehl-Neelsen technique. In accordance with recent WHO policy change [19], all smears with one or more AFB/100 HPF were considered positive.
Fasting blood glucose (FBG) concentration was determined using the glucose oxidase method and diabetes confirmed if FBG concentration was ≥ 126 mg/dl [20].
The Nigerian National HIV testing algorithm recommended by the World Health Organization for resource- poor countries was used for HIV testing. It is a serial testing using 3 rapid test kits namely Determine (Inverness, Japan), UniGold (Trinity, Ireland) and StatPak (chemodiagnostic, Spain). Determine was used as the first screening test kit. This was followed by uniGold, to confirm a positive result while StatPak served as a tie breaker.
Ethical approval for the study was obtained from ethical committees of both hospitals. All patients consented to participate in the study.
Results
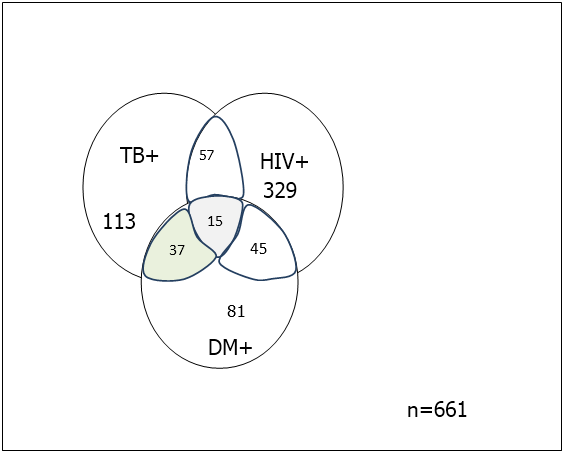
A total of 1487 presumptive TB cases participated in the study. The concomitant occurrence of TB/HIV/DM in the same individual revealed a prevalence of 1.6% (24/1487). Males were concomitantly more infected (2.3%) than females (1.1%) (Figure: 1).
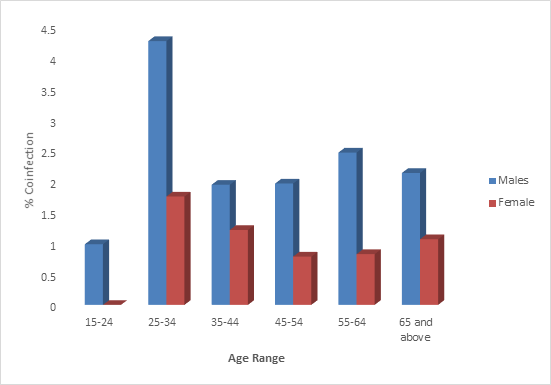
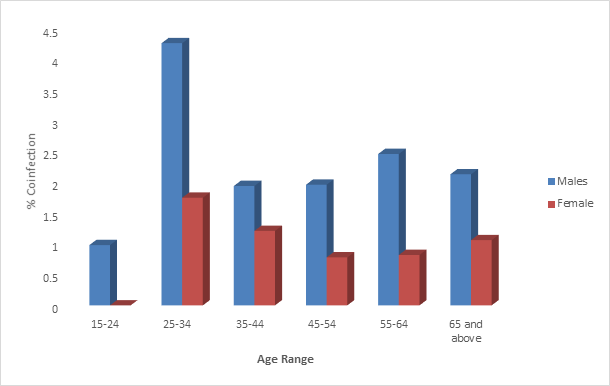
Figure 2 shows the age distribution of concomitant TB/HIV/DM patients. The age group of 25-34 years had a higher infection rate.
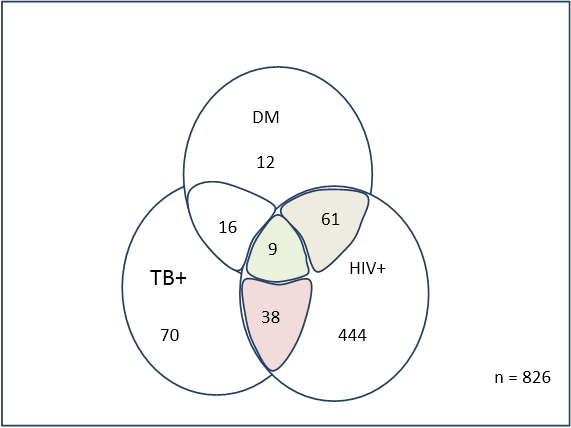
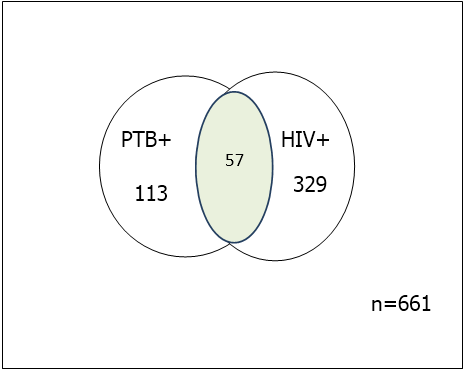
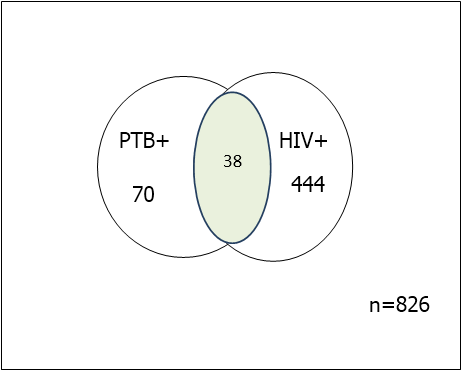
The co- morbidity patterns shows a TB/HIV co- infection rate of 6.4%. TB/HIV co-infection was higher in males (8.6%) than in females (4.6%) (Figure 3).
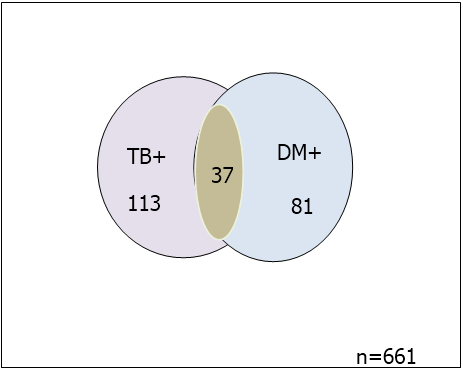
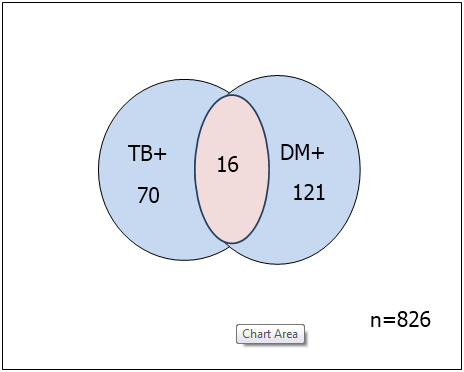
TB/DM co-infection rate of 3.6% was observed in the study. Males 37(5.6%) were more infected than females 16(1.9%)( Figure 4).
The age group of 25-34 years was more coinfected while 15-24years had the least infection (Figure 5).
Among the 1487 patients, HIV infection was the most common morbidity (52%). Overall, the prevalence of tuberculosis, HIV and diabetes was higher in females (54.8%) than males (45.2%) as presented in table 1
| Disease category | N = 1487 Males infected (%) Females infected (%) | Total (%) | |
| Pulmonary tuberculosis | 113 (61.7) | 70 (38.3) | 183 (12.3) |
| Diabetes mellitus | 81 (40.1) | 121 (59.9) | 202 (13.6) |
| HIV | 329 (42.60 | 444 (57.4) | 773 (52.0) |
| Total | 523 (45.2) | 635 (54.8) | 1158 (77.9) |
Table 1: Prevalence TB, HIV and DM in the study population
Discussion
The concept of multi-morbidity is an issue of public health significance. In our study, the concomitance of TB/HIV/DM in the same individual was found in 24 of the 1487 patients, giving a prevalence of 1.6%. Similar studies in Brazil, South Africa and Abakaliki, Nigeria [21-23] had reported prevalence rates of 1.14%, 3.5% and 2.8% respectively. This highlights the importance of multi-morbidity.
Multi-morbidity result is in complex disease patterns that may have multiplicative and not merely addictive consequences and health outcomes. This could diminish patient’s ability to manage their conditions. Such consequences may include increase in mortality, decrease quality of life, complications of treatment and higher utilization of health care system [24].
Nigeria’s poor health care systems may not cope with such burden. Multi-morbidity of TB/HIV/DM was more frequent in males and in the age group of 25-34 years. Gender and age has been associated with both tuberculosis and multi-morbidity [25] and other studies had reported that men develop tuberculosis more often [26-27]. The study areas, Nnewi and Onitsha are populated by male traders and trading in these areas are often conducted in overcrowded environments which could aid tuberculosis transmission and multi-morbidity. Its prevalence in young people of 25-34 years could have serious could have serious economic /health implications as this subset is Nigeria’s predominant population group [28] and the most productive age range of any society [29]. Labor force in the country may be adversely affected and various sectors of the economy will suffer.
Tuberculosis has well been documented as the most important opportunistic infection among HIV-infected patients [30]. In this study, TB/HIV co-infection rate of 6.4% was observed. This is in line with some previous TB/HIV co-infection rates in Nigeria: 5.9% in the Niger Delta [31], 6.3% in Onitsha [32], but lower than 18.4% observed in Lagos [33] and 19% in Durban [34]. The high prevalence rates suggest strong association between tuberculosis and HIV infection in the study areas. The higher TB/HIV in males could be as a result of attitude of men towards indiscriminant sex.
Diabetes and tuberculosis (DM/TB), two diseases of immense public health significance has been linked together [35]. We found a DM/TB prevalence of 3.6% with a higher infection in the age group of 25-34 years. A similar but higher prevalence of 5.3% was earlier reported in Abakaliki, Nigeria. Previous literature supports that diabetes is an important risk factor for the development of pulmonary tuberculosis [6,8]. A possible mechanism of the association of the diabetes and tuberculosis is the depression of the immune response from protective immune system which in turn facilitates the progression of latently infected Mycobacterium tuberculosis to active tuberculosis [36].
Human immunodeficiency virus infection was the most common morbidity (52%) in this study. This was an expected result as there is a high prevalence of HIV / AIDS in the country. Nigeria also accounts for 10% of global HIV infection [17]. Females had higher HIV infection than males. It has earlier been reported [37, 38] that HIV prevalence was three times higher in females than males. The cultural norms in the study areas where women are expected to meet male sexual needs, poverty and prostitution might account for higher HIV infection in women.
Conclusion
The multi-morbidity of TB/HIV/DM revealed a prevalence of 1.6% in Anambra State. Multi-morbidity was more frequent in males and age group of 25-34 year old. It is therefore imperative that healthcare systems in Nigeria should integrate TB/HIV/DM control programmes to improve early case detection and reduce their morbidities.
Conflict of interest
We have no conflict of interest to declare
We have no conflict of interest to declare
References
- Prados TA., et al. “Multimorbidity patterns: a systematic review”. Journal of Clinical Epidemiology67.3 (2014): 254-266.
- Uijen AA and Lisdonk EH. “Multimorbidity in primary care: prevalence and trend over the last 20 years”. European Journal of General Practice14.suppl 1 (2008): 28-32.
- Fortin M., et al. “Prevalence of multi-morbidity among adults seen in family practice”. The Annals of Family Medicine 3.3 (2005): 223-228.
- World Health Organization. Innovative care for chronic condition: Building blocks for action Geneva. World Health Organization 2002.
- World Health Organization. Global Tuberculosis Control 2011. Geneva, Switzerland.
- Jeon C and Murray M. “Diabetes mellitus increases the risk of active tuberculosis: A systematic review of 13 observational studies”. PLOS Medicine5.7 (2008): 1091-1101.
- Young F., et al. “A review of co-morbidity between infectious and chronic diseases in sub-Saharan African: TB and diabetes mellitus, HIV and metabolic syndrome and the impact of globalization”. Global and Health 5.9 (2009):
- Mekonnem S., et al. “High magnitude of diabetes mellitus among diabetes patients in Ethiopia”. British Journal of Medicine and Medical Research4.3 (2014): 862-872.
- Stevenson CR., et al. “Diabetes and Tuberculosis: the impact of diabetes epidermic on tuberculosis incidence”. BMC Public Health7 (2007): 234.
- Nwachukwu NO., et al. “Prevalence of diabetes mellitus among tuberculosis suspects in Nnewi, Nigeria”. Journal of Microbiology and Biotechnology Research6.2 (2016): 1-5.
- Balakrishnan S., et al. “High diabetes prevalence among tuberculosis cases in Kerala, India”. PLOS ONE 7.10 (2012): e46502.
- Brown TT., et al. “Antiretroviral therapy and the prevalence and incidence of diabetes mellitus in the multicenter AIDS cohort Study”. Archives of Internal Medicine 165.10 (2005): 1179-1184.
- Pao V., et al. “HIV therapy, metabolic syndrome, and cardiovascular risk”. Current Atherosclerosis Reports 10.1 (2008): 61-70.
- Falasca K., et al. “Metabolic syndrome and cardiovascular risk in HIV-infected patients with lipodystrophy”. International Journal of Immunopathology and Pharmacology 20.30 (2007): 519-527.
- Ruslari R., et al. “Implication of the Global increase of diabetes for tuberculosis control and patient care”. Tropical Medicine & International Health15.11 (2010): 1289-1299.
- Atlink H. “From the local to the global: fifty years of research on tuberculosis”. Medical History 59 (2015): 3-5.
- International Diabetes Federation. International Diabetes Federation diabetes atlas-2013. 6th Ed.
- USAID. Nigeria Tuberculosis factsheet. United States Embassy in Nigeria. January 2012.
- World Health Organization. Framework for implementing new tuberculosis diagnosis. World Health Organization 2010. Geneva, Switzerland.
- World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its implications. World Health Organization 1999. WHO/NCD/NCS/99.2
- Reis- Santos B., et al. “Prevalence and Patterns of multimorbidity among tuberculosis patients in Brazil: a cross-sectional study. International Journal for Equity in Health 12.1 (2013): 61.
- Oni T., et al. “Patterns of HIV, TB, and Non-communiocable disease multi-morbidity in peri-urban South Africa- a cross sectional study”. BMC Infectious Diseases 15.20 (2015):
- Anwara O., et al.“The prevalence of diabetes mellitus in HIV seropositive subject coinfected with mycobacterium tuberculosis”. Journal of AIDS and HIV Research7.9 (2015): 109-116.
- Gijsen R., et al. “Causs and consequences of co-morbidity: a review”. Journal of Clinical Epidemiology54.7 (2001): 661-674.
- Fortin M., et al. “A systematic review on multiborbidity: towards a more uniform methodology”. The Annals of Family Medicine10.2 (2012): 142-151.
- Lawn SD and Zumla AI. “Tuberculosis”. Lancet 378.9785 (2011): 57-72.
- World Health Organization. Global Tuberculosis Report. Executive summary. World Health Organization 2013. WHO/HTM/B/2013.15
- 2006 Census. Analytical report at the national level. National Population commission, Nigeria.
- The World’s youth 2006 data sheet. Population reference Bureau. United Nations.
- Pawloski A., et al. “Tuberculosis and HIV coinfection”. PLOS pathogens 8.2 (2012): e1002464.
- Nwabuko CO., et al. “Prevalence of tuberculosis-HIV coinfection and relationship between tuberculosis and CD4 count/ESR in HIV patients in Niger Delta region of Nigeria”. IOSR JDMS 2.4 (2012): 01-04.
- Nwachukwu NO., et al. “Prevalence of tuberculosis in HIV positive subjects in Onitsha”. Japanese Journal of Medical Science and Biology 3.2 (2013): 1-6.
- Onubogu CC., et al. “Prevalence of tuberculosis and human immunodeficiency virus (TB/HIV) coinfection amongst patient with broncho pulmonary disorders in Lagos”. African Journal of Microbiology Research 4.18 (2010): 1904.
- Basset W., et al. “Intensive tuberculosis screening for HIV-infected patients starting anti rectroviral therapy in Durban, South Africa”.Clinical Infectious Diseases 51.7 (2010): 823-829.
- Sarah LB and Paul G. “The tubercular diabetic: The impact of diabetes mellitus on tuberculosis and its threat to global tuberculosis control”.Clinical Medicine11.4 (2011): 344-347.
- Sulaiman SA., et al. “Prevalence of hypertension, control of blood pressure and treatment in hypertensive with type 2 diabetes in Hospital University Sains Malaysia”. Diabetes & Metabolic Syndrome 5.3 (2011): 115-119.
- UNAIDS. UNAIDS report on the Global AIDS Epidemic 2013. Geneva, Switzerland.
- UNFPA. United Nations population Fund. South Africa- HIV report. United Nations Population Fund 2014.
Citation:
Nwachukwu ON., et al. “Prevalence and Patterns of Multimorbidity of Tuberculosis, Human Immunodeficiency Virus and Diabetes Mellitus in Anambra State, Nigeria”. Clinical Biotechnology and Microbiology 1.1 (2016): 1-8.
Copyright: © 2016 Nwachukwu ON., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.