Case Report
Volume 4 Issue 1 - 2019
3rd Nerve Palsy after Microsurgical Clipping of Basilar Top Aneurysm
1Associate prof .Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
2Neurosurgeon, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Resident, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
2Neurosurgeon, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
3Resident, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
*Corresponding Author: Bipin Chaurasia, Resident, Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Received: June 14, 2019; Published: July 25, 2019
Abstract
Postoperative oculomotor nerve palsy is a rare complication that occurs in the setting of micro-surgical aneurysm clipping. While a number of theories have been postulated to explain the development of postoperative oculomotor nerve palsies, the underlying pathophysiology of such complications still remain to be elucidated. In this report, we present a case of postoperative isolated ipsilateral oculomotor nerve palsy after clipping of basilar tip aneurysm which we believe may be attributed to peroperative oculomotor nerve manipulation related neuropraxia.
Keywords: Oculomotor nerve palsy; Basilar apex aneurysm; Postoperative
Introduction
Oculomotor nerve is the third cranial nerve that enters the orbit through the superior orbital fissure and controls muscles that drive most movements of the eye and raise the eyelid. Oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in the control of eye movement. Oculomotor nerve palsy is an eye condition resulting from damage to the third cranial nerve or a branch there of. As the name suggests, oculomotor nerve supplies the major¬ity of the muscles that control eye movements.
Therefore, damages to oculomotor nerve will render affected individuals unable to move his or her eye normally. Unilateral oculomotor nerve palsy is often encountered in the setting of ipsilateral aneurysms located at the posteri¬or communicating artery (PcomA), internal carotid artery (ICA) or their junction (PcomA/ICA). There have been some reports on ocu¬lomotor nerve palsy as a result of aneurysms in basilar tip, anterior artery or anterior communi¬cating artery. In the present report, we describe a case of basilar apex aneurysm presenting with ipsilateral postoperative oculo¬motor nerve palsy that is thought to be attrib¬uted to peroperative oculomotor nerve handling followed by neuropraxia.
Case Report
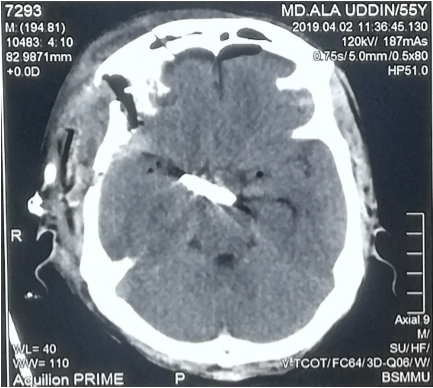
A 55years old hypertension male with no other significant past medical history or contributing family history complained about sudden severe headache for one hour followed by several episodes of vomiting and unconsciousness for 05 hours on admission at our hospital. Physical examination results were within nor¬mal limits except for considerable neck stiffness, positive Kernig sign and Brudzinski’s sign. Computed tomography (CT) scan demonstrated diffuse subarachnoid hemorrhage which was especially concentrated in ambient, sylvian fissure, interpeduncular and suprasellar cisterns with intraventricular extensions and mild triventricular hydrocephalus. (Figure 1).
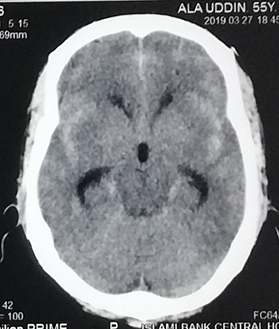
Figure 1: Computed tomography of the head show¬ing diffuse subarachnoid hemorrhage especially concentrated in ambient, sylvian fissure, interpeduncular and suprasellar cisterns with intraventricular extensions and mild triventricular hydrocephalus.
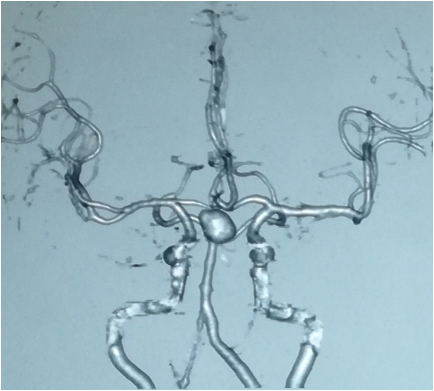
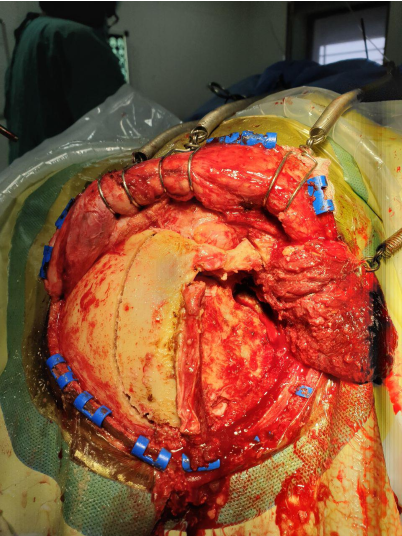
CT angiography (CTA) revealed a large saccular basilar tip aneurysm (approximately 10.7×9.5×10.5mm) (Figure 2A & 2B). The aneurysm was microsurgically clipped (Figure 4) via the right Orbitozygomatic approach (Figure 3). Postoperatively the patient developed complete right third nerve palsy characterized by the presence of dilated pupil, ptosis and downward deviation and abduction of the eyeball. CT scan revealed no postoperative intracranial hematoma and the surgical clip was in the proper location. However, compression of the basal cisterns and assessment of the ventricular system were noted (Figure 5). Postoperative CTA showed no existence of another aneurysm or vasospasm (Figure 6). The patient was discharged 02 weeks after the surgery. At this point, his mydriasis and eye lid drooping was still present to a lesser extent.
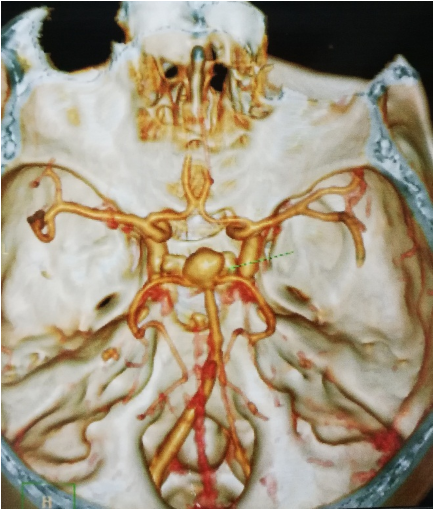
Figure 2B:
Figure 2A & 2B: Computed tomography angiography show¬ing a large saccular basilar tip aneurysm (approximately 10.7×9.5×10.5mm). The arrow indicates the aneurysm. At one-month follow-up, the patient’s pupil was slightly contracted and reflexed reluctantly to direct and indirect light stimulation.
Figure 2A & 2B: Computed tomography angiography show¬ing a large saccular basilar tip aneurysm (approximately 10.7×9.5×10.5mm). The arrow indicates the aneurysm. At one-month follow-up, the patient’s pupil was slightly contracted and reflexed reluctantly to direct and indirect light stimulation.
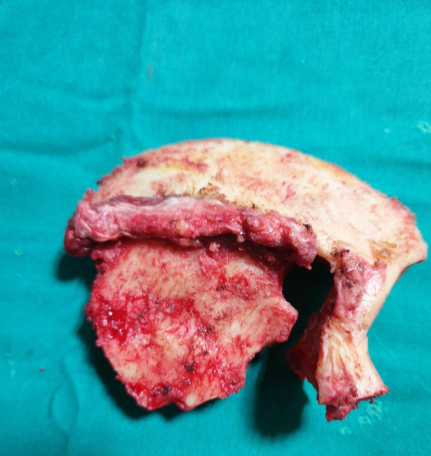
Figure 3B:
Figure 3A & 3B: Right sided Orbitozygomatic craniotomy (one piece), extradural anterior clinoidectomy & clipping of basilar apex aneurysm through trans-sylvian approach.
Figure 3A & 3B: Right sided Orbitozygomatic craniotomy (one piece), extradural anterior clinoidectomy & clipping of basilar apex aneurysm through trans-sylvian approach.

Figure 3B:
Figure 3A & 3B: Right sided Orbitozygomatic craniotomy (one piece), extradural anterior clinoidectomy & clipping of basilar apex aneurysm through trans-sylvian approach.
Figure 3A & 3B: Right sided Orbitozygomatic craniotomy (one piece), extradural anterior clinoidectomy & clipping of basilar apex aneurysm through trans-sylvian approach.
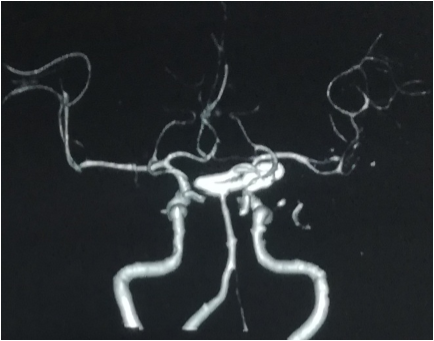
Figure 5: CT scan revealed no postoperative intracranial hematoma and the surgical clip was in the proper location.

Figure 6: Postoperative CTA showed no existence of another aneurysm or vasospasm and the surgical clip was in the proper location.
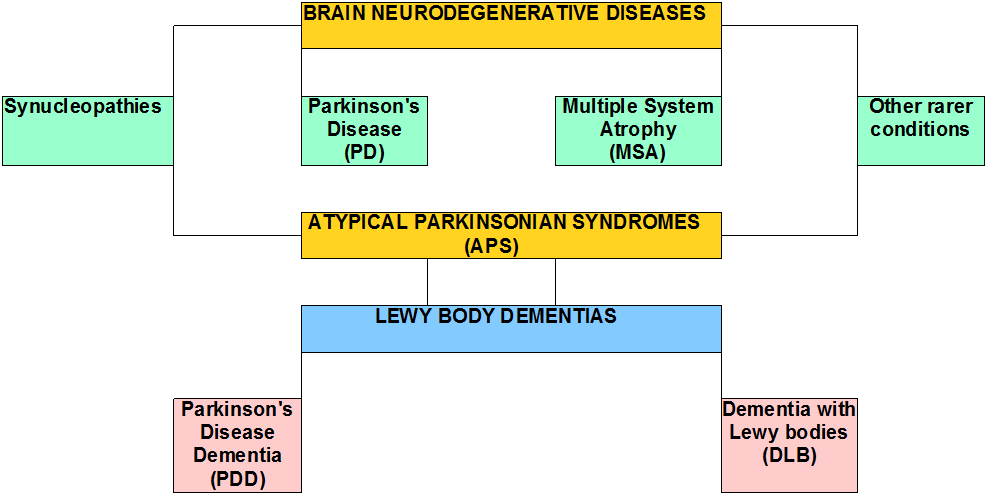
Figure 7: On postoperative day two, the patient developed a complete right third nerve palsy. Picture was taken with kind permission of the patient).
Discussion
There are many proposed hypotheses pertain¬ing to the etiology of oculomotor nerve palsy before and after aneurysm surgery. Direct com¬pression by the aneurysm is the most classic and common cause. Other causes include direct injury to the third nerve intraoperatively [6], microvascular ischemia [9], focal hemato¬ma formation [3], vasospasm [8, 12], anomaly of the vessels along the oculomotor nerve [10], elevated intracranial pressure and herniation, compression by intracranial structures other than aneurysms [7], and undetermined ori¬gins [11].
In the present case, compression by aneurysm may not be possible because of the anatomi¬cal distance between the two entities. Postoperative CT, CTA decrease the chances of hematoma formation, vasospasm and elevated intracranial pressure. Although we cannot rule out the possibility of ischemic injury to the oculomotor nerve. Small vessel ischemic injury to oculomotor nerve usu¬ally exhibits pupil-sparing [9] whereas our patient demonstrated a blown pupil. So we believe that, probably from coarse dissection of the cavernous sinus dura and as well as direct anterior clinoidectomy or from heat of the low power drill may be responsible for the 3rd nerve palsy of our patient.
References
- Aiba T and Fukuda M. “Unilateral oculomotor nerve paresis associated with anterior communicating artery aneurysm rupture--two case reports”. Neurol Med Chir (Tokyo) 43 (2003): 484-487.
- Boccardo M., et al. “Isolated oculomotor palsy caused by aneurysm of the basilar artery bifurcation”. J Neurol 233.1 (1986): 61-62.
- Balossier A., et al. “Third nerve palsy induced by a ruptured anterior communicating artery aneurysm”. Br J Neurosurg 26 (2012): 770-772.
- Fairbanks C and White JB. “Oculomotor nerve palsy in the setting of an anterior cerebral A2 segment aneurysm”. J Neurointerv Surg 3.1 (2011): 74-76.
- Green WR., et al. “Neuro-Ophthalmologic Evaluation Of Oculomotor Nerve Paralysis”. Arch Ophthalmol 72 (1964): 154-167.
- Grayson MC., et al. “Analysis of the recovery of third nerve function after direct surgical intervention for posterior communicating aneurysms”. Br J Ophthalmol 58 (1974): 118-125.
- Jeon JS., et al. “Dissecting aneurysm of vertebral artery manifestating as contralateral abducens nerve palsy”. J Korean Neurosurg Soc 53 (2013): 194-196.
- Kudo T. “Postoperative oculomotor palsy due to vasospasm in a patient with a ruptured internal carotid artery aneurysm: a case report”. Neurosurgery 19 (1986): 274-277.
- Lee SH., et al. “Isolated oculomotor nerve palsy: diagnostic approach using the degree of external and internal dysfunction”. Clin Neurol Neurosurg 104 (2002): 136-141.
- Richards BW., et al. “Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves”. Am J Ophthalmol 113 (1992): 489-496.
- White JB., et al. “Isolated third nerve palsy associated with a ruptured anterior communicating artery aneurysm”. Neurocrit Care 7 (2007): 260-262.
- Chowdhury., et al. “Azygos anterior cerebral artery aneurysm with subarachnoid hemorrhage. Neuroimmunology Neuroinflammation 5 (2018): 39.
Citation:
Bipin Chaurasia., et al. “3rd Nerve Palsy after Microsurgical Clipping of Basilar Top Aneurysm”. Current Opinions in Neurological Science 4.1 (2019): 33-39.
Copyright: © 2019 Bipin Chaurasia., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






























 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.