Case Report
Volume 2 Issue 2 - 2018
A Rare Case of Bobble Head Doll Syndrome
Department of Neurosurgery, University of Zimbabwe, Harare, Zimbabwe
*Corresponding Author: Nathaniel Zimani, Department of Neurosurgery, University of Zimbabwe, Harare, Zimbabwe.
Received: February 19, 2018; Published: March 07, 2018
Abstract
Bobble-head doll syndrome is a rare and surgically treatable movement disorder characterized by up-and-down (yes-yes) head bobbing occurring at a rate of 2-3 Hz. Side-to-side (no-no) head bobbing is less frequently described. It is usually associated with cystic abnormalities in the region of the anterior third ventricle. Various physiologic mechanisms have been proposed but none of them has been substantiated. We report a patient with this syndrome due to a suprasellar arachnoid cyst, a six year old female patient who presented with a rare movement disorder called bobble head doll syndrome which was treated surgically. This case report seeks to highlight this treatable movement disorder and treatment options available for its cure.
Keywords: Bobble Head Doll; Third Ventricle; Suprasellar Arachnoid Cyst; Ataxia
Introduction
Bobble head doll syndrome is a rare and unique movement disorder encountered in children. It was first described in 1966 by Benton., et al. It is usually associated with expansion of the third ventricle. By the time we noted our case, only 58 cases had been reported, this being the first in Africa. Making it a fairly rare disease hence the need to report it.
Case Report
We report a case of six year old female patient from Harare, a product of an uncomplicated full term pregnancy and spontaneous breech delivery who presented with bobbling of the head plus enlarging of head for two years. This bobbling of the head was worse during the day but at night it would disappear while the patient was asleep. It was noted to be getting worse with time during the two year period. The patient initially was sent to school but had to stop as this was now associated with inability to walk straight, was also noted to have had an enlarging head over the years but the mother is not sure of actual dates. This was not associated with vomiting but was associated with intellectual function as evidenced by teachers at school, having noted a decrease in performance. The patient was otherwise a happy and pleasant child.
She was initially seen by a general practitioner who then referred due to the enlarging head and a diagnosis of mental retardation. The patient was seen in the neurosurgical clinic and had a CT SCAN done (Figure 1 below), at that time she was symptomatic for hydrocephalus with unrelenting headache and then an emergency VP shunt insertion was then done. The patient improved clinically in terms of hydrocephalus but was noted to be getting worse in terms of the bobble head syndrome. A repeated scan showed a migrated shunt (ventricular end). At this time the patient was asymptomatic in terms of hydrocephalus.
On examination pink, happy child, chest was noted to be clear as well as the rest of the examination in general. Patient had bobbling of head which appeared to be of yes-yes type at 2-3 Hz per min. Glasgow coma scale 15/15 with an enlarged head at 2 SD above normal size for age. She had six nerve palsy on the left side and nystagmus horizontal type, left sided hemiparesis with power of 3/5 and an ataxia. The blood test results were unremarkable. CT scan showed a suprasellar arachnoid cyst with dilated ventricles (Figure 1 below).
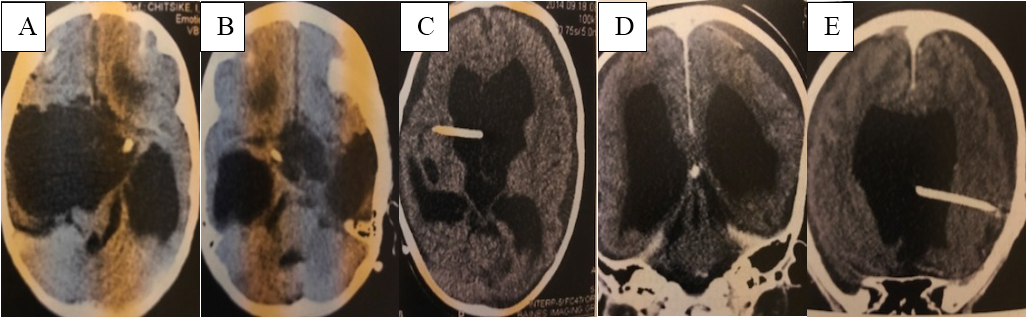
Figure 1: CT scan brain showing arachnoid cyst before and after shunts : A: arachnoid cyst extending to the
lateral part of the cranium; B: arachnoid cyst around the area of the third ventricle; C: post op CT scan showing
shunt in the arachnoid cyst and relief of pressure as compared previously ,but also showing bilateral subdural
collections; D: coronal image showing relief of pressure of the third ventricle ,again the subdural collection can
be seen; E: coronal image showing the shunt in situ in the arachnoid cyst which has collapsed due to the shunt.
The patient was electively taken to theatre and had first the shunt removed (ventricular end) and insertion of a cysto-peritoneal shunt, a medium pressure shunt was used. Post-operative recovery was unremarkable. The patient was reviewed in neurological clinic where the bobbling continued for the first two months unchanged and a repeat scan was done which showed bilateral subdural hematoma which was asymptomatic so patient was observed. At six month follow up patient bobbling had improved remarkably, barely visible, although ataxia was still present. The parents are planning to take the patient to school. At review at 1 year it was noted to have disappeared
Discussion
First described by Benton., et al. in the year 1966 [1], “bobble head doll syndrome (BHDS)” is a rare and an interesting movement disorder characterized by continuous or episodic forward and backward head nodding at times associated with side to side movements of the head of 2-3 Hz frequency [2,3]. These movement disorders are sensitive to sensory stimuli. This might explain why these movements disappear when asleep (for most of the cases) and increase during activities.
Epidemiology is unknown partly due to the rarity of the condition and also might be due to under diagnosis of the disease entity itself. It is found mainly in pediatric population usually under the age of 3 years [4] (youngest in newborn to oldest 26 year old). In the case of our patient ,the late presentation was due to late referral ironically due to wrong diagnosis or better stated due to focus on the other part of disease ie hydrocephalus.
This is believed to be a pathologically based disease. It is presumed that this movement disorder is due to the pressure effect of dilated third ventricle which distorts the dorsomedial red nucleus and dentatorubrothalamic pathways [2,5,6]. In addition there is compression of medial thalamus, the latter having their somatotropic motor representation of head and neck area [5]. The pressure over the medial thalamus leads to head and neck tremors and as the lesion progresses it gives rise to truncal and appendicular tremors also by affecting thalamic area.
It is possible that the back and forth movement of fluid within the cyst causes rhythmic pressure on the diencephalic motor pathways. Attenuation of tremors on volitional activities and their presence at rest suggest a possible role of basal ganglia in the genesis of this disorder. The basal ganglia plays a large part in controlling motor function and thus abnormalities to this system can result in movement disorders such as Parkinson’s Disease and dyskinesia both of which share commonalities with bobble head syndrome [2,5]. It is also suggested that the movement develops as a learned phenomenon as it stops on volitional activities.
This probably helps in improving the CSF circulation ad is supported by the observation of disappearance of head movements and headache on extreme flexion or extension of neck in a case with bobble head syndrome. The main clinical feature is the bobbling of the head as described nodding at times associated with side to side movements of the head of 2-3 Hz frequency [2,4,7 and 8]. At times these movements can be made to disappear when given or made to do tasks and this is better appreciated in the early stages [2,9,10]. In the cases of those with late presentation or large pathologies then this is not appreciated as it is more constant in nature. The bobbling may be accompanied by ataxia [10]. Patients often have obstructed hydrocephalus due to blockage at the level of foreman of Monro, hence might present with large head and other symptoms of hydrocephalus [11].
The main imaging of choice would be an MRI SCAN [2] as it allows for better clarification in terms of structure and the pathology. A CT SCAN is an alternative which can be used. Another test would be to use cisternography. This is used to see CSF flow and might be useful in planning choice of surgery. There is no uniformly agreed upon treatment option for the disease. This is because the most common cause is a suprasellar cyst and hence treatment is dependent on this pathology. Options include shunting cyst, shunting hydrocephalus or both and third ventriculostomy [12,10].
In our case we elected to do a cysto-peritoneal shunt. Its advantage is in the simplicity in doing it and being cost effective. It is also always where possible shunt of the cyst and the hydrocephalus at the same time where three way catheter is available. The disadvantage is similar to all shunts and includes shunt infection, migration and subdural haematoma as in our case not to mention a few. Although the latter may be avoided by using a high pressure shunt. The next would be to do an endoscopic fenestration of the cyst to allow for drainage, others in the same sitting have gone to do ETV [13].
These can be done combination [14]. For some patients just shunting the hydrocephalus has been to shown to help [8]. The best definitive treatment is difficult to say because of sporadic cases and good outcome with either treatment. Not all bobble head syndrome cases will be treated by surgical treatment but in the case follow up it does offer a good outcome.
Conclusion
Bobble head syndrome is a rare movement disorder which has room for surgical treatment with good results in whatever center available. It must be appreciated for it to be treated because it is a treatable life changing disease.
References
- Nellhaus G. “The bobble head doll syndrome: a “tic” with a neuropathologic basis”. Pediatrics 40.2 (1967): 250-253.
- Bhattacharyya KB., et al. “Bobbling head in a young subject”. Annals of Indian Academy of Neurology 17.4 (1988): 371-373.
- Gangemi M. “Hydrocephalus and “bobble head doll” syndrome. A case report”. Acta Neurologica 10.2 (1988): 143-147.
- Bhattacharyya KB., et al. “Bobble head doll syndrome: some atypical features with a new lesion and review of the literature”. Acta Neurologica Scandinavica 108.3 (2003): 216-220.
- Wiese JA., et al. “Bobble Head Doll Syndrome: review of pathophysiology and CSF dynamics”. Pediatric Neurology 1.6 (1985): 361-366.
- Ishihara M., et al. ““No-no” type bobble head doll syndrome in an infant with an arachnoid cyst of the posterior fossa: a case report”. Pediatric Neurology 49.6 (2013): 474-476.
- Hagebeuk EE., et al. “Bobble head doll syndrome successfully treated with an endoscopic ventriculocystocisternostomy. Case report and review of literature”. Journal of Neurosurgery 103 (2005): 253-259.
- De Brito Henriques., et al. “Bobble head doll syndrome associated with DandyWalker syndrome. Case report”. Journal of Neurosurgery 107 (2007): 248-250.
- Deonna T and B Dubey. “Bobble head doll syndrome. Case report with a review on the different types of abnormal head movements in infancy, and their clinical significance”. Helvetica Paediatrica Acta 31.3 (1976): 221-227.
- Fioravanti A., et al. “Bobble head doll syndrome due to Suprasellar arachnoid cyst: endoscopic treatment in two cases”. Child's Nervous System 20.10 (2004): 770-773.
- Zamponi N., et al. “Bobble Head doll syndrome in a child with a third ventricular cyst and hydrocephalus”. Child's Nervous System 21. 5 (2005): 350-354.
- Albright L., “Treatment of bobble head doll syndrome by transcallosal cystectomy”. Neurosurgery 8.5 (1981): 593-595.
- Van Beijnum J., et al. “Navigated laser- assisted endoscopic fenestration of a suprasellar arachnoid cyst in a 2 year old child with bobble head doll syndrome. Case report”. Journal of Neurosurgery 104 (2006): 348-351.
Citation:
Nathaniel Zimani., et al. “A Rare Case of Bobble Head Doll Syndrome”. Current Opinions in Neurological Science 2.2 (2018):
437-440.
Copyright: © 2018 Nathaniel Zimani., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.