Research Article
Volume 1 Issue 1 - 2016
Bioequivalence Study of Darunavir Ethanolate and Darunavir Propylene Glycolate Tablets 800 mg in Healthy Volunteers under Fed Conditions
1Clinical Pharmacology Department, APL Research Centre, Aurobindo Pharma Ltd, Survey no.313, Bachupally, Hyderabad, Telangana, India
2Clinical Operations, Axis Clinicals Latina, Mexico
2Clinical Operations, Axis Clinicals Latina, Mexico
*Corresponding Author: Akula Thukaram Bapuji, Sr. Vice President, APL Research Centre, Aurobindo Pharma Ltd, Hyderabad, Telangana, India.
Received: September 23, 2016; Published: October 22, 2016
Abstract
Background: Darunavir is an inhibitor of the human immunodeficiency virus (HIV-1) protease. Darunavir exists in various pseudo polymorphs such as alcohol solvates, hydrate solvates, alkane solvates. Darunavir was approved in US in the form of Darunavir ethanolate (RLD). Aurobindo Pharma Ltd, India developed Darunavir as Darunavir propylene glycolate tablets. Both Darunavir ethanolate and Darunavir propylene glycolate are alcohol solvates used to improve stability and bioavailability of Darunavir; however pharmacokinetic and bioequivalence data of Darunavir propylene glycolate tablets in healthy volunteers is not available.
Objective: This study was designed to evaluate the bioequivalence of Darunavir Propylene Glycolate tablets manufactured by Aurobindo Pharma Ltd, India with PREZISTA (Darunavir ethanolate) Tablets 800 mg reference formulation of Janssen Ortho LLC, USA in healthy volunteers under fed conditions. This study compared dissolution profiles, relative bioavailability, pharmacokinetics, safety and tolerability of Darunavir ethanolate and Darunavir propylene glycolate tablet formulations.
Methods: To evaluate the pharmaceutical equivalence of the test and reference products, in vitro dissolution test was performed using the US Pharmacopeia (USP) dissolution apparatus-II, paddle method and a simple model independent approach using the difference factor (f1) and the similarity factor (f2) were adopted to compare dissolution profiles. After an overnight fasting of at least 10.0 hours and exactly 30 minutes after serving of a high fat high calorie meal, a single oral 800-mg dose of the 2 formulations were administered to 14 healthy volunteers under fed conditions in a randomized, open- label, 2-treatment, 2-sequence, 2-period crossover study with washout period of 7 days. In addition, 100 mg Ritonavir (NORVIR) was administered every 12 hours for two days prior to administration of Darunavir and till sampling of 36.00 hours post dose in each period. Darunavir plasma concentrations were quantified using a validated LC-MS/MS detection method and were used to determine the pharmacokinetic parameters. As mandated by the US Food and Drug Administration, the test and reference formulations were considered bioequivalent if the T/R ratios and 90% CI’s of the geometric mean ratios for the log-transformed values of pharmacokinetic parameters were within the predetermined range of 80.00 to 125.00.
Results: When subjected to a simple model independent approach of dissolution profile comparison, f1 (difference) and f2 (similarity factor) were found to be 4.44 and 66.64 respectively. Similarly, the two Darunavir Tablet formulations were safe and well tolerated by all the volunteers. The T/R ratios (90% CI’s) for the ratios of Cmax, AUC0-t and AUC0-inf respectively were 111.40 (97.44-127.35), 108.81 (97.81-121.05) and 112.31 (96.04-131.33).
Conclusion: The results of this single-dose fed study showed that test formulation developed with Darunavir propylene glycolate solvate form was found to be predictive bioequivalent to reference formulation in healthy volunteers. Both test and reference formulations were safe and well tolerated.
Keywords: Darunavir propylene glycolate; Darunavir ethanolate bioequivalence; LC-MS/MS detection method; Human plasma; Pharmacokinetics; Safety
Abbreviations: PI: Protease inhibitor; DRV: Darunavir; HIV: Human Immunodeficiency virus; BMI: Body mass index; CI: Confidence Intervals; AUC: Area under the curve; ESI: Electrospray ionization
Introduction
Darunavir [DRV, Prezista (1R, 5S, 6R)-2,8-dioxabicyclo [3.3.0] oct-6-yl]-N-[(2S,3R)- -[(4-aminophenyl) sulfonyl-(2-methylpropyl) amino]-3-hydroxy-1-phenyl-butan-2-yl] carbamate, formerly known as TMC114], is a new HIV peptidic protease inhibitor (PI), with high levels of antiviral activity against wild- type virus and stains with phenotypic resistance to other protease inhibitors (PIs) [1,2]. Darunavir is chemically related to amprenavir [3], and efficient in vitro against viral strains less sensitive to other PIs [4,1]. DRV is a key component of many salvage therapies in multi-treated patients. The efficacy of darunavir against PI-resistant strains was clinically confirmed as this drug was successfully administered to heavily pretreated patients who experienced a virological failure after several boosted-PIs [5]. The Power III clinical study also confirmed that darunavir treatment achieved a higher virologic response in pretreated patients compared to usual boosted PIs [6]. Darunavir prevents the formation of mature infectious virus particles by inhibiting the cleavage of HIV-1 encoded gag-pol polyproteins in virus- infected cells. [7] As with other PIs, the metabolism of DRV is cytochrome P450 (CYP) 3A4-dependent and is generally co-administered with low-dose of ritonavir. DRV was licensed in June 2006 in the USA and subsequently in European Union in February 2007 [8].
Bioequivalence means comparison of pharmacokinetics of two different formulations which are expected to show similar in vivo response i.e similar in terms of safety and efficacy.
Two formulations are said to be bioequivalent if they exhibit similar rate and extent of absorption assessed by means of pharmacokinetic parameters Cmax & AUC derived from plasma concentration time curve when administered in same molar dose.
Bioequivalence can be established through various methods, including in vivo and in vitro methods; however, the pharmacokinetic approach is the most commonly used method. The reason might be that the primary aim of bioequivalence studies is to assess the rate and extent of drug absorption, which can be readily assessed by key pharmacokinetic parameters such as Cmax, Tmax, AUC and t1/2 [9,10].
Currently pharmacokinetic and bioequivalence data of Darunavir propylene glycolate tablets 800 mg in healthy volunteers is not available.
This study compared the relative bioavailability and pharmacokinetics of test formulation (Darunavir propylene glycolate tablets 800 mg) developed by Aurobindo Pharma Ltd, India with that of reference formulation [PREZISTA (Darunavir ethanolate) Tablets 800 mg] of Janssen Ortho LLC, USA in healthy mexican volunteers under fed conditions.
Methods
Formulations: The reference formulation and test formulation of Darunavir were 800 mg Tablets. The test formulation is Darunavir propylene glycolate 800 mg tablets manufactured by Aurobindo Pharma Ltd, India. The reference formulation is PREZISTA® (Darunavir ethanolate) Tablets 800 mg manufactured by Janssen Ortho LLC, USA. Each tablet of test formulation contains Darunavir propylene glycolate equivalent to 800 mg Darunavir. Each tablet of reference formulation contains darunavir ethanolate equivalent to 800 mg of darunavir. Norvir® (Ritonavir) Tablets100 mg tablets were manufactured by AbbVie Inc, USA.
Assay and In-vitro Dissolution Studies: To evaluate the pharmaceutical equivalence between the test and reference products, dissolution test was performed using the US Pharmacopeia (USP) dissolution apparatus-II, paddle method according to the official monograph. Samples collected at various time intervals were analyzed using the RP-HPLC/UV detection method, and a simple model independent approach using the difference factor (f1) and the similarity factor (f2) was adopted to compare dissolution profiles. The f1 calculates the percent difference between the 2 curves at each time point and is the measure of the relative error between the 2 curves, whereas the f2 is a logarithmic reciprocal square root transformation of the sum of squared error and is the measure of the similarity in the percent of dissolution between the 2 curves. These factors were calculated using the following equations, respectively:
f1= {[St=1n |Rt-Tt|]/[St=1n Rt]} x 100
f2= 50 x log {[1+ (1/n) St=1n (Rt-Tt) 2]-0.5 x 100}
f1= {[St=1n |Rt-Tt|]/[St=1n Rt]} x 100
f2= 50 x log {[1+ (1/n) St=1n (Rt-Tt) 2]-0.5 x 100}
Where n is the number of time points, Rt is the dissolution value of the reference product at time t, and Tt is the dissolution value of the test product at time t.
Using the mean dissolution values from both curves at each time interval, f1 and f2 were calculated using the above mentioned equations. For curves to be considered similar, f1 values should be close to 0, and f2 values should be close to 100. Generally, f1 values up to 15 (0–15) and f2 values ≥ 50 (50–100) ensure sameness or equivalence of the 2 curves and, thus, of the performance of the 2 products.
Volunteers: This study was conducted according to the principles of the Declaration of Helsinki and its amendments. The study protocol was approved by the Ethical Committee of the AXIS CLINICALS LATINA S.A. de C.V, Ing. Basiliso Romo Anguiano No. 225Col. Guadalupe Insurgentes, Ciudad de México, C.P. 07870. The study objectives and the effects of drugs used in the study were explained to volunteers at the start of the study, and informed consent was obtained. Study volunteers were also compensated financially.
Healthy adult male and female Mexican volunteers aged between 18 and 55 years were recruited for this study. A detailed medical history was obtained and a clinical examination was performed for all volunteers at the beginning of the study under the supervision of a qualified physician. In addition, 12-lead electrocardiography, complete blood count, blood pressure, blood sugar level, liver function tests, lipid profile, and renal function tests were also carried out in all study volunteers. Volunteers were confirmed with negative test result of alcoholometry, respiratory income of each period prior to the administration of Darunavir and Ritonavir formulations. All the Subjects were within the BMI ranging from 18 to 27 kg/m2. Participating women should not be pregnant or lactating. They must sign a letter of commitment of being not pregnant (since the signing of informed consent).
| No. Vol. | Gender | Age (years) | Weight (kg) | Height (m) | BMI (kg/m2) |
| 01 | Female | 42 | 52.2 | 1.47 | 24.2 |
| 02 | Female | 47 | 55.4 | 1.48 | 25.3 |
| 03 | Male | 35 | 69.0 | 1.71 | 23.6 |
| 04 | Female | 37 | 56.8 | 1.57 | 23.0 |
| 05 | Female | 24 | 55.3 | 1.58 | 22.1 |
| 06 | Male | 33 | 73.2 | 1.66 | 26.6 |
| 07 | Male | 33 | 71.3 | 1.73 | 23.8 |
| 08 | Male | 30 | 78.5 | 1.77 | 25.1 |
| 09 | Male | 27 | 78.7 | 1.81 | 24.0 |
| 10 | Female | 37 | 55.2 | 1.59 | 21.9 |
| 11 | Male | 25 | 64.3 | 1.66 | 23.3 |
| 12 | Female | 34 | 59.9 | 1.61 | 23.1 |
| 13 | Male | 45 | 71.2 | 1.64 | 26.5 |
| 14 | Female | 25 | 54.2 | 1.54 | 22.9 |
| Average | 33.9 | 63.9 | 1.63 | 24 | |
| Standard Deviation | 7.3 | 9.5 | 0.10 | 1.5 | |
| Minimum | 24.0 | 52.2 | 1.47 | 21.9 | |
| Maximum | 47.00 | 78.7 | 1.81 | 26.6 | |
| % CV | 21.7 | 14.9 | 6.24 | 5.1 | |
Volunteers per gender: |
Male |
7 |
Female |
7 |
Table 1: Demographical data of the volunteers who participated in the clinical study.
Volunteers with a history of hypersensitivity to study drug or any other drugs belonging to the same therapeutic group and history of bronchial asthma were excluded. Volunteers with recent history of drug abuse, including alcohol and with a history or physical examination evidence of gastrointestinal disease, kidney, liver, endocrine, respiratory, cardiovascular, dermatological or hematological clinically significant were also excluded from the study. Volunteers who had taken potentially toxic drugs within 30 days before the start of the study and who have taken any medication within 14 days or 7 half-lives thereof, prior to the start of the study were also excluded. Volunteers who have donated or lost 450 mL or more of blood within 60 days prior to study and who consumed grapefruit juice or drinks, or spicy foods in the 10 hours prior to admission of the study drug were also excluded from the study.
Study Design and Drug Administration: Various bioequivalence parameters of the 2 products were assessed under fed conditions in a randomized, open-labeled, balanced, 2-treatment, 2-sequence, 2-period, single-dose, crossover study with a 1-week washout period at the AXIS CLINICALS LATINA S.A. de C.V, Ing. Basiliso Romo Anguiano No. 225Col. Guadalupe Insurgentes, Ciudad de México, C.P. 07870 after obtaining approval from REC (Research and Ethics Committee), Mexico & COFEPRIS (Federal Commission for the Protection Against Sanitary Risks) with authorization number 163300410B0147/2016.
Using SAS software generated randomization schedule, volunteers were randomly divided into 2 groups (group 1 and group 2), each group consisting of 7 healthy volunteers. During the first study period, healthy volunteers from group 1 received a single oral 800-mg dose of the reference formulation, where as healthy volunteers from group 2 received the test formulation. In the second study period, the order was reversed. A non-blind approach was applied; both volunteers and investigators were aware of the formulations given to each group.
| Study Period | Group | Darunavir Formulation Administered |
| First Period | 1 | One tablet of Darunavir Ethanolate (Reference formulation) and 1 tablet of Ritonavir 100 mg |
| 2 | One tablet of Darunavir Propylene Glycolate (Test formulation) and 1 tablet of Ritonavir 100 mg | |
| 1 week washout period | ||
| Second Period | 1 | One tablet of Darunavir Propylene Glycolate (Test formulation) and 1 tablet of Ritonavir 100 mg |
| 2 | One tablet of Darunavir Ethanolate (Reference formulation) and 1 tablet of Ritonavir 100 mg | |
Table 2: Study Design for Bioequivalence Evaluation of Test and Reference Formulations of Darunavir Tablets.
In each period, a single oral dose of Ritonavir (NORVIR®) Tablets 100 mg manufactured by AbbVie Inc, USA was administered twice daily at an interval of 12 hrs which started two days before administration of a single oral dose of either one Reference tablet or Test Tablet of Darunavir 800 mg with 240 mL of drinking water at room temperature under fed conditions. High fat and high calorie breakfast was offered 30 minutes before study drug administration to all volunteers. Breakfast was of approximately 800 to 1000 calories with 150 cal, 250 cal & 500 to 600 cal derived from proteins, carbohydrates and fats respectively. Breakfast contained 2 eggs scrambled in butter, 2 strips of bacon, 2 slices of toast with butter, 2 grated potato croquettes and whole milk (240 mL). Ritonavir dosing was continued until 36.00 hours post dose in each period by study personnel under the supervision of Investigator.
Tolerability Assessment: Tolerability in volunteers was assessed before medication administration and at -48.00, 0.00, 3.00, 8.00 and 16.00 hours during the study through physical examination, monitoring vital signs(temperature, blood pressure, heart rate, and respiratory rate) and interviewing them about adverse events that may be associated with the use of Darunavir (eg, headache, nausea, vomiting, abdominal cramps/pain, loose and/or bloody stools, allergic reactions, hearing problems, eye or vision problems, speaking and swallowing problems, and muscular weakness) under the supervision of a qualified physician.
Three (03) adverse events were reported in 03 volunteers during the Clinical Study and according to medical criterion all of them were of moderate severity. These three adverse events were muscle pain, headache and diarrhea. There were no serious adverse events reported during the entire study. Both test (Darunavir propylene glycolate) and reference (Darunavir ethanolate) formulations were well tolerated by all the healthy volunteers in this study.
Sample Collection and Processing: Venous blood samples (6 mL) were collected at 0.00 (pre-dose in duplicate) and at 0.33, 0.67, 1.00, 1.50, 2.00, 2.50, 3.00, 3.50, 4.00, 5.00, 6.00, 8.00, 12.00, 16.00, 24.00, 36.00 and 48.00 hours post dose, drawn by venipuncture, by placing a catheter fixed, preferably in the anterior aspect of the forearm.
Blood samples were collected in tubes containing sodium heparin as anticoagulant; they were centrifuged to separate plasma immediately at 3500 rpm for 10 minutes, at a temperature between 2°C and 15°C, the separated plasma was transferred into Cryogenic tubes. Cryogenic tubes were frozen at -70 ± 15°C until analysis.
Analysis of Samples: Samples were analyzed by a validated LC-MS/MS method, discussed below.
Darunavir standard was received from TLC Pharmaceutical standards, Canada and Darunavir-d9 standard was received from TLC Pharmachem, Canada.
HPLC-grade solvents such as methanol, acetonitrile and all other chemicals and reagents such as Ammonium Acetate and Ammonium formate were purchased from J.T. Baker. Deionised water was prepared using a Millipore water system. All these reagents and chemicals were used without further purification.
Solid-phase extraction was adopted for the sample preparation. At the time of analysis, the samples were thawed at room temperature and Darunavir-d9 solution (6 µg/mL) as the internal standard was vertex- mixed with 200 µL plasma sample for 15 seconds. Then, these samples were added with 200 uL of 100 mm ammonium acetate buffer and mixed. Prelabelled Strata-X SPE cartridges were activated with1 mL of methanol equilibrated with 1 mL of deionized water and loaded the plasma samples onto respective prelabelled SPE cartridges and applied positive pressure to pass the plasma samples through SPE cartridges. Then, the sample SPE cartridges were washed with 1 mL of deionized water, followed by 1 mL of 10% methanol. The sample SPE cartridges were left drying for 3 minutes and samples were eluted with 1 mL of methanol into Prelabelled collection tubes. The eluted samples were evaporated for 20 minutes at 50°C and 20 psi nitrogen gas. The residues were dissolved in 0.5 mL mobile phase and 5 µL samples were injected to the chromatographic system.
The chromatographic separations were achieved using ACE C18 analytical column (5 µm 4.6 x 100 mm). The mobile phase consisted of Methanol-Acetonitrile-2 mm Ammonium formate buffer (70%:15%:15%). The flow rate of the mobile phase was set at 0.8 ml/ min. The column oven temperature was 35˚C. The auto sampler temperature was 5°C.
The Shimadzu HPLC system was coupled to an API 3200 MS/ MS triple-quadrupole system detector equipped with a turbo ion spray ionization (ESI) source (Applied Bio systems MDS, SCIEX, Canada). The turbo ion spray ionization source was operated in a negative mode. The ion spray voltage was adjusted to -4000 V. The mass spectrometer was operated at a unit resolution for both Q1 and Q3 in multiple reaction monitoring (MRM) mode. The transition of precursor to product ion was monitored at 548.20→392.10 for Darunavir and 557.30→401.20 for internal standard (Darunavir-d9). The method had a total run time 3 minutes. Chromatograms processing, data generation and concentrations back calculations were all performed by the Analyst software (Applied Biosystems, MDS, SCIEX and Canada).
The chromatographic method was validated according to international guidelines to establish selectivity, accuracy, precision, recovery, calibration curve, and stability.
Sample concentrations C, were calculated using the following formula
x = y-c/m
Where, x is analyte concentration in sample; y is ratio of analyte peak area/Internal standard peak area; m is slope of the calibration curve; and c is y-axis intercept value
x = y-c/m
Where, x is analyte concentration in sample; y is ratio of analyte peak area/Internal standard peak area; m is slope of the calibration curve; and c is y-axis intercept value
Pharmacokinetics and Statistical Analyses
Plasma concentrations of Darunavir at various time intervals following oral administration of the 2 products were determined for each volunteer and mean values were calculated. A noncompartment model was used to determine the following pharmacokinetic parameters: Cmax, Tmax, AUC0–t, AUC0-inf, kel and t1/2. Cmax and Tmax were obtained directly from the concentration–time curve; AUC was calculated using the linear trapezoidal method. Elimination rate constant (ke) was calculated by applying a log-linear regression analysis to at least the last 3 quantifiable Darunavir concentrations, and then t1/2 was calculated as 0.693/ke. All of these pharmacokinetic parameters were determined using the using the software Phoenix® WinNonlin® Version 6.4.
Plasma concentrations of Darunavir at various time intervals following oral administration of the 2 products were determined for each volunteer and mean values were calculated. A noncompartment model was used to determine the following pharmacokinetic parameters: Cmax, Tmax, AUC0–t, AUC0-inf, kel and t1/2. Cmax and Tmax were obtained directly from the concentration–time curve; AUC was calculated using the linear trapezoidal method. Elimination rate constant (ke) was calculated by applying a log-linear regression analysis to at least the last 3 quantifiable Darunavir concentrations, and then t1/2 was calculated as 0.693/ke. All of these pharmacokinetic parameters were determined using the using the software Phoenix® WinNonlin® Version 6.4.
Pharmacokinetic data for the 2 formulations were log-transformed before statistical analysis, which was based on the 90% CIs for the ratio of the geometric means for these log-transformed pharmacokinetic parameters of the 2 formulations (test/reference).
The lower boundary (LB) and higher boundary (HB) of 90% CIs were calculated using the following equations [11]:
LB = e(MD-[t-value X SD/√n])
HB = e(MD+ [t-value X SD/√n])
Where MD is the mean difference and SD refers to the standard deviation of the transformed metric; n is the number of patients in the study;
LB = e(MD-[t-value X SD/√n])
HB = e(MD+ [t-value X SD/√n])
Where MD is the mean difference and SD refers to the standard deviation of the transformed metric; n is the number of patients in the study;
If the 90% CIs for the ratios of Cmax, AUC0–t and AUC0-inf values of the test and reference formulations fell within the range of 80.00 to 125.00, then these formulations were considered bioequivalent, as recommended by the USFDA [12].
Results
Assay and In-vitro Dissolution Studies: The mean (SD) percentage of the active ingredient in the test and reference formulations was found to be 99% (2%) and 98% (1%), respectively.
Darunavir mean in vitro drug release (dissolution) profiles of the test and reference tablet formulations were determined (Figure 1) and the data were subjected to a simple model independent approach of dissolution profile comparison. The f1 and the f2 were found to be 4.44 and 66.64, respectively (Table 3).
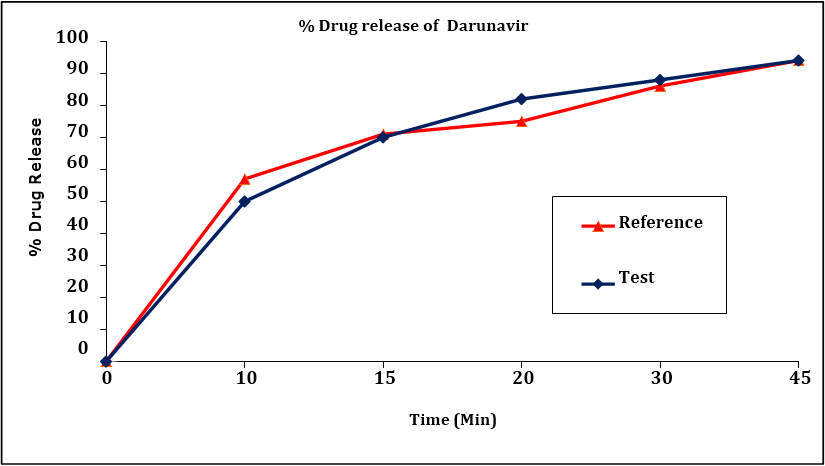
Figure 1: Darunavir in vitro drug release profile of test and reference formulations. Each point represents mean (SD) of 12 Tablets.
| Time (min) | Mean % Release | Difference Factor (f1) |
Similarity Factor (f2) |
|
| Test Formulation |
Reference Formulation |
|||
| 0 | 0 | 0 | 4.44 | 66.64 |
| 10 | 50 | 57 | ||
| 15 | 70 | 71 | ||
| 20 | 82 | 75 | ||
| 30 | 88 | 86 | ||
| 45 | 94 | 94 | ||
Table 3: Comparison of the dissolution profile of 2 Darunavir Tablet formulations (n = 12, where n is the number of tablets tested of each formulation).
Tolerability: Both test (Darunavir propylene glycolate) and reference (Darunavir ethanolate) formulations were well tolerated by all the healthy volunteers in this study. No unexpected incidents occurred that influenced study outcomes, and all the 14 volunteers continued to study end and were discharged in good health.
Validation of the Analytical Method: The LC-MS/MS method developed for the quantification of Darunavir in plasma was linear in the range of 50.0 to 15008.9 ng/mL, where at the LLOQ accuracy obtained was 98.94% (less than 20% deviation) and 89.90%-106.40% for standard points higher than LLOQ (less than 15% deviation), and 75% ratio of total standard points were accepted. The correlation coefficients (r) of all standard curves were more than 0.9976 for plasma samples. The lower limit of quantification was 50ng/mL for darunavir in plasma. LLOQ response is identifiable, discrete and reproducible with precision and accuracy of ± 20%. The peak is identifiable, precise and accurate at this concentration. Specificity of the method was verified by the absence of any co-eluted peaks of endogenous plasma component at the retention times of the drug or the internal standard. All samples passed the acceptance criteria. The intra-day accuracies were 97.86% and 98.42% for LLOQ and 100.62%-105.24% for QC's above LLOQ and the inter-day accuracies were 98.42% for LLOQ and 97.17%-101.17% for QC's above LLOQ. The intra-day precision was 4.00% for LLOQ and 0.80-1.80 for QC's above LLOQ. The inter-day precision was 3.60% for LLOQ and 1.30-3.70 for QC's above LLOQ. This results support the fact that the method is accurate and precise, where deviations obtained were less than 20% for LLOQ and less than 15% for the QC's above the LLOQ. The average extraction recoveries of darunavir determined at 149.5, 6307.4 and 11426.5 ng/ml were 78.7%, 74.5% and 83.0% respectively, while that of internal standard (Darunavir-d9) was 76.9% with high degree of precision, accuracy and reproducibility. Darunavir was stable with absolute percentages of deviation of calculated vs theoretical concentration being less than 15% for auto sampler, freeze-thaw, short-term and long-term stabilities determined at two concentrations of 149.5 and 11426.5 ng/ml. The stability was within the limit of 85.00%-115.00% & the CV% less than 15.00%.
Pharmacokinetics and Statistical Analyses: Darunavir mean plasma concentration–time profiles after administration of the test and reference formulations under fed conditions in Mexican healthy volunteers are shown in Figure 2. Mean (SD) values of various pharmacokinetic parameters for the test and reference formulations respectively for Cmax were 8513.6 (1863.00) and 7669.4 (1620.13) ng/mL; AUC0-t were 113076.1 (28661.36) and 103483.1 (23158.80) ng•h/mL; AUC0-inf were 149595.6 (42627.74) and 131229.1 (30372.29) ng•h/mL; t1/2 were 22.46 (11.815) and 21.79 (8.512) h; Tmax were 4.43 (1.542) and 4.96 (1.781) h; Kel were 0.0379 (0.02225) and 0.0364 (0.01336) h-1. Similarly, the 90% CIs for the ratios of Cmax, AUC0–t and AUC0-inf for the 2 formulations respectively were 97.44-127.35, 97.81-121.05 and 96.04-131.33 which along with summary statistics such as median, range, and %CV, are given in Table 4.
| Pharmacokinetic Parameters | Test Formulation | Reference Formulation | P value | T/R Point Estimate (90% CI) |
| Cmax (ng/mL ) Mean (SD) Range Median %CV |
8513.6 (1863.00) 5617.9-12359.8 8263.1 21.88 |
7669.4 (1620.13) 3941.8-9798.0 8159.6 21.12 |
0.1763 |
111.40 (97.44-127.35) |
| AUC0-t (hr.ng/mL) Mean (SD) Range Median %CV |
113076.1 (28661.36) 78623.5-171867.6 106324.4 25.35 |
103483.1 (23158.80) 65248.0-138909.7 99110.6 22.38 |
0.1832 |
108.81 (97.81-121.05) |
| AUC0-inf (hr.ng/mL) Mean (SD) Range Median %CV |
149595.6 (42627.74) 79913.1-207268.0 155976.4 28.50 |
131229.1 (30372.29) 77051.4-167625.3 142394.6 23.14 |
0.2109 |
112.31 (96.04-131.33) |
| Tmax (h) Mean (SD) Range Median %CV |
4.43 (1.542) 2.50-8.00 3.75 34.83 |
4.96 (1.781) 2.00-8.00 4.50 35.87 |
-- |
-- |
| t1/2 (hr) Mean (SD) Range Median %CV |
22.46 (11.815) 6.95-54.48 19.72 52.60 |
21.79 (8.512) 9.82-44.91 19.56 39.07 |
-- |
-- |
| Kel (hr-1) Mean (SD) Range Median %CV |
0.0379 (0.02225) 0.0100-0.1000 0.0350 58.77 |
0.0364 (0.01336) 0.0200-0.0700 0.0400 36.68 |
Table 4: Pharmacokinetic parameters and 90% CIs for the ratios of the geometric means of their log- transformed values for the 2 Darunavir tablet formulations under fed conditions (n = 14, where n is the number of volunteers).
Discussion
Aspects of this study design such as use of a single dose, recruitment of healthy volunteers, fed, standardized diet, fluid intake etc and the study conditions were consistent with the regulatory guidelines [12,13] to bring uniformity in the testing conditions for the 2 formulations.
The mean values for Cmax, Tmax, AUC0-t, AUC0-inf, Kel and t1/2 of the 2 formulations did not differ significantly (P ≥ 0.05), suggesting that the plasma profiles generated by the test formulation were not significantly different from those produced by the reference formulation.
Based on the observed T/R ratios and 90% CI’s of Cmax, AUC0-t and AUC0-inf, it was evident that the test formulation showed similar in-vivo profile to that of reference formulation under fed conditions. Similarly, the in vitro dissolution studies found that the formulations were pharmaceutically equivalent with respect to dosage form.
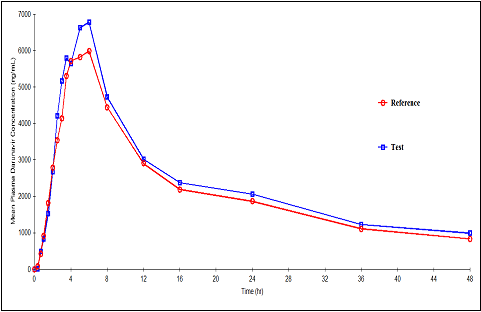
Figure 2: Plasma concentration versus time profile for Darunavir after 800-mg oral dose of test and reference formulations under fed conditions. Each point represents mean (ng/mL).
Conclusions
The results of this single-dose fed study showed that test formulation developed with Darunavir propylene glycolate solvate form was found to be predictive bioequivalent to reference formulation in healthy male and female volunteers. No statistically significant differences were found among in vitro dissolution profiles, relative bioavailability and pharmacokinetic parameters. The study also concluded that test formulation developed with propylene glycolate solvate form has similar in-vitro and in-vivo behaviour to that of reference formulation with ethanolate solvate form and both test and reference formulations were safe and well tolerated.
Acknowledgments
All authors contributed equally to this study. Axis Clinicals Ltd, Mexico was selected by Aurobindo Pharma Ltd, India to design and perform this bioequivalence study and to determine whether the test formulation developed by Aurobindo is bioequivalent to reference formulation. The authors have indicated that they have no other conflicts of interest regarding the content of this article.
References
- S. De Meyer, H. Azijn, D. Surleraux, D. Jochmans, A. Tahri, R. Pauwels, P. Wigerinck,M.P. DeBethune, Antimicrob. Agents Chemother.49 (2007) 2314.
- Y. Koh, H. Nakata, K. Maeda, H. Ogata, G. Bilcer, T. Devasamudram, J.F. Kincaid,P. Boross, Y.-F. Wang, Y. Tie, P. Volarath, L. Gaddis, R.W. Harrison, I.T. Weber,A.K. Ghosh, H. Mitsuya, Antimicrob. Agents Chemother.47 (2003) 3123.
- N.M. King, M. Prabu-Jeyabalan, E.A. Nalivaika, P. Wigerinck, M.-P. deBethune, C.A. Schiffer, J. Virol. 78 (2004) 12012.[4] M. Vermeir, S. Lachau-Durand, G. Manners, F. Cuyckens, B. van Hoof, A. Raoof,Drug Metab.Dispos.37 (2009) 809.
- Y. Koh, H. Nakata, K. Maeda, H. Ogata, G. Bilcer, T. Devasamudram, J.F.Kincaid, P. Boross, Y.-F.Wang, Y. Tie, P. Volarath, L. Gaddis, R.W. Harrison,I.T.Weber, A.K. Ghosh, H. Mitsuya, Antimicrob. Agents Chemother.47 (2003) 3123.
- E. Poveda, F. Blanco, P. Garcia-Gasco, A. Alcolea, V. Briz, V. Soriano,AIDS 20 (2006) 1558.
- J.M. Molina, C. Katlama, B. Grinsztejn, A. Timerman, R. Pedro, S. DeMeyer, M.P. de B´ethune, T. Vangeneugden, E. Lefebvre, Proceedings ofthe XVI International AIDS Conference, Toronto, Canada, 2006, TUPE0060.
- M. Vermeir, S. Lachau-Durand, G. Manners, F. Cuyckens, B. van Hoof, A. Raoof,Drug Metab.Dispos.37 (2009) 809.
- V.J. Sekar, E. Lefebvre, M. De Pauw, T. Vangeneugden, R.M. Hoetelmans, Br. J.Clin. Pharmacol.66 (2008) 215.
- Chow SC, Liu JP. Design and Analysis of Bioavailability and Bioequivalence Studies. 3rd ed. BocaRaton, Fl: Chapman & Hall/CRC; 2008.
- Shargel L, Yu ABC. Applied Biopharmaceutics and Pharmacokinetics. Stamford, Conn: Appleton& Lange Norwalk; 1999.
- Balthasar JP. “Bioequivalence and Bioequivalency Testing”. American Journal of Pharmaceutical Education63 (1999); 194-198.
- Food and Drug Administration (FDA). Guidance for industry: bioavailability and bioequivalence studies for orally administered drug products — general considerations. Rockville, Md: United States Department of Health and Human Services, FDA, Center for Drug Evaluation and Research (CDER), Revision 1; 2003.
- European Medicines Agency (EMEA). Guideline on the investigation of bioequivalence [CPMP/EWP/QWP/1401/98],Rev.1/Corr**.London,UK;20 January 2010.
Citation:
Akula Thukaram Bapuji., et al. “Bioequivalence Study of Darunavir Ethanolate and Darunavir Propylene Glycolate Tab-lets 800 mg in Healthy Volunteers under Fed Conditions”. Chronicles of Pharmaceutical Science 1.1 (2016): 21-31.
Copyright: © 2016 Akula Thukaram Bapuji., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.