Case Report
Volume 2 Issue 3 - 2018
Accidental Discovery of Enterouterine Fistula in a Woman with Secondary Amenorrhoea
1Department of Radiology, Federal Medical Centre, Owerri
2Department of obstetrics and Gynaecology, Imo State University Teaching Hospital, Orlu
3Department of Obstetrics and Gynaecology, Federal Medical Centre, Owerri
2Department of obstetrics and Gynaecology, Imo State University Teaching Hospital, Orlu
3Department of Obstetrics and Gynaecology, Federal Medical Centre, Owerri
*Corresponding Author: Dr Chijoke Okeudo, Department of obstetrics and Gynaecology, Imo State University Teaching Hospital, Orlu.
Received: June 03, 2018; Published: July 03, 2018
Abstract
Enterouterine fistula is a very rare form of genital tract fistula and a rare complication of myomectomy whose diagnosis requires a high index of suspicion and an experienced radiologist. It is also an infrequent cause of secondary amenorrhoea.
Keyword: Post-myomectomy; Secondary Amenorrhoea; Enterouterine fistula
Introduction
A fistula is an abnormal connection between two epithelium-lined organs or vessels that do not connect. In the case of the uterus, fistulas can develop to the bladder, skin, colon, and small intestine, resulting in vesico-uterine, uterocutaneous and enterouterine fistulas [1]. Enterouterine fistulas occur infrequently. It may result from obstetric complications from caesarean section, forceps-aided delivery, external cephalic version, dilatation and curettage (D&C) for removal of placenta, perforation of an intra-uterine device, inflammatory bowel disease like Crohn’s disease, pelvic malignancy, pelvic radiation therapy, pelvic surgery from myomectomy or appendicectomy, iatrogenic causes or trauma [2].
A rare case of enterouterine fistula in a patient after myomectomy is reported. The fistula caused no symptoms and was accidentally discovered at hysterosalpingography (HSG) for secondary amenorrhoea.
Case Report
Mrs N.I. was a 40-year-old Para 1+0 (alive 1) woman presented to the Radiology Department of Federal Medical Centre, Owerri, for hysterosalpingography (HSG) as a routine work-up for secondary amenorrhoea. She presented with history of absence of menstruation of 4 months duration. Prior to the onset of her symptoms, she had been having regular 28 day cycle with 5 days of normal menstrual flow since menarche. There was no history of vaginal discharge or lower abdominal pain. No history suggestive of pregnancy nor termination of pregnancy and not on hormonal medication. She had an uneventful myomectomy 6 months prior to presentation. She resumed her normal menses for two months after the surgery, before it ceased. Other histories were not contributory.
Physical examination revealed a healthy looking woman, not pale, afebrile and in no painful distress. Abdominal examination revealed a Pfannenstiel incision scar of about 10 cm in length. Other systemic examinations were essentially normal.
Investigations done included high vaginal swab and endocervical swab for microscopy, culture and sensitivity, which yielded no bacterial growth after 24 hours of incubation. Hormone profile values were within normal range. She was subsequently referred to the Radiology Department for pelvic ultrasound scan and HSG.
Pelvic ultrasound scan did not show any abnormality. HSG revealed an abnormally shaped uterine cavity, which was narrow, suggestive of uterine/cervical synechia. The fallopian tubes were not demonstrated but free peritoneal spillage of contrast was seen on the right side of the pelvic cavity. Contrast-opacified small bowel loops were noted on the left side of the abdomen (Figure 1 and Figure 2). Diagnosis of enterouterine fistula with uterine/cervical synechia was made. Following this observation, further information was sought from the patient. She admitted to have subsequently noticed that her stools appeared darker than usual cyclically, since her menses ceased.
At surgery (involving General Surgeon and Gynaecologist), the jejunum was found to be adherent to the posterior wall of the uterus. Their separation showed the fistula of about 2 cm in diameter between the jejunum and posterior wall of the uterus. The tract was excised along with resection of a small segment of the jejunum followed by re-anastomosis of the jejunal loop. The tract on the uterus was also excised and the defect closed. The internal Os was dilated with Hegar dilator to relieve the cervical stenosis. Postoperative period was uneventful. She was discharged from the hospital on the 7th post-operative day she made a return visit one month later. She had no complaints and had also resumed her normal menses. She however declined a repeat HSG since her menses had resumed.
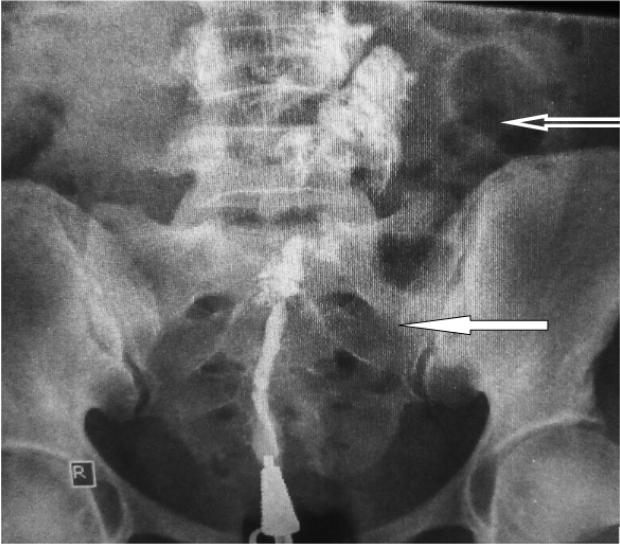
Figure 1: Hysterosalpingogram showing the abnormally shaped uterine cavity (white
arrow) and contrast outlining a short segment of bowel loop (white open arrow) in
the same investigation. The uterine cavity is narrow, suggestive of uterine synechia.
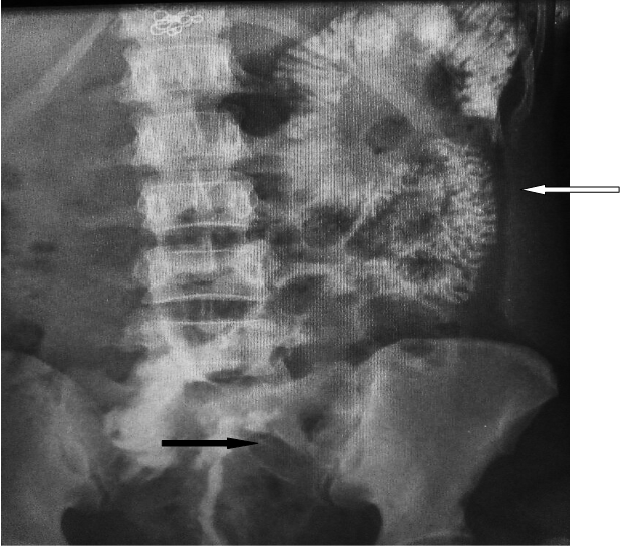
Figure 2: Hysterosalpingogram showing the abnormally shaped uterine cavity (black
arrow) and progressive increase in small bowel loop opacification (white arrow).
Discussion
Enterouterine fistula is a rare form of communication between the gastrointestinal and genital tracts [3]. Martin., et al. [4] published a review of 80 cases of enterouterine fistulas. Out of these, 42 followed obstetric injury, 17 resulted from inflammatory processes, 12 following curettage and 9 related to carcinoma, non-resulted from a previous myomectomy.
In cases where pelvic malignancy is a cause of enterouterine fistula, endometrial carcinoma is the most common cause [4]. Although the rate of myomectomy in Nigeria for management of fibroid is between 15.8% and 86%, the development of enterouterine fistula as a complication is rarely reported [5]. The index patient developed enterouterine fistula after myomectomy. The ileum and the sigmoid colon are the most commonly injured portions of the bowel due to their anatomic locations [6], however it was the jejunum that was involved in the index case. This could be explained by the different aetiology in our case.
The clinical presentation of enterouterine fistula depends on the size and location. Small fistulae may be asymptomatic and are discovered incidentally during investigation of other conditions, just like the index case, that was discovered during HSG. The eventual history of cyclical passage of dark stools made the managing team to think of reverse flow of menstrual blood through the fistulous tract in the presence of cervical stenosis.
Ultrasound scan (US), HSG, computed tomography (CT) and magnetic resonance imaging (MRI) all contribute in the diagnosis of enterouterine fistula. US is usually the first line investigation because of its accessibility, affordability and non-involvement of ionizing radiation. US findings may be normal, just like in the index patient. A transvaginal US may show fluid collection within the endometrial cavity. Sonohysterography using contrast medium could be used to visualise not only the fistula tract but also the uterine wall and the bowel loop [7]. HSG is useful in outlining the characteristics of the fistula and may be the investigation of choice in the majority of cases. Contrast may be seen passing through the fistula from the uterine cavity to the lumen of the bowel loop. Cross-sectional imaging with CT and MRI may be necessary to demonstrate subtle features in the anatomy of the fistula, including the course of the tract and extra-luminal disease, including associated abscesses, tumour, or other coexisting processes that may be missed with contrast studies. [8] Such information is useful for patient management and planning for surgical repair.
Management of enterouterine fistula has traditionally been surgical involving resection of the fistula tract and involved structures followed by primary re-anastomosis. Józwik [9] suggested that endometrium in the fistulous tract may be amenable to hormonal regulation and therefore conservative treatment.
This patient had surgery with resection of the fistula tract and primary re-anastomosis of the bowel loops and closure of the defect in the posterior uterine wall.
Conclusion
This rare condition has been presented to alert Gynaecologists to the possibility that enterouterine fistula may be a rare and unsuspected complication of myomectomy and cause of secondary amenorrhoea.
Sources of Funding: The research was fully funded by the authors.
Contribution of Authors
The authors substantially contributed to:
The authors substantially contributed to:
- Conception and design, acquisition of data and interpretation of data
- Drafting the article and revising it critically for important intellectual content and
- Finally approved the article to be published
References
- Kilinc F., et al. “Unusual case of post-cesarean vesico-uterine fistula”. International Journal of Urology 10 (2003): 236-238.
- Iloabachie GC and Njoku O. “Vesico-uterine fistula”. British Journal of Urology 57 (1985): 438-439.
- McFarlane MEC., et al. “Jejunouterine fistula: a case report”. Gynecological Surgery 5 (2008): 173-175.
- Martin DH., et al. “Enterouterine fistula. Review; report of an unusual case”. Obstetrics & Gynecology 7 (1956): 466-468.
- Akinyemi BO., et al. “Uterine fibroid: a review”. Nigerian Journal of Medicine 13 (2004): 318-329.
- Garg N., et al. “Unsafe abortions-Shearing of the sigmoid and the descending colons”. The Journal of Obstetrics and Gynecology of India 54 (2004): 83-84.
- Takada T., et al. “Preoperative diagnosis of colouterine fistula secondary to diverticulitis by sonohysterography with contrast medium”. Ultrasound Diagnosis in Obstetrics and Gynecology 24 (2004): 682-683.
- Yu NC., et al. “Fistulas of the genitourinary tract: a radiologic review”. RadioGraphics 24 (2004): 1331-1352.
- Józwik M. “Hormonal dependence of fistulas communicating with the uterus”. International Urogynecology Journal - and Pelvic Floor Dysfunction 18 (2007): 719-720.
Citation:
Chijoke Okeudo., et al. “Accidental Discovery of Enterouterine Fistula in a Woman with Secondary Amenorrhoea”. Chronicle
of Medicine and Surgery 2.3 (2018): 173-177.
Copyright: © 2018 Chijoke Okeudo., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.