Research Article
Volume 3 Issue 1 - 2018
Plasmodium falciparum Malaria among Pregnant Women Attending Ante - Natal Clinic, Federal Medical Center, Birnin Kudu, Jigawa State, Nigeria
1Department of Biology, Kano University of Science and Technology Wudil, Kano, Nigeria
2Department of Biological Sciences, Bayero University Kano, Nigeria
3Department of Biological Sciences, Federal University Gusau, Nigeria
4Department of Microbiology, Kano University of Science and Technology Wudil Kano, Nigeria
2Department of Biological Sciences, Bayero University Kano, Nigeria
3Department of Biological Sciences, Federal University Gusau, Nigeria
4Department of Microbiology, Kano University of Science and Technology Wudil Kano, Nigeria
*Corresponding Author: Muhammad Ali, Department of Biological Sciences, Federal University Gusau, Nigeria. Email: alimuhd4real@gmail.com
Receive: September 14, 2018; Published: September 22, 2018
Abstract
Malaria in pregnancy is a major public health problem in endemic areas of sub-Saharan Africa and has significant consequences on birth outcome. This research work was carried out between May and August, 2017 in Ante- Natal clinic, Federal Medical Center, Birnin Kudu, Jigawa State, Nigeria. A total of 406 blood samples were collected from the pregnant women. Malaria parasites were examined microscopically on thick and thin blood smear stained with Giemsa stain, personal data were collected orally and from file records and were analyzed using Chi-square test. The results showed that of 406 pregnant women sampled, 219 (53.9%) were positive for Plasmodium falciparum. The highest prevalence of P. falciparum (79.8%) was observed in ages 15-20 pregnant women while the lowest prevalence of (21.6%) was found in ages 41-45. Statistical analysis showed a significant difference in between the various age groups (P<0.05). Multigravidae pregnant women recorded higher prevalence of (54.7%) while (52.5%) prevalence was observed in primigravidae. Women in the second trimester were more infected with P. falciparum (43.8%) than those in first trimester (26.5%) and third trimester (29.7%) and this was not significant (P>0.05). Malaria infection showed a high level of endemicity in the study area, hence, there is need for prompt treatment offered to pregnant women, encourage the use of insecticide -treated bed nets and to incorporate the laboratory components into the RBM strategy by enhancing parasite diagnosis at all levels of health care.
Keywords: Birnin Kudu; Gravidity; Pregnant women; Prevalence; Plasmodium falciparum
Introduction
Malaria is a preventable and treatable infectious disease, which is transmitted through the bites of infected female anopheles mosquitoes. Malaria is caused by a protozoan parasite of the genus Plasmodium, four species namely; Plasmodium vivax, P. ovale, P. malariae and P. falciparum are responsible for human malaria [1]. P. falciparum accounts for about 80% morbidity and 90% mortality in humans [2], its common symptoms include headache, weakness, fever, pains, high body temperature (chills and rigors), bitterness of mouth and loss of appetite [3]. In children, additional symptoms include more than sleeping, nausea and vomiting.
Malaria kills more than one million people every year, most of them in Sub Saharan Africa, where malaria is a leading cause of death for children under five years and pregnant women [4]. However, the current status as reported by WHO [5] was 219 million cases in 2010. That year between 660,000 and 1.2 million people died from the disease (roughly 2000-3000 per day [6]. In Sub Saharan Africa, malaria in pregnancy is predominantly asymptomatic and yet a major cause of severe maternal anaemia and low birth weight babies strongly associated with marked increase in infant mortality [7].
Malaria is endemic in Nigeria and its existence is well recognized and surveys reporting the prevalence in various communities in Nigeria [8-10]. Available records show that at least 50 percent of the population of Nigeria suffers from at least one episode of malaria each year [11]. High level of malaria endemicity, parasite resistance to affordable drugs and inadequate access to treatment facilities has contributed to making the disease the leading killer of children, accounting for an estimated 300,000 deaths each year. Many researchers have reported high prevalence rates of malaria in pregnancy in different parts of the country, ranging from 19.7% to 72.0% [12], with anaemia, pregnancy miscarriages and low birth weight of babies identified as the most debilitating effects of the disease which accounts for 11% of maternal deaths in the country [13]. Pregnant women are 3 times more likely to suffer from severe disease as a result of malarial infection compared with their non-pregnant counterparts, and have a mortality rate from severe disease that approaches 50% [14,15]. In endemic areas, acquired immunity, though established is liable to break down the conditions of stress, in pregnant women. During pregnancy, there are usually high protein requirement and if dietary intake is insufficient, metabolic channels may be altered to withdraw protein from the immune system, hence the low the immunity in pregnant women [16]. Fetal and prenatal mortality, which sometimes lead to premature and false labour, occur in malarious mothers, although the incidence of preterm delivery is significantly increased only in non-immune mothers or those with low level of acquired immunity. Different studies have shown that malaria infection is more prevalent in primigravidae than in multigravidae [17,18].
Transmission of malaria is intense and stable in Nigeria because the intensity of attack remains constant throughout the year or from year to year. The degree of endemicity of malaria measured is based on the spleen rate in children aged 2-9 years as published by World Health Organization (WHO) in order of severity. Hypoendemic malaria occurs when spleen rate in children is less than 10%, Mesoendemic occurs when the spleen rate is 11-50% in children, Hyperendemic occurs when spleen rate is 75% in children and greater than 25% in adults while Holoendemic occurs when spleen rate is greater than 75% in children but very low in adults. Malaria is holoendemic in Nigeria, with Plasmodium falciparum accounting for ninety five percent of all infections in the country [12]. Due to the terminal form of the malaria infection in the country, we studied the prevalence of the disease in pregnant women in ante- natal clinic of Federal Medical Center, Birnin Kudu, Jigawa State, Nigeria.
Materials and Methods
The Study Area and Population
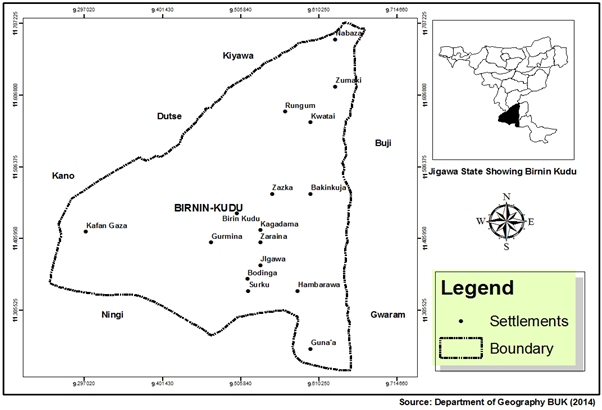
Birnin Kudu is a small town and a Local Government Area in the south of Jigawa State, Nigeria (Figure 1). The Local Government Area is located 41Km from the state capital and some 120Km south-east of Kano [19]. It is situated at 11.45° North latitude, 9.5° East longitude and 474m elevation above the sea level [20]; and has an estimated population of 313,373 [21]. The climate is semi-arid, characterized by long dry season and short wet season. The climatic factors vary considerably over the year and are sharply inconsistent. The temperature out regime is warm to hot. The mean annual temperature is about 25°C but the mean monthly values range between 21°C in the coolest month and 31°C in the hottest month. Wet season is roughly four months (June to September) and dry season is seven to eight months (October to May). The rainy season may commence in May, but early rains in April are most common. The bulk of the rainfall comes in June through September. Violent dust storms are usually accompanied by tornadoes and lightening, which usually precede the onset of the rains in May/June and their retreat in September or earlier than that [22]. Most of the state falls within the in Sudan Savannah vegetation belt, but traces of Guinea savannah vegetation are found in parts of the southern districts. Extensive open grasslands, with few scattered stunted trees, are characteristics of the vegetation. The ecology of Birnin Kudu provides suitable breeding sites for biological multiplication, development and high survival rate of female Anopheles mosquito vectors for the transmission of malaria parasite to the populace. The major occupation of the inhabitants is farming, Cattle rearing and fishing
Birnin Kudu is a small town and a Local Government Area in the south of Jigawa State, Nigeria (Figure 1). The Local Government Area is located 41Km from the state capital and some 120Km south-east of Kano [19]. It is situated at 11.45° North latitude, 9.5° East longitude and 474m elevation above the sea level [20]; and has an estimated population of 313,373 [21]. The climate is semi-arid, characterized by long dry season and short wet season. The climatic factors vary considerably over the year and are sharply inconsistent. The temperature out regime is warm to hot. The mean annual temperature is about 25°C but the mean monthly values range between 21°C in the coolest month and 31°C in the hottest month. Wet season is roughly four months (June to September) and dry season is seven to eight months (October to May). The rainy season may commence in May, but early rains in April are most common. The bulk of the rainfall comes in June through September. Violent dust storms are usually accompanied by tornadoes and lightening, which usually precede the onset of the rains in May/June and their retreat in September or earlier than that [22]. Most of the state falls within the in Sudan Savannah vegetation belt, but traces of Guinea savannah vegetation are found in parts of the southern districts. Extensive open grasslands, with few scattered stunted trees, are characteristics of the vegetation. The ecology of Birnin Kudu provides suitable breeding sites for biological multiplication, development and high survival rate of female Anopheles mosquito vectors for the transmission of malaria parasite to the populace. The major occupation of the inhabitants is farming, Cattle rearing and fishing
Ethical Consideration
Prior to data collection, ethical clearance was taken from the State Ministry of Health and from the Chief Medical Director of Federal Medical Center Birnin Kudu, Jigawa State, Nigeria. The oral consent of each pregnant women sampled was also sought before commencing this study. Four Hundred and Six pregnant women who visited the ante-natal clinic of Federal Medical Center, Birnin Kudu were involved. Structured Questionnaire were distributed to and completed by the pregnant women to obtain information such as age, stage of pregnancy, gravidity and bio-data. Pregnant women who could not read or write where assisted in filling their questionnaires.
Prior to data collection, ethical clearance was taken from the State Ministry of Health and from the Chief Medical Director of Federal Medical Center Birnin Kudu, Jigawa State, Nigeria. The oral consent of each pregnant women sampled was also sought before commencing this study. Four Hundred and Six pregnant women who visited the ante-natal clinic of Federal Medical Center, Birnin Kudu were involved. Structured Questionnaire were distributed to and completed by the pregnant women to obtain information such as age, stage of pregnancy, gravidity and bio-data. Pregnant women who could not read or write where assisted in filling their questionnaires.
Sample collection and Examination
Sample collection was done between May and August, 2017. Samples were collected under the supervision of a trained laboratory technician. 2ml venous blood was collected from both groups using tourniquet tied to the upper arm after cleaning of the spot, blood samples were collected and emptied into anticoagulant specimen bottles. Both thin and thick blood films were stained with 0.5ml of Leishman’s solution for 30 minutes as recommended by WHO and examined for malaria parasites by standard method. Venous blood samples were collected using a tubing tourniquet tied to the upper arm of each of the children with care and adequate safety precautions to ensure test result are reliable, contamination of the samples was avoided and infection from blood transmissible pathogens was also prevented. Protective gloves were worn when collecting and handling blood samples. The blood samples were collected into EDTA bottle/container which was labelled with information such as name of the child, sex and age; and mixed gently. This anticoagulant (EDTA) is commonly used for haematological test. The chemicals therein, prevent blood from clotting by removing calcium [23].
Sample collection was done between May and August, 2017. Samples were collected under the supervision of a trained laboratory technician. 2ml venous blood was collected from both groups using tourniquet tied to the upper arm after cleaning of the spot, blood samples were collected and emptied into anticoagulant specimen bottles. Both thin and thick blood films were stained with 0.5ml of Leishman’s solution for 30 minutes as recommended by WHO and examined for malaria parasites by standard method. Venous blood samples were collected using a tubing tourniquet tied to the upper arm of each of the children with care and adequate safety precautions to ensure test result are reliable, contamination of the samples was avoided and infection from blood transmissible pathogens was also prevented. Protective gloves were worn when collecting and handling blood samples. The blood samples were collected into EDTA bottle/container which was labelled with information such as name of the child, sex and age; and mixed gently. This anticoagulant (EDTA) is commonly used for haematological test. The chemicals therein, prevent blood from clotting by removing calcium [23].
Thin/Thick Blood Film preparation and parasitological examination
The laboratory method employed for staining and identification of malaria parasites in collected blood samples was as described by Cheese rough [23]. Both thick and thin films were prepared. A small drop of blood was placed on a clean microscopic slide near the end of a slide, a spreader was used to smear a blood steadily across the slide in a steady even movement at an angle of 45° and the slide was allowed to dry and labeled appropriately. One [1] volume of Giemsa stain was flooded on the slide for few minutes, two [2] volumes of buffered distil water of PH 6.8 was added and left for further 10 minutes, the slide was washed thoroughly under tap water to differentiate (the colour should be salmon pink), the slide was left to dry and back of the slide was clean with cotton wool soaked in alcohol. A drop of oil immersion was placed on a stained slide to cover about 10mm in diameter in the areas of the film and viewed with the (X100) objective of compound microscope in order to identify the plasmodium parasites [23]. Positive or negative results were recorded accordingly.
The laboratory method employed for staining and identification of malaria parasites in collected blood samples was as described by Cheese rough [23]. Both thick and thin films were prepared. A small drop of blood was placed on a clean microscopic slide near the end of a slide, a spreader was used to smear a blood steadily across the slide in a steady even movement at an angle of 45° and the slide was allowed to dry and labeled appropriately. One [1] volume of Giemsa stain was flooded on the slide for few minutes, two [2] volumes of buffered distil water of PH 6.8 was added and left for further 10 minutes, the slide was washed thoroughly under tap water to differentiate (the colour should be salmon pink), the slide was left to dry and back of the slide was clean with cotton wool soaked in alcohol. A drop of oil immersion was placed on a stained slide to cover about 10mm in diameter in the areas of the film and viewed with the (X100) objective of compound microscope in order to identify the plasmodium parasites [23]. Positive or negative results were recorded accordingly.
Statistical Analysis
The prevalence of parasites was presented as descriptive statistics while the relationship between several variables and the presence of parasites was determined using Chi square test Chi-square at 5% level of significance (P˂0.05 was considered significant). The data analysis was performed using statistical programme for social sciences (SPSS) version.
The prevalence of parasites was presented as descriptive statistics while the relationship between several variables and the presence of parasites was determined using Chi square test Chi-square at 5% level of significance (P˂0.05 was considered significant). The data analysis was performed using statistical programme for social sciences (SPSS) version.
Results
Out of the 406 samples collected from the pregnant women, 219 (53.9%) were infected with P. falciparum (tables 1, 2 and 3). From the age groups of the pregnant women sampled, it was observed that the age group between 15-20 years had the highest prevalence of P. falciparum infection 71 (79.8%) while least prevalence was observed in age group between 41-45 years with 11(21.6%). Chi-square analysis revealed that there is a significant difference (p<0.05) in the prevalence of P. falciparum infection among the age group (Table 1).
| Age Group (Years) | No. Examined | No (%) Infected |
| 15-20 | 89 | 71 (79.8) |
| 21-25 | 79 | 53 (67.1) |
| 26-30 | 67 | 38 (56.7) |
| 31-35 | 62 | 28 (48.2) |
| 36-40 | 58 | 18 (31.0) |
| 41-45 | 51 | 11 (21.6) |
| Total | 406 | 219 (53.9) |
Table 1: Prevalence of Plasmodium falciparum according to age of pregnant women in the study area.
Of the 141 primigravidae sampled, 74 (52.5%) were infected with malaria parasite while the highest prevalence of 145 (54.7%) was recorded from 265 multigravidae sampled (Table 2). However, statistical analysis showed that there was no significant difference (p>0.05) in the prevalence of malaria parasites according to parity.
| Pregnancy Gravidity | No. Examined | No (%) Infected |
| Primigravidae | 141 | 74 (52.5) |
| Multigravidae | 265 | 145 (54.7) |
| Total | 406 | 219 (53.9) |
Table 2: Prevalence of Plasmodium falciparum according to pregnancy gravidity of women in the study area.
As for the gestational periods (Table 3), the highest prevalence of 96 (43.8%) of P. falciparum infection was recorded among women in second trimesters; followed by those in third and first trimesters with prevalence of (29.7%) and (26.5%), respectively. Chi-square analysis revealed a significant difference in the trimesters (p < 0.05).
| Trimester | No. Examined | No (%) Infected |
| First | 67 | 58 (26.5) |
| Second | 209 | 96 (43.8) |
| Third | 130 | 65 (29.7) |
| Total | 406 | 219 (53.9) |
Table 3: Prevalence of Plasmodium falciparum according to trimester among women in the study area.
Discussion
This study revealed that malaria parasite was prevalent in Federal Medical Center, Birnin Kudu. P. falciparum was the only species observed; which also had been confirmed earlier as the predominant species in Sub Saharan Africa by WHO [5]. The present study revealed that the prevalence of P. falciparum malaria varied considerably between ages, gravidity, trimester of the pregnant women screened. The prevalence of 53.9% of P. falciparum observed in the blood sample of pregnant women in this study is slightly higher than those of Egwunyenga., et al. [24] who recorded 36.2% in studies carried out in Jos, Bauchi and Eku regions of Nigeria and almost closer to the findings of Boyou., et al. [25], Okwa., et al. [12], Nduka., et al. [26] Iwueze., et al. [22] which recorded 57.5%, 60.0%, 54.0% and 58.0% in Gabon, Lagos State, Nigeria, South East Nigeria and Anambra State, Nigeria, respectively; as well a much higher prevalence of 72% reported by Singh., et al. [27] in India and Akinboye., et al. [28] in Oyo State, Nigeria.
The relatively higher prevalence of malaria infection in this study may be attributed to the high level of illiteracy, traditional believes, lack of personal engagement of the population to fight malaria, the climate which influence the development of mosquito larvae, human behaviour and the presence Anopheles gambien and Anopheles funestus which are anthropophilic and consequently, are said to be the most efficient in the world [29]. All these factors promote the spread of malaria infection. The presence of P. falciparum infection in this study is not surprising as it was reported that falciparum malaria infection mostly occur in the Sub-Saharan Africa and also has been shown to be more common in pregnant women than non- pregnant women [30]. The results of this study has further confirmed to the fact that the epidemiology of malaria parasite is dependent on seasons of the year. This observation is in accordance with the work of Emerton [31], Amadi and Abenezer [32], Yahaya., et al. [33] and Yakudima., et al. [34] who reported that the highest infection rate of the disease occurred during the peak of rainy season when there were abundance of Anopheles mosquito vectors in the transmission of the parasite.
It was observed from the results that pregnant women of all age group were infected with P. falciparum malaria. However, the significantly higher infection rate of malaria recorded in the age group between 15-20 years compared to other age group could be due to the fact that the younger age groups have less contact with the mosquito vector than the other age groups and therefore, their immunity is not as well developed as others. This also confirmed that as women get older, their resistance to malaria becomes higher due to improvement in host immunity. This result is closely similar to that of McGregor., et al. [35] in Gambia, West Africa who reported a decline in prevalence of malaria infection as age increase and that with improved host immunity, thus reducing susceptibility in later years; as well as the reports of Desai., et al. [36] in Sub-Saharan Africa; Kolawole., et al. [37] in Ilorin, Kwara State, Nigeria; Falade., et al. [38] in Ibadan, South Western Nigeria; Banao., et al. [39] in Maradi, Niger Republic and Iwueze., et al. [22] in Anambra State, Nigeria who recorded higher infection rate in age group <21, but disagrees with the works of Adefioye., et al. [40] in Oshogbo, Nigeria who found higher prevalence of malaria in between age group of 36-39.
The higher prevalence of P. falciparum infection in multigravidae than in primigravidae recorded in this study may be as a result of lack of specific immunity to malaria infection and the immunological changes in host during pregnancy or due to low level of Antibodies against Variant Surface Antigen (VSA). This result corroborates the works of Campos., et al. [41] in Luanda, Angola and Isa., et al. [42] in Maiduguri, Borno State, Nigeria where the multigravidae had the highest prevalence of malaria infection. However, this result disagrees with the findings of McGregor., et al. [35]; Sketelie., et al. [43]; Anorlu., et al. [44]; Opare-Ado and Odoi [45]; Zhou., et al. [46]; Desai., et al. [36]; Schanz- Dunn and Nour [47]; Akanbi., et al. [17]; Amali., et al. [48]; Wogu., et al. [49]; Ibecheozor and Peletri [50]; Bedu-Ado., et al. [18] and Ebenezer., et al. [51].
The significantly higher prevalence of falciparum malaria parasite recorded among pregnant women in their second trimester than other trimesters in this study is in agreement with the works of Schanz- Dunn and Nour [47]; Amali., et al. [48] in Makurdi, Benue State, Nigeria and Isa., et al. [42] in Maiduguri, Borno State, Nigeria and Inah., et al. [52] in Abi Local Government Area, Cross River State, Nigeria, but disagree with the reports of Brabin [16] in Western Kenya, Desai., et al. [36] in Sub- Saharan Africa and Houmsou., et al. [20] in Nigeria, who reported that pregnant women in their first trimester had higher prevalence of malaria infection as well as the reports of Alnonghol., et al. [53] and Ebenezer., et al. [51] who indicated high prevalence in third trimester. Chi-square analysis revealed that there is a significant difference between the first, second and third trimesters.
Conclusion
The result of this study indicated that there is active transmission of malaria which indeed constitutes a public health problem in the study area. The high prevalence observed, might be attributed to the period of study (May-August) which is within the period of maximum rainfall in Nigeria. Therefore, Relevant government agencies should ensure that Insecticide-Treated Bed Nets (ITNs) are made available free to every pregnant woman. Appropriate antimalarial drugs for treatment should be given free to all malaria positive pregnant women. Community participation and health education strategies, promoting awareness of malaria and the importance of control measures aimed at reducing the incidence of malaria in our environment should be encouraged through media advocacy and during ante- natal care hours. Proactive steps such as cleaning of waterways, avoiding stagnant pools, maintaining a healthy environment condition (which discourages the breeding of mosquitoes) and other effective malaria control strategies would all have a synergistic effect in controlling malaria infection among pregnant women.
Acknowledgements
We are greatly thankful to the Chief Medical Director, Nursing and Laboratory staff of the Center for their valuable contribution and assistance throughout this study. We thank the patients for their interest and cooperation.
We are greatly thankful to the Chief Medical Director, Nursing and Laboratory staff of the Center for their valuable contribution and assistance throughout this study. We thank the patients for their interest and cooperation.
References
- Ekanem OJ., et al. “Sensitivity of Plasmodium falciparum to chloroquine and Sulphadoxine/ Pyrimethamine in Nigeria Children”. Bulletin of World Health Organization 68.1 (1990): 45-52.
- Carter JA., et al. “Development impairment following severe falciparum malaria in children”. Tropical Medicine International Health 10 (2005): 3-10.
- Jimoh A., et al. “Quantifying the economic burden of infection in Nigeria using the willingness to pay approach”. Journal of Cost Effective and Resource Allocation 5(2007): 5-6.
- “World Health Organization. Blood Transfusion Safety. Regional Meeting of Directors of Blood Transfusion Services Sharja, United Emirates. World Health Organization, Information Sheet.” (2008): 15-17.
- “World Health Organization. Strategic Framework for Malaria Control during pregnancy in the Africa Region. Geneva, World Health Organization.” (2003).
- Nayyar GML., et al. “Poor quality antimalarial drugs in Southeast Asia and Sub Saharan Africa”. Lancet Infectious Diseases 12 (2012): 488-496.
- Okwa OO. “Preliminary Investigation on malaria in Sickle cell patients among pregnant women and infants in Lagos, Nigeria”. Nigeria Journal of Parasitology 25 (2004): 81-85.
- Epid TT., et al. “Prevalence of malaria in blood donors in Abakaliki metropolis, Nigeria”. Scientific Research and Essay 3.4 (2008): 162-164.
- Onyido AE., et al. “Malaria burden and vector abundance in Sub Urban Community in the rainforest zone of Nigeria”. Nigerian Journal of Microbiology 24.1 (2010): 2224-2230.
- Opara AU., et al. “Prevalence of malaria among rural farmers of North Central Area of Ebonyi State Nigeria”. International Science Research Journal 3 (2011): 29-33.
- Ejezie GC., et al. “Malaria and its retreatment in rural villages of Aboh Mbaise, Imo State, Nigeria”. Acta Tropica 48 (1991): 17-24.
- Okwa OO., et al. “Transmission dynamics of malaria in four selected ecological zones of Nigeria in the rainy season”. Annals African Medicine 8 (2009): 1-9.
- “Federal Ministry of Health”. Malaria situation analysis document. Federal Ministry of Health; (2000): 14.
- Monif GRG., et al. “Infectious Disease in Obstetrics and Gynecology. 6th edition”. New York: Parthenon (2004): 280-286.
- “World Health Organization. Guidelines for the Treatment of Malaria. Geneva: World Health Organization” (2006).
- Brabin BJ. “An Analysis of Malaria in Pregnancy in Africa.” Bulletin of the World Health Organization 61.6 (1983): 1005-1016.
- Akanbi OM., et al. “Role of malaria induced stress on anaemia in pregnancy”. Asian Pacific Journal of Tropical Medicine 3 (2010): 211-214.
- Bedu- Ado., et al. “Reduced Prevalence of placental malaria in Primiparae with blood group O”. Malarial Journal 13 (2014): 289.
- Fleming AF., et al. “Malaria and Haemoglobin genotype in young Northern Nigeria children.” Annals of Tropical Medicine and Parasitology 79 (1985): 1-5.
- Houmsou RS., et al. “Malarial infection in HIV Infected Pregnant women attending a rural Antenatal Clinic in Nigeria”. Advances in Epidemiology 14(2014): 5-11.
- Ikeh EI., et al. “The prevalence and intensity of malaria parasite in children at Jos University Teaching Hospital, Nigeria”. Highland Medical Research Journal 1(2002): 9-10.
- Iwueze MO., et al. “Prevalence, Intensity and Clinical profile of malaria among pregnant women attending antenatal clinics in Onitsha North Local Government Area, Anambra State, Southern Nigeria”. The Bio scientist 2.1 (2014): 17-19.
- Cheesbrough M., “Medical Laboratory Manual for Tropical Countries.” Part 2, 2nd edition, University Press Cambridge (2000): 454.
- Egwunyenga AO., et al. “Plasmodium/Intestinal helminthes co-infection among pregnant Nigeria women". Mem Instr Oswaldo Cruz: 96.8(2001): 1055-1059.
- Boyou-Akotet MK., et al. “Prevalence of Plasmodium falciparum infection in pregnant women in Gabon”. Malaria Journal 2(2003): 18-24.
- Nduka FO., et al. “Prevalence of malaria parasites and anaemia in pregnant and non - pregnant women in Aba and Okigwe towns of Southeast Nigeria”. Animal Research International 3.3(2006): 508-512.
- Singh N., et al. “Epidemiology of malaria in pregnancy in Central India”. Bulletin of the World Health Organization 77.7(1999): 567-572.
- Akinboye DO., et al. “The Influence of Malaria on some Haemotological Parameters in Pregnancy”. Nigerian Journal of Parasitology 32.2 (2011): 187-191.
- “Centre for Disease Control and Prevention. Biology: Anopheles Mosquitoe”. 404 (2008): 639-3534.
- “Chemical Microbiology Reviews. Impact of malaria during pregnancy on low birth weight in Sub-Saharan Africa”. American Society of Microbiology 17.4 760-769.
- Emerton GD., “An Audit of the mManagement of Malaria in Tanzania District Hospital”. Transactions of the Royal Society of Tropical Medicine and Hygiene 86(1992): 76-478.
- Amadi., et al. “Prevalence of Haemoparasitic Infections in Humans and Insect Vectors in Yenagoa, Bayelsa State, Nigeria”. Jouurnal of Parasitology 29.2 (2009):131-135.
- Yahaya A., et al. “Seasonal Variation of Malaria Infection among Out-Patients Attending Wudil General Hospital, Kano State, Nigeria”. International Journal of Applied Research and Technology 1.7(2012): 79-84.
- Yakudima II., et al. “Retrospective Study of Seasonal Trends of Malaria reported cases in Kano State Nigeria”. Bayero Journal of Pure and Applied Sciences 10.2 (2017): 238-244.
- Mcgregor IA. “Malaria Infection of the Placenta in the Gambia West Africa.” Transactions of the Royal Society Tropical Medicine and Hygiene. 77: (1983) 232-244.
- Desai M., et al. “Epidemiology and burden of malaria in pregnancy”. Lancet infectious Diseases 7(2007): 93-104.
- Kolawole OM., et al. “Some Biochemical and Haematological Studies on the Prevalence of Congen ital Malaria in Ilorin, Nigeria”. Biochemistry 19.2(2007): 59-64.
- Falade CO., et al. “Intermittent preventive treatment with Sulfadoxine Pyramethamine is effective in preventing maternal and placental malaria in Ibadan, South Western Nigeria”. Malaria Journal 6(2007): 88.
- Banao TO., et al. “The prevalence of malaria among pregnant women in Maradi, Niger Republic”. Nigerian Journal of Parasitology 31.1(2010): 31-34.
- Adefioye OA., et al “Prevalence of Malaria Infection among pregnant women in Osogbo South West Nigeria”. American- Eurasian Journal of Scientific Research 2.1 43-45.
- Campos PC., et al. “Plasmodium falciparum infection in pregnant woman attending antenatal care in Luanda, Angola.” (2012).
- Isa MS., et al. “Prevalence of malaria parasite infection among pregnant women ante-natal clinic in State Specialist Hospital, Maiduguri, Borno State, Nigeria”. Biosciences Research Health Medical Perspective Abstract”.
- Stekelie RW., et al. “The burden of Malaria in pregnancy in malaria endemic areas”. American Journal of Medicine and Hygiene 64.1 (2001): 28-35.
- Anorlu RJ., et al. “Asymptomatic malaria parasitemia in pregnant women at booking in a primary health care facility in a peri-urban community in Lagos, Nigeria”. African Journal of Medical Sciences 30 (2001): 39-41.
- Opare-Ado HS., et al. “Malaria in pregnancy. In: Kwawukume, E. Y., Emuweyan, E. E., Editors. Comprehensive Obstetrics in the tropics, 1.” First ed. Accra, Ghana: Asante and Hittscher Printing Press Publishers. (2002): 250- 260.
- Zhou A., et al. “Prevalence of Plasmodium falciparum infection in pregnant Cameroonian women”. American Journal of Tropical Medicine and Hygiene 67.6 (2002): 566-570.
- Schanz-Dunn J., et al. “Malaria and Pregnancy: A global health Perspective”. Reviews in Obsterics and Gynecology Summer 3 (2009): 183-192.
- Amali O., et al. “Malaria and Anaemia among pregnant women in Makurdi Benue State”. The Nigerian Journal of Parasitology 32.2 (2011): 93-196.
- Wogu MN. “Prevalence of malaria parasite infections among women attending ante-natal clinic in Port Harcourt, River State, Nigeria”. International Journal of Tropical Health and Diseases 3.2 (2003):126-132.
- Ibecheozor NKO., et al. “Malaria in pregnancy; facts from Parasitology laboratory: a ten year study in Abuja. North Central Nigeria”. International Journal of Mosquito research1.3 (2014): 10-14.
- Ebenezer A., et al. “Patterns of Plasmodium falciparum Malaria among Pregnant women Attending Antenatal Clinics in the Communities along the Epie Creek, Bayelsa State, Nigeria”. Annals of Biological Research 7.6 (2016): 1-5.
- Inah SA., et al. “Prvalence of Malaria among Pregnant Women and Children under Five years in Abi Local Government Area, Cross River State, Nigeria”. Asian Journal of Medicine and Health 17.1 (2017): 1-17.
- Alnongzhol BM., et al. American Journal of Tropical Medicine and Hygiene 67.6(2002): 566-570.
Citation:
Abdullahi Yahaya., et al. “Plasmodium Falciparum Malaria Among Pregnant Women Attending Ante - Natal Clinic, Federal
Medical Center, Birnin Kudu, Jigawa State, Nigeria”. Chronicles of Pharmaceutical Science 3.1 (2018): 745-752.
Copyright: © 2018 Abdullahi Yahaya., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.