Research Article
Volume 4 Issue 1 - 2019
The Effects of Vitamin D on Multiple Sclerosis Relapse and Progression
Department of Neurology, Palmetto Health-University of South Carolina, Columbia, SC, USA
*Corresponding Author: Renu Pokharna, MD, FAANEM, MSCS, CRND, CNP, NM, Director of Clinical Neuro-Immunology, Department of Neurology, Prisma Health-USC, SC, USA.
Received: April 03, 2019; Published: May 06, 2019
Abstract
Purpose of Study: Multiple Sclerosis (MS) is an immune mediated inflammatory disease that affects the myelin around Central Nervous System (CNS) axons. The clinical presentation of the disease can vary greatly and is therefore classified into different types based on the patterns of relapses. Past research has shown that vitamin D may slow the progression of MS, but much of that research has been limited in scope. Our hypothesis is that MS patients who are taking Vitamin D supplements will have lower relapse rates and less disease progression compared to those who are not taking Vitamin D supplements.
Methods: We conducted a retrospective, cross sectional chart review of 392 patients from Prisma Health-USC Neurology. All types of MS, genders, ages, and races were included. Chi-square and Mann-Whitney statistical analyses were performed to examine the relationship between Vitamin D usages and relapse number.
Results: The Chi-square analysis found the relationship between these variables to be statistically insignificant, X2 (1, N = 392) = 0.05, p = 0.821. The Mann-Whitney analysis also found that the number of relapses were not significantly different for patients on Vitamin D (median relapse = 1, range = 0-10) than for those not on Vitamin D (median relapse = 0.5, range = 0-12) U = 18627, p = 0.743. Overall, our study failed to show a statistically significant relationship between Vitamin D and MS relapse progressions.
Conclusions: Our results failed to show a significant association between Vitamin D supplementation and MS relapse. More research needs to be done regarding the relationship between Vitamin D and MS relapse progression, specifically with prospective studies that can include controlled variables, checking Vitamin D levels, and larger sample sizes that include patients with all types of MS.
Keywords: Multiple sclerosis relapsing remitting; Multiple sclerosis relapses; Vitamin D
Introduction
Multiple Sclerosis (MS) is an immune mediated inflammatory disease that affects the myelin around CNS axons [1]. Because of the disease’s effects on Central Nervous System (CNS) axons, the disease presents with various autonomic, motor, and sensory symptoms [2] The etiology of MS is largely unknown, but a variant in one Major Histo-Compatibility (MHC) II gene, Epstein Barr Virus (EBV) infection, cigarette smoking, low Vitamin D levels, and place of residence during childhood all seem to contribute to MS development [3,4]. One common point of interest in MS research is Vitamin D. Most MS patients have low vitamin D levels at the time of diagnosis [5]. MS has been found to be more prevalent in the Northern Hemisphere, where there are shorter days and less sunlight on average [6]. Therefore, these populations are getting less exposure to vitamin D. These observations lead us to believe that there is a relationship between vitamin D and MS.
Still, the relationship between vitamin D and its effects on MS disease progression is unclear. Low vitamin D3 levels have been shown to be associated with increased relapse rates in both pediatric and adult CIS (Clinically Isolated Syndrome) patients [7]. Higher vitamin D levels have been associated with decreased relapse risk in Remitting Relapsing Multiple Sclerosis (RRMS) [8]. However, it has also been shown that high vitamin D has decreased the number of enhancing lesions in magnetic resonance imaging (MRI), but has had no effect in the progression of MS itself [9]. The anti-inflammatory actions of vitamin D may explain its relationship with MS. Vitamin D has been found to act on T cells, specifically inhibiting CD4+ T cell proliferation, IL-6, and IL-17. It also enhances regulatory T cells (CD4+CD25+FoxP3+) [10].
Overall, many of the studies regarding vitamin D and MS relapses are limited because of small sample sizes. Vitamin D supplementation has been shown to decrease the number of relapses and disease severity [5,11,12]. In one study, a 25-hydroxyvitamin D serum level of greater than or equal to 50 nmol/L had a fourth of the T2 lesion volume at the end of 60 months in MS population that were also taking interferon Beta 1 b (IFNB-1b) [13]. Another study showed that 25-hydroxyvitamin D had an effect on time to relapse and enhancing lesion load for MS patients on IFNβ and Glatiramer Acetate, however, no effect on MS relapse [15].
Still other studies have not shown these positive results with vitamin D supplementation and even others that are limited by a small sample size [10,11]. Recently a meta-analysis and a systematic review were published, each looking at various outcomes including annualized relapse rate, change in Expanded Disability Status Scale (EDSS), number of MRI gadolinium-enhancing T1 lesions and number of new MRI gadolinium-enhancing T1 and T2 lesions. Neither showed that vitamin D had a statistically significant effect on any of these outcomes [15,16]. Due to the unclear and conflicting data more research needs to be done to identify the effects of vitamin D on MS relapse and progression.
Therefore we decided to answer this question in our population whether Vitamin D is making any effect on relapses and hypothesized our research. For our study, it is hypothesized that patients that are taking vitamin D supplements will have a lower relapse rate and lower EDSS scores compared to those that are not taking any vitamin D supplements.
Methods
The project consisted of a retrospective, cross sectional chart review. Patients were all from Prisma Health-USC Neurology and had been diagnosed with MS using the 2010 Revised McDonalds criteria. The list of patients was compiled from ICD-10 G35 code between the time span of January 1, 2012 to May 17, 2018. All genders, ages, and races were included. Patients diagnosed with CIS, RRMS, SPMS (Secondary Relapsing Remitting Multiple Sclerosis), PPMS (Primary Progressive Multiple Sclerosis) and PRMS (Primary Remitting Relapsing Multiple Sclerosis) were all included. The data collected from each patient included: age, race, gender, EDSS scores and number of relapses, vitamin D usage, and other data to be used for future studies.
Statistical Analysis: Chi-square test was used to compare vitamin D and MS relapse. Mann-Whitney test was performed to compare the number of relapses for patients that were on vitamin D and not on vitamin D.
Results
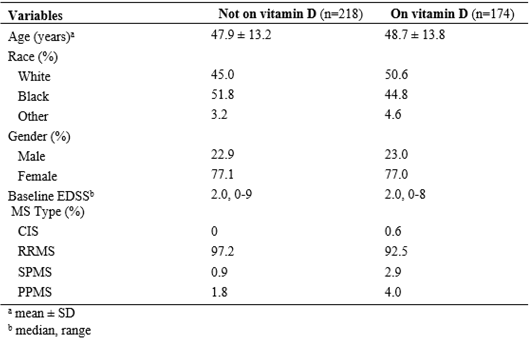
Four hundred twenty patients were collected, 392 of which had confirmed identities and diagnoses. The patient demographics and clinical characteristics are shown in Table 1.
Chi squared testing
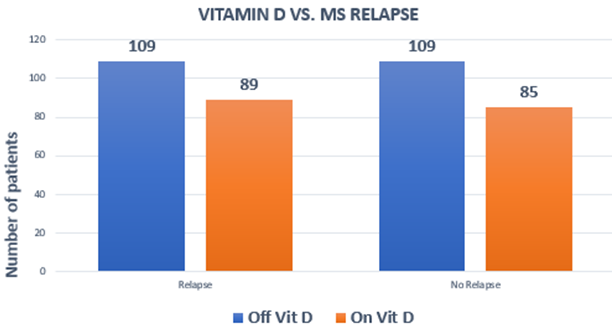
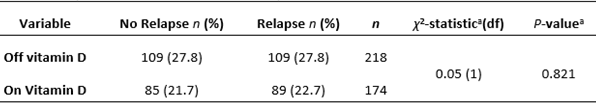
A cross-sectional analysis showed that 174 patients were on vitamin D (of which 89 had a relapse) and 218 patients were off vitamin D (of which 109 had a relapse), as shown in Figure 1. 22.7% of patients on vitamin D had a relapse and 27.8% of patients not on vitamin D had a relapse. The chi-square test showed an association between vitamin D and MS relapses that was not statistically significant; χ2 (1, n = 392) = 0.05, p = 0.821, as seen in Table 2.
A cross-sectional analysis showed that 174 patients were on vitamin D (of which 89 had a relapse) and 218 patients were off vitamin D (of which 109 had a relapse), as shown in Figure 1. 22.7% of patients on vitamin D had a relapse and 27.8% of patients not on vitamin D had a relapse. The chi-square test showed an association between vitamin D and MS relapses that was not statistically significant; χ2 (1, n = 392) = 0.05, p = 0.821, as seen in Table 2.
The Mann-Whitney test indicated that the number of relapses was not significantly different for patients on vitamin D, (median relapse(s) = 1.0, range = 0-10) versus patients that were not on vitamin D (median relapse(s) = 0.5, range = 0-12) U=18627, p = 0.743, as seen in Table 3.
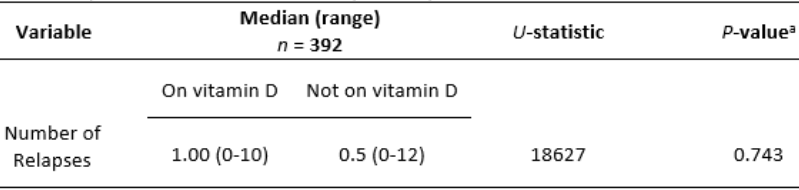
Table 3: Comparison of the number of relapses for patients on vitamin D and not on vitamin D.
aMann-Whitney test (2-tailed p-value)
aMann-Whitney test (2-tailed p-value)
Discussion
In this retrospective chart review, relationships between patients on vitamin D supplementation and MS relapses were investigated. Our results showed that there was no statistically significant association between vitamin D and the presence of an MS relapse (p=0.821). Additionally, our results showed that there was no statistically significant relationship between patients on vitamin D and their number of MS relapses.
Our study showed negative results unlike previous studies such as Wawrzyniak et al which showed that vitamin D deficiency was correlated with more frequent MS relapses in patients with RRMS [17]. Our study, however, looked at patients with all types of MS, not just RRMS. In fact, 4.6% of our patients had a type of MS other than RRMS and this could have skewed our results.
The primary limitation of our study was that this study was a retrospective chart review. Patients were recorded as either on vitamin D or not based solely on information provided in the chart. Serum vitamin D levels were not measured to ensure compliance. We also did not take into account start and stop dates or levels of vitamin D supplementation. Considering this, the patients that we considered to be on vitamin D for the purposes of the study may have misrepresented our true vitamin D patient population and caused our study to have negative results.
We also noted 49.5% of our patients (n=194) did not experience relapses. We believe that so many patients with zero relapses could likely have contributed to the negative results of our study. Possible reasons for these patients’ lack of relapses include treatment at other clinics, lack of patient follow-up, or failure in reporting of relapses to physicians.
Different disease modifying treatments (DMTs) between patients were not considered in our statistical analysis. The patients in our study were on a wide variety of DMTs or no medication at all. We did not include DMTs in our analysis because start and stop dates were not always clear and many patients used multiple DMTs throughout treatment.
Overall the relationship between vitamin D and its possible positive effects on MS outcomes is an area in need of continued research. Future prospective studies and controlling for many of the variables listed above would be highly valuable in investigating further the relationships between vitamin D and its effect on MS. I would think that a multi-centered randomized placebo-controlled trial with varying doses of vitamin D with DMT being taken into account would be great, also checking levels of vitamin D for compliance would be more informative, but not sure if that is realistic at this point.
References
- Ma, K., et al. “Rifampicin attenuates experimental autoimmune encephalomyelitis by inhibiting pathogenic Th17 cells responses”. Journal of neurochemistry 139.6 (2016): 1151-1162.A-DRB1 gene. US National Library of Medicine. Retrieved 12/30/2018 from https://ghr.nlm.nih.gov/gene/HLA-DRB!#conditions.
- Fahmi, R. M., et al. “Vitamin D Levels in Patients with Multiple Sclerosis”. Egyptian Journal of Neurology,Psychiatry & Neurosurgery 51.2 (2014): 145-152.
- Smolders, J., et al. “Vitamin D as an immune modulator in multiple sclerosis a review”. Journal of neuroimmunology 194.1(2008): 7-17.
- Mowry EM., et al. “Vitamin D status is associated with relapse rate in pediatric‐onset multiple sclerosis”. Annals of neurology 67.5 (2010): 618-624.
- Runia TF., et al. “Lower serum vitamin D levels are associated with a higher relapse risk in multiple sclerosis”. Neurology 79.3 (2012): 261-266.
- Kimball SM., et al. “Safety of vitamin D in adults with multiple sclerosis”. American Journal of Clinical Nutrition 86.3 (2007): 645-651.
- Correale J., et al. “Vitamin D-mediated immune regulation in multiple sclerosis”. Journal of the NeurologicalSciences 311 (2011): 23-31.
- Hossein-nezhad A and Holick MF. “Vitamin D for health: a global perspective”. Mayo Clinic Proceedings 88.7 (2013): 720-755.
- Pierrot-Deseilligny C., et al. “Relationship between 25-OH-D serum level and relapse rate in multiple sclerosis patients before and after vitamin D supplementation”. Therapeutic Advances in Neurological Disorders 5.4 (2012): 187-198.
- Ascherio A., et al. “Vitamin D as an early predictor of multiple sclerosis activity and progression”. JAMA Neurology 71.3 (2014): 306-314.
- Rotstein, D. L., et al. “Effect of vitamin D on MS activity by disease-modifying therapy class”. Neurology Neuroimmunology & Neuroinflammation 2.6 (2015): e167.
- McLaughlin L., et al. “Vitamin D for the treatment of multiple sclerosis: a meta-analysis”. Journal of Neurology 265.12 (2018): 2893-2905.
- Jagannath VA., et al. “Vitamin D for the management of multiple sclerosis”. Cochrane Database of Systematic Reviews (2018).
- Wawrzyniak S., et al. “Association of vitamin D status and clinical and radiological outcomes in a treated MS population in Poland”. Brain and Behavior 7.2 (2017): e00609.
Citation:
Renu Pokharna., et al. “The Effects of Vitamin D on Multiple Sclerosis Relapse and Progression”. Current Opinions in Neurological Science 4.1 (2019): 1-5.
Copyright: © 2019 Renu Pokharna., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.