Review Article
Volume 3 Issue 1 - 2018
Review on Prevalence, Ignorance and Seriousness of Postpartum Depression in Developing Countries
MBBS students of Jinnah Sindh Medical University, Karachi
*Corresponding Author: Ali Mustufa, MBBS student of Jinnah Sindh Medical University, Karachi.
Received: November 24, 2018; Published: December 29, 2018
Abstract
Postpartum depression is a mood disorder occurring after childbirth, it is a serious issue which can ultimately cause death if ignored. Studies suggest PPD occurs three times more in developing countries as compared to developed countries. Cultural, economic, racial, and financial factors all play a role in causing, diagnosing and curing Postpartum or postnatal depression. It affects not only the mental health of parents but also the physical growth and mental development of the offspring so it is a disorder not to be taken lightly.
Introduction
Transition to parenthood represents a significant life event with increasing susceptibility to a number of physical, emotional and behavioral changes in both males and females. Postpartum depression, also known as postnatal depression, is the most common cognitive and mental disorder that affects approximately 10-20% of new mothers and growing scientific data indicates that both the parents are affected by this change. The maternal stress levels are mostly linked to paternal ones. The first four weeks after partum serve as a crucial phase of parent’s life and should be considered as a critical stage comprising of extreme sadness, anxiety and exhaustion that may make it difficult for them to complete their daily activities and could have a significant impact on the child’s mental as well as physical health [1].
It is important to highlight the fact that while PPD may seem anew, in most cases it emerges from prenatal depression which is not diagnosed and treated during pregnancy. Depression during pregnancy is correlated with a number of risk factors that can cause mothers to ignore their health as well as their child’s health which can cause early delivery of a premature baby [2].
PPD is caused by a combination of physical, emotional, psychological and chemical factors. After childbirth, the levels of estrogen and progesterone in the mother instantly drop leading to a chemical change in the brain that may trigger mood swings. Consequently, sleep deprivation also leads to physical distress and tiredness which can trigger other symptoms as well [1].
Neglecting depression as an illness
Illness
An unhealthy condition of body or mind [21]. A healthy proportion of people among the world do not believe postpartum depression or depression as a whole an illness. The status of women in most developing countries is inferior to others, Hence postpartum depression is not taken as a serious issue by the male dominated society of the third world countries.
Difference in social status: There is a persistent flaw existing in the majority of the developing countries as to the social status of women is considered as inferior to that of males and majority of the time their problems are ignored or they don’t have enough courage to speak up of their issues as apart from suffering from depression they feel occurring in postnatal women was conducted on Nigerian and Ethiopian women proved socioeconomic factors play a pivotal role in causing them [22].a sense of inferiority or expect non-seriousness attitude concerning their problem. A study for Common Mental Disorders
Financial status: Poor financial status compels people to ignore postnatal depression as a serious problem. Added to the mental suffering, untreated maternal depression is associated with adverse public health and social consequences for both mother and child. Maternal depression is disabling, leading to a reduced ability to function and work [23]. Suicide is expected to soon become the leading cause of maternal mortality in some low and middle income countries [24] in line with the situation in high income countries [25].
Poor care of child: Postnatal depression occurs after the birth of a child and affects the parents and neglecting such an enormous illness affects not only the parent’s mental health but also impacts the physical health of the baby as the newly born requires complete attention for not only proper growth but also impacts its survival. The child death in the cohort was 42.1 children per 1000 persons, and maternal depression is associated with child death. The risk of child death increases when maternal depression is combined with physical and emotional violence, showing a synergistic interaction [26].
Risk Factors: Postpartum does not occur without cause and some of the factors that have been identified are mentioned as follows:
Marital Status: Marital life impacts a lot on the development and progression of postpartum depression. Studies have found that single mothers are twice as likely to develop postpartum depression as compared to their married counterparts [27]. Men and women having a poor martial relationship suffer PPD more than couples with healthy marital relationship [30].
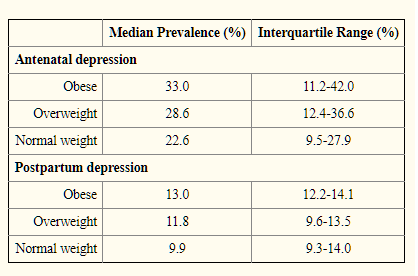
Obesity in relation to PPD: Gain of weight after child birth is common but there is a tendency of females to develop neurological diseases because of their weight. Weight gain in the postpartum period is usually due to over calorie intake as a part of the diet they were taking during pregnancy and sleep deprivation. It is seen increase in BMI increases chances of developing postpartum depression [28]. Studies show Pre-pregnancy obesity prevalence continues to increase and varies by race-ethnicity and maternal age. These findings highlight the need to address obesity as a key component of preconception care, particularly among high-risk groups [29].
Hormonal Changes: There is a major fluctuation in the hormone of woman who had just given birth. progesterone, estrogen, prolactin, cortisol, oxytocin, thyroid, and vasopressin are the most affected hormones and are the most suspected hormones in the causing of Postpartum depression [30]. Postpartum women had a significantly greater level of cortisol, prolactin, thyroxine and oestrogen than non-puerperal women and women suffering from PPD are seen with a significantly low level of prolactin and high levels of progesterone [19].
Complications of Postpartum Depression
Effects of postpartum depression can cause long-term negative outcomes including mental, emotional and behavioral problems.
Effects of postpartum depression can cause long-term negative outcomes including mental, emotional and behavioral problems.
Early Mother-Infant Interactions
According to researchers, disturbed early interactions disturbances. The interaction disturbances in depressed mothers and their infants are present universally in different cultures and socioeconomic status groups [7]. Depressed mothers have two ways of interacting with their children including an invasive and dominant way and an apathetic and inactive way [8]. Depressed mothers touch their kids less frequently as compared to non-depressed mothers and they touch in a more negative way like roughly pulling or poking them. That is why infants of depressed mothers spend more time touching their own skin [9]. The infants of depressed mothers also show poor cognitive-linguistic functioning [20]. The mother’s ability to co-ordinate her vocal behavior with the infant is also affected. So all the early interactive activities between the mother and infant later affect the social, mental and physical development of the infant.
According to researchers, disturbed early interactions disturbances. The interaction disturbances in depressed mothers and their infants are present universally in different cultures and socioeconomic status groups [7]. Depressed mothers have two ways of interacting with their children including an invasive and dominant way and an apathetic and inactive way [8]. Depressed mothers touch their kids less frequently as compared to non-depressed mothers and they touch in a more negative way like roughly pulling or poking them. That is why infants of depressed mothers spend more time touching their own skin [9]. The infants of depressed mothers also show poor cognitive-linguistic functioning [20]. The mother’s ability to co-ordinate her vocal behavior with the infant is also affected. So all the early interactive activities between the mother and infant later affect the social, mental and physical development of the infant.
Inadequate Caregiving Practices
Some caregiving practices are jeopardized by the effects of postpartum depression but they are less important than early mother-infant interaction.
Some caregiving practices are jeopardized by the effects of postpartum depression but they are less important than early mother-infant interaction.
Breast Feeding
Most studies on parenting have showed decrease in breastfeeding for mothers who are going through postpartum depression. Mothers with high levels of depression are most likely to stop breastfeeding at 4 to 16 weeks postpartum and have replaced it with juice or water at that time period which can lead to feeding difficulties in infants [10]. Mothers were also not satisfied with breastfeeding and experienced problems relating to it as well as low levels of efficiency [31]. In one study, breastfeeding was not affected by depression [32].
Most studies on parenting have showed decrease in breastfeeding for mothers who are going through postpartum depression. Mothers with high levels of depression are most likely to stop breastfeeding at 4 to 16 weeks postpartum and have replaced it with juice or water at that time period which can lead to feeding difficulties in infants [10]. Mothers were also not satisfied with breastfeeding and experienced problems relating to it as well as low levels of efficiency [31]. In one study, breastfeeding was not affected by depression [32].
Sleeping Problems
Sleeping problems are also associated with maternal depression which includes placing the baby in prone position instead of the normal supine position, the infant sleeping in its parents’ bed, being nursed to sleep and not sleeping for longer periods of time [33]. These sleeping problems increase when the severity of depression increases. The infant’s sleeping problems may cause sleep deprivation in mothers with consistent feeling of tiredness. Mothers who have infant sleep problems have poor physical and mental health as compared to mothers who do not.
Sleeping problems are also associated with maternal depression which includes placing the baby in prone position instead of the normal supine position, the infant sleeping in its parents’ bed, being nursed to sleep and not sleeping for longer periods of time [33]. These sleeping problems increase when the severity of depression increases. The infant’s sleeping problems may cause sleep deprivation in mothers with consistent feeling of tiredness. Mothers who have infant sleep problems have poor physical and mental health as compared to mothers who do not.
Healthcare
Maternal depressive symptoms also affect the child’s health. A study has shown that infants with depressed mothers had received less preventive measures including age-appropriate well-child visits and up to date vaccinations [34].
Maternal depressive symptoms also affect the child’s health. A study has shown that infants with depressed mothers had received less preventive measures including age-appropriate well-child visits and up to date vaccinations [34].
Safety Practices
Safety practices are also affected by maternal depression. Safety measures like using a car seat, lowering the temperature of water heater, keeping sharp objects and medicines in a safe place and using smoke alarms are usually not seen in mothers with depressive symptoms at 2-4 months [10].
Safety practices are also affected by maternal depression. Safety measures like using a car seat, lowering the temperature of water heater, keeping sharp objects and medicines in a safe place and using smoke alarms are usually not seen in mothers with depressive symptoms at 2-4 months [10].
Suicidal Thoughts
Postpartum depression may also cause mothers to have suicidal thoughts. This usually occurs when the mother is not prepared and ready for having a child. These mothers are anxious, mentally confused and have low self-esteem. Family’s support is needed to get through this situation.
Postpartum depression may also cause mothers to have suicidal thoughts. This usually occurs when the mother is not prepared and ready for having a child. These mothers are anxious, mentally confused and have low self-esteem. Family’s support is needed to get through this situation.
Thoughts of Harming Infant
Thoughts of harming the infant are usually present in depressed mothers. A study showed that more than half of the depressed mothers had a problem with having negative thoughts about the infant and they were afraid of being alone with their kid [35].
Thoughts of harming the infant are usually present in depressed mothers. A study showed that more than half of the depressed mothers had a problem with having negative thoughts about the infant and they were afraid of being alone with their kid [35].
Punishments
Mothers with depressive symptoms are seen to be more bitter and rude towards the infant than non-depressive mothers. These mothers usually deal with their infants harshly by slapping or spanking them more often [10].
Mothers with depressive symptoms are seen to be more bitter and rude towards the infant than non-depressive mothers. These mothers usually deal with their infants harshly by slapping or spanking them more often [10].
Cognitive Performance In Infant
By investigating different sources, some effects of postpartum depression have been seen on the cognitive development of children, mainly boys, such as language, IQ level and behavioral problems. So, this review indicates that postpartum depression can lead to reduced cognitive performance in children by impairing maternal mental health.
By investigating different sources, some effects of postpartum depression have been seen on the cognitive development of children, mainly boys, such as language, IQ level and behavioral problems. So, this review indicates that postpartum depression can lead to reduced cognitive performance in children by impairing maternal mental health.
Paternal Depression
Postnatal depression does not only influence the psychological health and wellbeing of fathers but it also affects the mothers and children as well [4]. Symptoms of PPD are less commonly studied and evaluated in males than in females. Recent studies have showed that father’s psychology may have long-term effects on the child’s mental and behavioral development independently of mother’s psychology. More research is required on factors associated with paternal depression [3].
Postnatal depression does not only influence the psychological health and wellbeing of fathers but it also affects the mothers and children as well [4]. Symptoms of PPD are less commonly studied and evaluated in males than in females. Recent studies have showed that father’s psychology may have long-term effects on the child’s mental and behavioral development independently of mother’s psychology. More research is required on factors associated with paternal depression [3].
Cure of postnatal or postpartum depression:
Postpartum depression can be treated by three different therapies
Postpartum depression can be treated by three different therapies
- Interpersonal therapy
- Cognitive Behavioral Therapy
- Antidepressants
Postpartum depression is usually nit treated with medication because it is relatively contraindicated in breastfeeding mothers.
1. Interpersonal Therapy (IPT): IPT mostly focuses on the effects of depression and is a potentially useful tool for the cure of postpartum depression .IPT is time limited interpersonally oriented psychotherapy that has been demonstrated to be really effective in Postpartum depression .IPT is used to treat acute attacks of depression as well as long term measures to prevent depression. It has proved to be superior than placebo medicine. It is used as a primary treatment and adjunct to antidepressant medicine in preventing relapse in patients. IPT is designed to treat depression by helping patients to focus on four different interpersonal problem areas:
1. Interpersonal Therapy (IPT): IPT mostly focuses on the effects of depression and is a potentially useful tool for the cure of postpartum depression .IPT is time limited interpersonally oriented psychotherapy that has been demonstrated to be really effective in Postpartum depression .IPT is used to treat acute attacks of depression as well as long term measures to prevent depression. It has proved to be superior than placebo medicine. It is used as a primary treatment and adjunct to antidepressant medicine in preventing relapse in patients. IPT is designed to treat depression by helping patients to focus on four different interpersonal problem areas:
- Role transitions
- Interpersonal disputes
- Grief
- Interpersonal deficits
After completion of an initial assessment therapist and patient collaborate to choose a specific problem area and start working on it. Because it’s a short term therapy, it’s only possible to cover a limited number of issues while the treatment is going on. It should be made clear that IPT for postpartum depression is not a “MIRACLE CURE” but it is a method through which skills can be taught that reduce recovery and also decrease the likelihood of relapse [12].
2. Cognitive Behavioral Therapy: CBT is as a talking therapy that can help manage problems by changing the way of thinking and behavior of an individual. It is specifically used for the treatment of postnatal depression. The patient will usually have a session with the therapist once a week or once every two weeks. The duration of the course of treatment usually lasts for 5-20 sessions and each session is of approximately 30-60 minutes [14].There are CBT based support groups that help alleviate postpartum depression and also teach long term coping strategies. It also helps a woman to recognize the relationship between behavior and thoughts [15].
3. Antidepressants: Antidepressants are recommended in cases of moderate to severe depression and if the patient does not want to try psychological treatment or if psychological treatment does not help. The main target of antidepressants are certain chemicals in the brain which help balance the mood of the patient. They help to ease the symptoms like low mood, irritability, lack of concentration and sleepiness allowing the patient to function like a normal individual and also helps the patient to cope better with the new born [14]. Combination of IPT and Imipramine has shown significantly more benefit than antidepressant alone [12]. It is better than placebo medicine. The Royal College of psychiatrists estimated that 50% -60% of people treated with antidepressant see a better improvement as compared to 25%-30% of those taking placebo [14]. Many new antidepressants have fewer side effects as compared to the old ones but each targets a different type of brain chemical so some of them work better for certain people than others.
New Antidepressants:
- Bupropion (Wellbutrin)
- Paroxetine (Paxil, pexeva)
- Fluoxetine (lexapo)
- Sertraline (Zoloft)
Old Antidepressants:
- Amitriptyline (Elavil)
- Desipramine (Norpramin)
- Doxepin (Deptran, sinequan)
- Tranylcypromine (Parnate)
- Trimipramine (surmontile) [16].
Antidepressant Use during Pregnancy and Breast feeding
Taking antidepressants during pregnancy has many potential hazards. Many researchers say that they increase the risk of birth defects.
Taking antidepressants during pregnancy has many potential hazards. Many researchers say that they increase the risk of birth defects.
In Utero Exposure: While a mother is pregnant medicines are transferred to the baby via placenta and amniotic fluid.
Exposure via Breast Milk: Infants are also exposed to maternal antidepressants via breast milk but the amount of medicine exposed is less than in utero exposure. Compared with other antidepressants fluoxetine was more likely to produce effects [17].
Specific techniques: The most common and specific treatment is psychoeducation. The therapist provides information about the nature and cure of postnatal depression as well as child development and care [12].
Conclusion
Postpartum depression or postnatal depression is a type of mood disorder related with child birth which can effect both male and female. Most common symptoms include extreme sadness, crying episodes, low energy, irritability and change in eating and sleeping patterns [11]. PND has a high degree of morbidity and its incidence is 7%-16% of child bearing women .DSM-IV has categorized it as a major type of depression [12]. It is a universal condition with more or less same rate in all countries [18].Psychological techniques are used for the cure of this type of depression cause medicines especially antidepressants effect the health and birth of the baby [12].
References
- Epifanio MS., et al. “Paternal and maternal transition to parenthood: The risk of postpartum depression and parenting stress”. Pediatric Reports 7.2 (2015): 1-19.
- Fiorelli M., et al. “Magnetic resonance imaging studies of postpartum depression: An overview”. Behavioural Neurology (2015): 1-16.
- Luoma I., et al. “Fathers’ postnatal depressive and anxiety symptoms: An exploration of links with paternal, maternal, infant and family factors”. Nordic Journal of Psychiatry 67.6 (2013): 407-413.
- Suto M., et al. “Prevalence and factors associated with postpartum depression in fathers: A regional, longitudinal study in Japan”. Research in Nursing & Health 39.4 (2016): 253-262.
- Beardslee WR., et al. “Children of affectively ill parents: a review of the past 10 years". Journal of the American Academy of Child and Adolescent Psychiatry 37.11 (1998): 1134-1141.
- Lovejoy MC ., et al. Maternal depression and parenting behavior: a meta-analytic review. Clinical Psychology Review 20.5 (2000): 561–592.
- Field T. “Prenatal depression effects on the fetus and neonate”. Emotional Development (2006): 317–339.
- Malphurs JE., et al. “Touch by intrusive and withdrawn mothers with depressive symptoms”. Early Development and Parenting 5 (1996): 111-115.
- Ferber SG., et al. “The development of maternal touch across the first year of life”. Early Human Development 84.6 (2008): 363–370.
- McLearn KT., et al. “Maternal depressive symptoms at 2 to 4 months postpartum and early parenting practices”. Archives of Pediatric & Adolescent Medicine 160 (2006): 279–284.
- https://www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617
- “Interpersonal Psychotherapy for postpartum Depression”. The Journal of Psychotherapy Practice and Research 4 (1995): 18-29.
- Treatment of Postpartum Depression Cooper, P.J,Marry, L. and Halligan,S.S.
- Treatment of Pospartum Depression. In: Tremblay ,R., Barr,R., Peters,R.and Boivin,M.(eds) Encyclopedia on Early Childhood Development. Center of Excellance for Early Childhood Development, Montreal, Quebec (2010).
- https://www.nhs.uk/conditions/cognitive-behavioural-therapy-cbt/
- https://www.nursingtimes.net/clinical-archive/womens-health/cbt-based-support-groups-for-postnatal-depression/5064218.article
- https://www.webmd.com/depression/postpartum-depression/postpartum-depression-antidepressants
- http://www.infantrisk.com/content/antideprassant-usage-during-pregnancy-and-breastfeeding
- “Transcultural Study of Postnatal Depression TCS-PND) Development and Testing of Harmonized Research Methods”. The British Journal of Psychiatry 184.46 (2004): pp.s10.s16
- Abou-Saleh., et al. "Hormonal aspects of postpartum depression." Psychoneuroendocrinology 23.5 (1998): 465-475.
- NICHD Early Child Care Research Network. “Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months”. Developmental Psychology 35.5 (1999): 1297–1310.
- https://www.merriam-webster.com/dictionary/illness
- Hanlon C., et al. “Sociocultural practices in Ethiopia: Association with onset and persistence of postnatal common mental disorders”. British Journal of Psychiatry 197.6 (2010): 468-475.
- Rahman A., et al. “Impact of maternal depression on infant nutritional status and illness: a cohort study”. Archives of General Psychiatry 61.9 (2004): 946-52.
- Patel V., et al. “Suicide mortality in India: a nationally representative survey”. The Lancet 379.9834 (2012): 2343-51.
- “Charlotte Hanlon International Health” 5.1 (2013): 4–5.
- Deyessa N., et al. “Joint effect of maternal depression and intimate partner violence on increased risk of child death in rural Ethiopia”. Archives of Disease in Childhood 95.10 (2010): 771-775.
- McCoy Sarah J., et al. "Risk factors for postpartum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature." The Journal of the American Osteopathic Association 106.4 (2006): 193-198.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4254698/
- Fisher S., et al. “Is Obesity Still Increasing among Pregnant Women? Prepregnancy Obesity Trends in 20 States, 2003-2009”. Preventive Medicine 56.6 (2013): 372–378.
- Collingwood, Jane. "Risk factors for postpartum depression." Psych Centeral (2010).
- Dennis CL and McQueen K. “Does maternal postpartum depressive symptomatology influence infant feeding outcomes?” Acta Paediatrica 96.4 (2007): 590– 594.
- McCarter-Spaulding D and Horowitz JA. “How does postpartum depression affect breastfeeding?” The American Journal of Maternal Child Nursing 32.1 (2007): 10–17.
- Hiscock H and Wake M. “Infant sleep problems and postnatal depression: a community-based study”. Pediatrics 107.6 (2001): 1317–1322.
- Minkovitz CS., et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics 115.2 (2005): 306–314.
- Jennings KD., et al. “Thought of harming infants in depressed and nondepressed mothers”. Journal of Affective Disorders 54.1-2 (1999): 21–28.
Citation:
Ali Mustufa., et al. “Review on Prevalence, Ignorance and Seriousness of Postpartum Depression in Developing Countries”. Clinical Biotechnology and Microbiology 3.1 (2018): 587-593.
Copyright: © 2018 Ali Mustufa., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.