Review Article
Volume 2 Issue 3 - 2018
Necrotizing Enterocolitis in Infants
1Institute of Molecular Biology and Biotechnology, Bahauddin Zakariya University, Multan, Pakistan
2College of Pharmacy, G.C. University, Faisalabad, Pakistan, Institute of Molecular Biology and Biotechnology, Bahauddin Zakariya University, Multan, Pakistan
2College of Pharmacy, G.C. University, Faisalabad, Pakistan, Institute of Molecular Biology and Biotechnology, Bahauddin Zakariya University, Multan, Pakistan
*Corresponding Author: Muhammad Imran Qadir, Institute of Molecular Biology and Biotechnology, Bahauddin Zakariya University,
Multan, Pakistan.
Received: June 15, 2018; Published: July 04, 2018
Summary
Necrotizing enterocolitis is a medical condition in which necrosis in various parts of bowel takes place. Usually it affects the premature infants and causes abdominal distension, intestinal necrosis and hemorrhage. In necrotizing enterocolitis, the primary risk factor is prematurity and it is the major cause of morbidity and mortality among the newborn babies. Particularly the infants having very low birth weight are more susceptible to NEC. The way of management of infants with NEC is quite different from other neonates. So any infant with symptoms of NEC, needs immediate treatment otherwise it may lead to some severe conditions of this disease. However, prevention is best cure of it because NEC has multifactorial nature in its etiology.
Keyword: Peritonitis; Neutropenia; Pneumoperitoneum; Abdominal distension
Introduction
Necrotizing enterocolitis is a disease of GIT track in which various portions of the bowel undergo necrosis and ultimately cause tissue damage [1]. This disease most probably occurs in premature infants that having no any other disease. Out of one thousand infants, about 2 or 3 are affected by this disease. Treatment of infants with NEC mostly involves bowel rest, gastric decompression, systemic antibiotics and parenteral nutrition. However, prevention from preterm birth and avoidance from milk of donor give great potential benefits [2,3]. The incidence of NEC varies inversely with pregnancy period length, mostly occurs in those infants with less gestational age.
Etiology
Definite cause of necrotizing enterocolitis is still unknown. However, Pseuodomonas aeruginosa is suspected to be a cause of this disease in infants [4-6]. Many other causes of necrotizing enterocolitis include poor immune system, intestinal flora, prolonged use of antibiotics and oral feeding other than the breast milk of the mother. It is proposed that oral feeding in infants increases the risk of necrotizing enterocolitis ten times greater than the infants that having feed from the mother directly. [7,8] Its reason is that the breast milk of the mother has anti-infective property that prevents the infants against certain diseases. [9]
Definite cause of necrotizing enterocolitis is still unknown. However, Pseuodomonas aeruginosa is suspected to be a cause of this disease in infants [4-6]. Many other causes of necrotizing enterocolitis include poor immune system, intestinal flora, prolonged use of antibiotics and oral feeding other than the breast milk of the mother. It is proposed that oral feeding in infants increases the risk of necrotizing enterocolitis ten times greater than the infants that having feed from the mother directly. [7,8] Its reason is that the breast milk of the mother has anti-infective property that prevents the infants against certain diseases. [9]
Pathophysiology
As the causative agent of necrotizing enterocolitis is not confirmed, so, its pathogenesis is also not exactly known. [10-12] However,
As the causative agent of necrotizing enterocolitis is not confirmed, so, its pathogenesis is also not exactly known. [10-12] However,
- Infants those having intestinal flora like Staphylococcus aureus and E. coli are more susceptible to NEC.
- Long term antibiotic therapy causes the change in the internal environment of the GIT that may lead to necrosis.
- Immature intestinal mucosa may also the cause of NEC.
Sign and Symptoms
Initial symptoms are feeding disturbance, bloody stools due to mucosal damage and abdominal distension. Late symptoms are perforations in the various parts of GIT, peritonitis and hypotension [13,14].
Initial symptoms are feeding disturbance, bloody stools due to mucosal damage and abdominal distension. Late symptoms are perforations in the various parts of GIT, peritonitis and hypotension [13,14].
Diagnosis
Necrotizing enterocolitis is diagnosed clinically but it also requires certain imaging techniques to confirm the disease like radiography, ultrasonography, etc. radiographic signs in infant having NEC are expansion of bowel loop (due to filling of gas) and pneumoperitoneum (free air outside the bowel within the abdomen) [15,16]. Ultrasonography also proves an effective technique in the diagnosis of NEC. Mostly abdominal distension, intestinal necrosis and hemorrhage like symptoms are seen in case of necrotizing enterocolitis in infants [17].
Necrotizing enterocolitis is diagnosed clinically but it also requires certain imaging techniques to confirm the disease like radiography, ultrasonography, etc. radiographic signs in infant having NEC are expansion of bowel loop (due to filling of gas) and pneumoperitoneum (free air outside the bowel within the abdomen) [15,16]. Ultrasonography also proves an effective technique in the diagnosis of NEC. Mostly abdominal distension, intestinal necrosis and hemorrhage like symptoms are seen in case of necrotizing enterocolitis in infants [17].
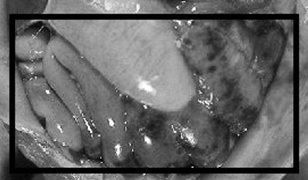
Figure 1: Gross pathology of neonatal necrotizing enterocolitis.
Autopsy of infant showing abdominal distension, intestinal necrosis
and hemorrhage and peritonitis due to perforation.
[Modified from https://phil.cdc.gov/Details.aspx?pid=855]
[Modified from https://phil.cdc.gov/Details.aspx?pid=855]
Treatment
Surgical treatment of NEC is possible but it may cause certain complications like short bowel syndrome and suppression in neural development. During surgery dead bowel contents are removed from the body [18-20]. Rather than the treatment, preventive measures are very useful to minimize the risk of NEC. Prevention is the best cure of NEC because there is many causes of getting NEC in infants, in other words NEC has multifactorial nature regarding its etiology [21,22].
Surgical treatment of NEC is possible but it may cause certain complications like short bowel syndrome and suppression in neural development. During surgery dead bowel contents are removed from the body [18-20]. Rather than the treatment, preventive measures are very useful to minimize the risk of NEC. Prevention is the best cure of NEC because there is many causes of getting NEC in infants, in other words NEC has multifactorial nature regarding its etiology [21,22].
Prevention
These include
These include
- Minimize oral feeding.
- Stoppage of antibiotic therapy
- Use only human milk or milk from donor if mother's milk is unavailable.
- Recent study shows that the use of higher rate of lipid infusion in the first week of life resulted in no infant with NEC [23].
References
- Reber KM and Nankervis CA. “Necrotizing enterocolitis preventative strategies”. Clinics in Perinatology 31.1 (2004): 157-167.
- Caplan MS. “Pathogenesis and Prevention of Neonatal Necrotizing Enterocolitis”. Fetal and Neonatal Physiology (2004).
- Stoll BJ. “Epidemiology of Necrotizing Enterocolitis”. Clinics in perinatology 21.2 (1994): 205-218.
- Kanto WP., et al. “Recognition and Medical management of necrotizing enterocolitis”. Clinics in Perinatology 21.2 (2000): 335-346.
- Morrison SC and Jacobson JM. “The radiology of necrotizing enterocolitis”. Clinics in Perinatology 21.2 (2004): 347-364.
- Bell MJ., et al. “Neonatal necrotizing enterocolitis. Therapeutic decision based upon clinical staging”. Annals of Surgery 187 (2001): 1-7.
- Sato TT and Oldham KT. “Abdominal drain placement versus laparotomy for necrotizing enterocolitis with perforation”. Clinics in Perinatology 31.3 (2004): 577-589.
- Sharma R., et al. “Portal venous gas and surgical outcome of neonatal necrotizing enterocolitis”. Journal of Pediatric Surgery 40.2 (2005): 371-376.
- Hintz SR., et al. “NICHD Neonatal Research Network. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis”. Pediatrics 115.5 (2005): 696-703.
- Rees CM., et al. “Surgical strategies for necrotising enterocolitis: a survey of practice in the United Kingdom”. Archives of Disease in Childhood. Fetal and Neonatal Edition 90.2 (2005): F152-F155.
- Lin HC., et al. “Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants”. Pediatrics 115.1 (2005): 1-4.
- Hsueh W., et al. “Neonatal necrotizing enterocolitis: clinical considerations and pathogenetic concepts”. Pediatric and Developmental Pathology 6.1 (2003): 6-23.
- Amin HJ., et al. “Arginine supplementation prevents necrotizing enterocolitis in the premature infant”. Journal of Pediatrics 140.2 (2002): 425-431.
- Reber KM., et al. “Newborn intestinal circulation. Physiology and pathophysiology”. Clinics in Perinatology 29 (2002): 23-39.
- Lin HC., et al. “Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants”. Pediatrics 115 (2005): 1-4.
- Dani C., et al. “Probiotics feeding in prevention of urinary track infection, bacterial sepsis and necrotizing enterocolitis in preterm infants. A prospective double blind study”. Biology of the Neonate 82 (2002): 103-108.
- Lucas A and Cole TJ. “Breastmilk neonatalnecrotizing enterocolitis”. Lancet 336 (1990): 1519-1523.
- Schanler RJ., et al. “Feeding strategies for premature infants: beneficial outcomes of feeding fortified human milk versus preterm formula”. Pediatrics 103 (1999): 1150-1157.
- Eibl MM., et al. “Prevention of necrotizing enterocolitis in low birth weight infants by IgA-IgGn feeding”. The New England Journal of Medicine 319 (1998): 1-7.
- Rubaltelli FF., et al. “Prevention of necrotizing enterocolitis in neonates at risk by oral administration of monomeric IgG”. Developmental Pharmacology and Therapeutics17 (1991): 138-143.
- Lawrence G., et al. “Enteral human IgG for prevention of necrotizing enterocolitis: a placebo controlled, randomized trial”. Lancet 357 (2001): 2090-2094.
- Orrhage K and Nord CE. “Factors controlling the bacterial colonization of the intestine in breastfed infants”. Acta Paediatrica 88 (1999): 47-57.
- Thompson C., et al. “Lactobacillus acidophilus sepsis in a neonate”. Journal of Perinatology 21 (2001): 288-260.
Citation:
Muhammad Imran Qadir and Muhammad Usman. “Necrotizing Enterocolitis in Infants”. Chronicle of Medicine and Surgery
2.3 (2018): 178-181.
Copyright: © 2018 Muhammad Imran Qadir and Muhammad Usman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.