Case Report
Volume 2 Issue 3 - 2018
Fourth Ventricle Papilloma and Cranio-Cervical Junction Meningioma: Coincidental Tumors: a Case Report and Review of the Literature
1Associate Professor of Neurosurgery, Tripoli University, Libya
2Associate Professor of Radiology, Tripoli Medical center, Tripoli-Libya
3Neurosurgeon, Ali Omar Askar Neurosurgery Hospital, Tripoli University, Libya
2Associate Professor of Radiology, Tripoli Medical center, Tripoli-Libya
3Neurosurgeon, Ali Omar Askar Neurosurgery Hospital, Tripoli University, Libya
*Corresponding Author: Dr. Muffaq Lashhab, Neurosurgeon, Ali Omar Askar Neurosurgery Hospital, Tripoli University, Libya.
Received: March 22, 2018; Published: April 05, 2018
Abstract
The co-existence presence of meningioma and choroid plexus papilloma is very rare. Few cases of simultaneous tumors at the 4th ventricle described in the literature but there is no a single craniocervical, 4th ventricle combined tumour case reported in the recent neurosurgery literature. The condition is difficult to be diagnosed clinically as there are discrepences between clinical and radiological findings, the best outcome was reached by the simultaneous removal of both tumors. Meningiomas with concurrent papillomas are thought to be different primary brain tumours arising in the same individual at random.
Keywords: Concurrent Intracranial Tumours; Meningioma; Choroid Plexus Papilloma; Ventricular Tumours
Introduction
Choroid plexus papillomas (CPPs) are rare tumors originating from the neuroectoderm, they comprise less than [1]. It has been found that children are the most heavily affected portion of the population (70% of C.C.Ps) with 50% presenting before the second year of life [2]. A very few reports of CPP in adult are present in the literature [2–5].
Skull basal meningioma’s uncommonly affect the foramen magnum. Despite the accelerating advances in imaging modalities, the tumor location and rate of recurrence along with rate of vertebral artery (V.A) encasement and surgical approaches are still open to debate. We report an unusual case of an intraventricular choroid plexus papilloma (CPP) occupying the fourth ventricle occurring together with Cranio-cervical junction meningioma. The clinical presentation, preoperative imaging, surgical treatment and histologic features of the two tumors are discussed.
Case Report
Clinical presentation
This study presents a woman aged 45-year-old complaining of progressive confusion, altered facial sensation, vomiting for 2 months, gait unsteadiness and both L.L weakness. The medical history is insignificant, Neurofibromatosis was excluded. On examination, she had an unsteady, wide.
This study presents a woman aged 45-year-old complaining of progressive confusion, altered facial sensation, vomiting for 2 months, gait unsteadiness and both L.L weakness. The medical history is insignificant, Neurofibromatosis was excluded. On examination, she had an unsteady, wide.
Radiological findings
Brain and craniocervical MRI reveals a well-defined elongated mass measures 44*21 mm with homogenous contrast enhancement which is filling the 4th ventricle, anteriorly it is seen markedly indenting the posterior aspect of the brain stem.
Brain and craniocervical MRI reveals a well-defined elongated mass measures 44*21 mm with homogenous contrast enhancement which is filling the 4th ventricle, anteriorly it is seen markedly indenting the posterior aspect of the brain stem.
It shows also LT SIDES Dural based homogenous contrast enhanced S.O.L at craniocervical junction with homogenous contrast enhancement measures 23*21 mm.Figure (1a, 1b).
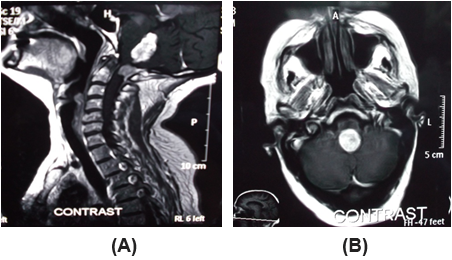
Figure 1: Brain and craniocervical junction preoperative MRI images with contrast
sagittal (a) and axial (b) views, craniocervical junction shows Fourth ventricle papilloma
(red arrow) and Cranio-Cervical junction meningioma(blue arrow).
Surgical intervention
The patient was underwent midline sub-occipital craniotomy. Opening the cistern magna and separating the tonsils to reach the tumours. It was shrunken by coagulation and irrigation and then removed. C1 laminectomy and gross total excision of the meningioma was established.Figure 2
The patient was underwent midline sub-occipital craniotomy. Opening the cistern magna and separating the tonsils to reach the tumours. It was shrunken by coagulation and irrigation and then removed. C1 laminectomy and gross total excision of the meningioma was established.Figure 2
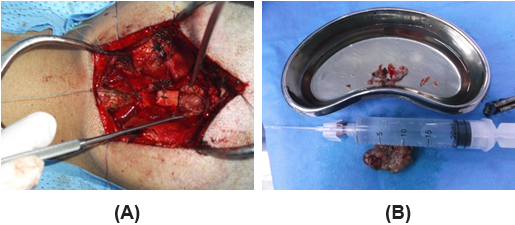
Figure 2: Intraoperative image shows exposed tumor filling the 4th ventricle
(a), (green arrow), and both tumors samples (b), (black arrows).
Pathology
Histopathology revealed a CCJ meningioma’s well as a choroid plexus papilloma.
Histopathology revealed a CCJ meningioma’s well as a choroid plexus papilloma.
Postoperatively
The patient evolution was satisfactory, she was admitted in INTENSIVE CARE UNIT for two days for observation, she was underwent motor rehabilitation with good clinical evolution. It is debatable whether or not to treat C.C.P with post-operative chemotherapy or radiation, therefore we didn't recommend her to do.Figure 3
The patient evolution was satisfactory, she was admitted in INTENSIVE CARE UNIT for two days for observation, she was underwent motor rehabilitation with good clinical evolution. It is debatable whether or not to treat C.C.P with post-operative chemotherapy or radiation, therefore we didn't recommend her to do.Figure 3
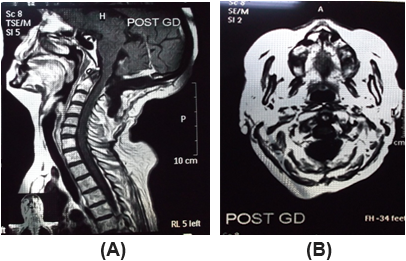
Figure 3: Brain and craniocervical junction postoperative MRI images
with contrast sagittal (a) and axial (b) views at level of craniocervical
junction shows total resection of both tumors. (white arrows).
Discussion
Histopathologically, CCPs are rare benign neoplasma, the origin of which is the choroid plexus epithelium of the 4th ventricle in adults and the lateral ventricles in children are the most common sites. CCP are usually treated by complete microsurgical resection, a surgery which is argued to be curative, however the role of chemotherapy and radiotherapy is open to be dispute.
As to meningeal tumors The second most frequent location for meningioma’s of posterior fossa is the Craniovertebral junction meningiomas which is either situated in the ventral or dorsal aspect of the foramen magnum, ventral foramen magnum lesions are obviously more difficult to approach surgically, as the brain stem, lower cranial nerves vertebral artery and the occipital condyles, all hinder proper exposure. Multiple intracranial tumors represent 4 to 8% of all brain neoplasm.
However it is well recognized that the association of CPP and meningioma a rare event. Regarding pathogenesis, there are several hypothesis.one of which was the COHENHELM THEORY suggesting a multipotential oncogenic role of embryonal rests 6, 7. There was also a hypothesis proposing a genetic link between the two tumors 11, although, on a histopathological level, they seem to be different. However, under close scrutiny both of these hypothesis were refuted 2, 12.
Although, most authors consider the concurrence of meningiomas and CCP to be a more coincidence, the fact that a third of reported cases of the two tumors stated that they were in adjacent locations demands a better explanation. It’s possible that the tumor occurring first could induce the formation of the other by acting as a local irritant 9, 10 having both tumors in close proximity to each other facilitates removal of both in one session.
Conclusions
This is a rare occurrence of concomitant meningioma and CPP. It has been speculated that the association of multiple different intracranial tumours might represent a "forme fruste" of central neurofibromatosis. But no proof of this hypothesis has been given so far. It also has been suggested that the meningioma itself might have acted as oncogenic stimulus to the development of the CCP tumor or "vice versa" in those cases, in which the two tumours are adjacently located. But the fact, that adjacent location occurs only in about one third of the reported cases, speaks against this assumption. It also cannot be supported by any other findings.
References
- Okay O., et al. “Choroid plexus papillomas in two siblings: Case report”. Turkish Neurosurgery 19.3 (2009): 281–284.
- Lee SH., et al. “Atypical choroid plexus papilloma in an adult”. Journal of Korean Neurosurgical Society 46.1 (2009): 74–76.
- Jinhu Y., et al. “Metastasis of a histologically benign choroid plexus papilloma: Case report and review of the literature”. Journal of Neuro-Oncology 83.1 (2007): 47–52.
- McCall T., et al. “Variations of disseminated choroid plexus papilloma: 2 case reports and a review of the literature”. Surgical Neurology 66 (2006): 62–68.
- Ahn SS and Cho YD. “Spinal drop metastasis from a posterior fossa choroid plexus papilloma”. Journal of Korean Neurosurgical Society 42 (2007): 475–477.
- Jellinger K. “Embryonal cell nests in human cerebellar nuclei” Zeitschrift für Anatomie und Entwicklungsgeschichte 138.2 (1972): 145–154.
- Friede RL. “Dating the development of human cerebellum”. Acta Neuropathologica 23.1 (1973): 48-58.
- Behrend RC. “Epidemiology of brain tumours”. Handb Neurology 16 (1974): 56-88.
- Deen HG and Laws ER. “Multiple primary brain tumours of different cell types”. Neurosurgery 8.1 (1981): 20-25.
- Gass H., et al. “Meningioma and oligoden- droglioma adjacent in the brain. Case report”. Journal of Neurosurgery 7.5 (1950): 440-443.
- Engelhard HH., et al. “Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equine”. Journal of Neurosurgery: Spine 13.1 (2010) : 67-77.
- Sackett JF., et al. “Meningeal and glial tumours in combination”. Neuroradiology 7.3 (1974):153-160.
- McLendon RE., et al. “Russell and Rubinstein’s Pathology of Tumors of the Nervous System”. CRC Press (2006)
- Langford LA. “Pathology of meningiomas”. Journal of Neuro-Oncology 29 (1996): 217-221.
- Weller RO “Microscopic morphology and histology of the human meninges”. Morphologie 89 (2005): 22-34.
- Nunes F., et al. “Inactivation patterns of NF2 and DAL-1/4.1B (EPB41L3) in sporadic meningioma”. Cancer Genetics and Cytogenetics 162 (2005): 135-139.
- Borden NM “Aggressive angioblastic meningioma with multiple sites in the neural axis”. American Journal of Neuroradiology 16 (1995): 793-794.
- Kamiya K., et al. “Malignant intraventricular meningioma with spinal metastasis through the cerebrospinal fluid”. Surgical Neurology 32 (1989): 213-218.
- Ludwin SK and Conley FK. “Malignant meningioma metastasizing through the cerebrospinal pathways”. Journal of Neurology, Neurosurgery, and Psychiatry 38 (1975):136-142.
- Hoffmann GT and Earle KM. “Meningioma with malignant transformation and implantation in the subarachnoid space”. Journal of Neurosurgery 17 (1960): 486-492.
Citation:
Muffaq Lashhab., et al. “Fourth Ventricle Papilloma and Cranio-Cervical Junction Meningioma: Coincidental Tumors: a Case
Report and Review of the Literature”. Current Opinions in Neurological Science 2.3 (2018): 463-467.
Copyright: © 2018 Muffaq Lashhab., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.