Research Article
Volume 3 Issue 2 - 2019
Socio-demographic & Clinical Profile of Patients with Substance Use Disorders Seeking Treatment. A Hospital Based Study
1Lecturer department of Psychiatry SKIMS Medical College Bemina
2Professor & Head department of Psychiatry SKIMS Medical College Bemina
3Senior Resident department of Psychiatry SKIMS Medical College Bemina
4Medical officer Department of Health and medical education.
5Associate Professor Department of Psychiatry SKIMS Medical College Bemina
6Senior Resident department of Psychiatry SKIMS Medical College Bemina
7Clinical Psychologist department of Psychiatry SKIMS Medical College Bemina
2Professor & Head department of Psychiatry SKIMS Medical College Bemina
3Senior Resident department of Psychiatry SKIMS Medical College Bemina
4Medical officer Department of Health and medical education.
5Associate Professor Department of Psychiatry SKIMS Medical College Bemina
6Senior Resident department of Psychiatry SKIMS Medical College Bemina
7Clinical Psychologist department of Psychiatry SKIMS Medical College Bemina
*Corresponding Author: Ajaz Ahmad Suhaff, senior Resident Deptt of Psychiatry SKIMS Medical College Bemina.
Received: April 29, 2019; Published: May 08, 2019
Abstract
Substance abuse is a complex and multidimensional problem. The problem is not merely that of an individual and a drug or a community, but of the interaction between the triad. The geographical location of Jammu and Kashmir makes transit of drugs possible across the state. Present prevailing disturbed conditions have worsened drug abuse scenario besides phenomenal increase in other psychiatric disorders in Kashmir. Drug addiction, a major problem worldwide, is associated with a high risk of relapse. Substance use can influence the support extended by the family members. This may be due to financial difficulties posed by the drug use, drug use leading to neglect of family responsibilities, involvement of the drug abuser in illegal activities, aggressive behavior that may occur under the influence of certain drugs or several other reasons.
Aims and Objectives: To study the demographic profile of patients with substance use disorders seeking treatment & the clinical profile of patients with substance use disorders seeking treatment.
Material and Methods: Study was undertaken on the patients with substance use disorders attending OPD of Government Psychiatric Disease Hospital, Government Medical College Srinagar Kashmir, which is a teaching hospital for both under and postgraduate students. First 300 consecutive patients attending psychiatric OPD with substance use disorders as per DSM-IV-TR criteria diagnosed by the consultant psychiatrist, were taken for the study. A detailed history of sociodemographic and clinical profile was taken as per the proforma. In case of any doubt about the nature of the drug abused the urine screening was done. All other routine investigations like CBC, LFT including gamma GT, KFT, serum electrolytes and blood sugar were also done. In our study majority of the patients were males, unmarried, with the mean age at time of presentation was 28.99 years, resident of urban and semi urban areas, Muslims, came from nuclear family, belonging to the middle class family. The most common reason for seeking treatment for substance use disorder was social problems, with the mean age of onset of substance use was 19.66 years. A significant number of patients 32.34% (N=97) were using more than one substance. Most common route of administration used by the patients in our study was oral 57.91%. Among the psychiatric comorbidity, patients with Major Depressive Disorder (MDD) were 32.06 %( N=42), Bipolar Affective Disorder (BPAD) were 31.29 %( N=41), anxiety and adjustment disorders were 27.48% (N=39). Out of the 300 patients only 13% (N=39) of the patients had previous history of hospitalization or treatment for substance abuse.
Conclusion: Most of the treatment seekers who attended the hospital for the substance use disorders were males in adult age group and most of them started using substance in adolescence. Bulk of the treatment seekers in our study was formed by businessmen, employees, students; most of which belonging to the nuclear family. Maximum were having good social support and referred by the family. Predominant substances used were opioids derivatives, cannabis, benzodiazepines and alcohol with significant number of polysubstance abusers using mostly opioid and benzodiazepine combination. So opioid derivative use is showing increasing trend in the treatment seekers in the valley. About forty three percent of the substance use disorders were having comorbid psychiatric disorder and more than one third having suicidal ideation although suicidal attempts were very less. Many of the patients were having high risk behavior, 9.34% percent were the parental drug users and 2.67% shared the needles and 19% of the patients had multiple sexual partners, 6.67% had sex with commercial sex worker. Both of these high risk behaviors form the fertile ground for the spread of deadly disease AIDS and other life threatening diseases.
Introduction
Substance abuse is a complex and multidimensional problem. The problem is not merely that of an individual and a drug or a community, but of the interaction between the triad [1]. Continuous discovery of new drugs has no doubt brought relief in the treatment of hitherto incurable conditions and saved thousands of lives, but most of these drugs have also adverse effects, if not judiciously used. India, the traditional drugs like opium, charas, bhang and ganja were used by sections of the society partly as leisure time activity and partly as part of the religious ceremony. Therefore, their consumptions did not invite much negative sanction from the society. Abuse of alcoholic beverages are endemic in many societies, whilst the abuse of other psychoactive substances present in epidemic features and drug abuse is transmitted from person to person like an infectious disease[2]. No effective treatment and prevention related policy issues can be arrived at without adequate information regarding the nature and distribution of drug abuse in population and their causative factors. The geographical location of Jammu and Kashmir makes transit of drugs possible across the state. Present prevailing disturbed conditions have worsened drug abuse scenario besides phenomenal increase in other psychiatric disorders in Kashmir [3]. Treatment services utilization by substance abusers is one of the sources and indicators of assessing problematic substance use. It is important to assess treatment demand from substance abusers and can be an effective tool for preliminary assessment of magnitude and pattern of substance abuse in the community [4]. Therefore, studying the profile of substance abusers in the hospital can act as tool to have an idea about the nature of substance abuse in the community and help to create a baseline data about substance abuse in Kashmir and nearby areas served by the hospital.
Drug addiction, a major problem worldwide, is associated with a high risk of relapse. Substance use can influence the support extended by the family members. This may be due to financial difficulties posed by the drug use, drug use leading to neglect of family responsibilities, involvement of the drug abuser in illegal activities, aggressive behavior that may occur under the influence of certain drugs or several other reasons. The substantial burden imposed on the family containing a member with substance use disorder and the impact of family interactions in perpetuating or ameliorating these problems have an effect on the initiation of, perpetuation of and recovery from the substance use disorder; the patient's motivation and ability to comply with treatment; and the patient's clinical course and outcome[5]. Social support influences motivation, treatment compliance and outcome in drug dependent patients. Substance abuse can influence social support and social support, in turn, can influence the substance abuse problem [6].
Aims and Objectives:-
To study
1. The demographic profile of patients with substance use disorders seeking treatment.
2. The clinical profile of patients with substance use disorders seeking treatment.
To study
1. The demographic profile of patients with substance use disorders seeking treatment.
2. The clinical profile of patients with substance use disorders seeking treatment.
Material and Methods
- Setting; Study was undertaken on the patients with substance use disorders attending OPD of Government Psychiatric Disease Hospital, Government Medical College Srinagar Kashmir, which is a teaching hospital for both under and postgraduate students.
- Method; First 300 consecutive patients attending psychiatric OPD with substance use disorders as per DSM-IV-TR criteria diagnosed by the consultant psychiatrist, were taken for the study. A detailed history of sociodemographic and clinical profile was taken as per the proforma. In case of any doubt about the nature of the drug abused the urine screening was done. All other routine investigations like CBC, LFT including gamma GT, KFT, serum electrolytes and blood sugar were also done.
- Measures: The following measures were considered in the study. 1. Sociodemographics:
2. Clinical profile:
D. Inclusion criteria;
1. The patient with substance use disorders who gave the consent.
2. 16 to 65 years of age.
1. The patient with substance use disorders who gave the consent.
2. 16 to 65 years of age.
E. Exclusion criteria;
1. Patients who did not gave consent.
2. Age <16yrs or >65 yrs.
3. Patients with organic brain disorders
4. Patients with medical conditions to cause psychiatric disorders like hypothyroidism, pheochromocytoma, epilepsy, cushing’s disease etc.
1. Patients who did not gave consent.
2. Age <16yrs or >65 yrs.
3. Patients with organic brain disorders
4. Patients with medical conditions to cause psychiatric disorders like hypothyroidism, pheochromocytoma, epilepsy, cushing’s disease etc.
Observations and Results
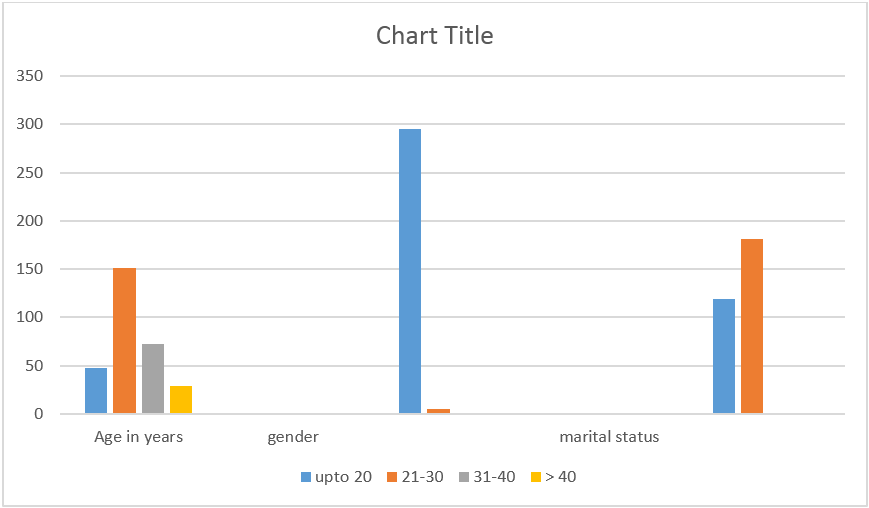
| Age(years) at the time of presentation | ||
| Age range | No. Of patients | Percentage |
| UPTO 20 | 48 | 16 |
| 21-30 | 151 | 50.33 |
| 31-40 | 72 | 24 |
| ›40 | 29 | 9.67 |
| Marital Status | ||
| MARRIED | 119 | |
| UNMARRIED | 181 | |
| GENDER | ||
| MALES | 295 | |
| FEMALES | 5 | |
| RESIDENCE | ||
| URBAN | 138 | |
| SEMI-URBAN | 61 | |
| RURAL | 101 | |
| RELIGION | ||
| MUSLIM | 281 | 93.67% |
| HINDU | 10 | 3.34% |
| SIKH | 9 | 3% |
| OCCUPATION | ||
| STUDENTS | 44 | 14.66% |
| BUSINESS | 94 | 31.33% |
| GOVT. EMPLOYEE | 66 | 22% |
| PRIVATE EMPLOYEE | 10 | 3.33% |
| UNEMPLOYED | 39 | 13% |
| DRIVER | 24 | 8% |
| LABOURER | 22 | 7.33% |
| OTHERS | 1 | 0.33% |
| FAMILY TYPE | ||
| NUCLEAR | 180 | 60% |
| E. NUCLEAR | 66 | 22% |
| JOINT | 54 | 18% |
| SOURCE OF REFFERAL | ||
| FAMILY/SELF | 179 | 59.67% |
| PHYSICIAN | 60 | 20% |
| PSYCHIATRIST | 29 | 9.67% |
| OTHERS | 32 | 10.67% |
| PREDOMINAT REASON FOR SEEKING THE TREATMENT | ||
| SOCIAL | 123 | 41% |
| COMORBIDITY | 93 | 31% |
| WITHDRAWAL | 59 | 19.67% |
| MEDICAL | 24 | 8% |
| LEGAL | 1 | 0.33% |
| SUBSTANCE USED | ||
| OPIODS | 73 | 24.34% |
| ALCOHOL | 45 | 15% |
| BEZODIAZEPINES | 24 | 8% |
| CANNABIS | 53 | 17.67% |
| INHALENTS | 6 | 2% |
| OTHERS | 2 | 0.66% |
| POLYSUBSTANCES | 97 | 32.34% |
| AGE(YEARS) OF ONSET/FIRST USE | ||
| UPTO 10 | 5 | 1.67% |
| 11-15 | 63 | 21% |
| 16-20 | 139 | 46.34% |
| -21-25 | 51 | 17% |
| 26-30 | 33 | 11% |
| ›31 | 9 | 3% |
| ROUTE OF ADMINISTRATION | ||
| ORAL | 172 | 57.91% |
| ORAL+SMOKING | 54 | 18.18% |
| SMOKING | 49 | 16.49% |
| OTHERS | 22 | 7.40% |
| PARENTRAL DRUGS USED | ||
| PENTAZOCINE | 11 | 39.28% |
| TRAMADOL | 9 | 32.14% |
| BENZODIAZEPINES | 7 | 25% |
| OTHERS | 1 | 3.57% |
| PREDOMINANT REASON FOR STARTING THE SUBSTANCE | ||
| PEER PRESSURE | 107 | 35.67% |
| EXCITEMENT/CURIOSITY | 71 | 23.67% |
| R.F.N.M.S. | 39 | 13% |
| PSYCHIATRIC COMRBIDITY | 69 | 23% |
| MEDICAL COMRBIDITY | 5 | 1.67% |
| E.P.M.S. | 6 | 2% |
| FAMILY HISTORY | 3 | 1% |
| TYPE OF THE PSYCHIATRIC COMORBIDITY | ||
| MDD | 42 | 32.06% |
| BPAD | 41 | 31.29% |
| ANXIETY & ADJUSTMENT DISORDER | 39 | 27.48% |
| SUBSTANCE INDUCED PSYCHOSIS | 7 | 5.34% |
| SCHIZOAFFECTIVE DISORDER | 2 | 1.52% |
In our study 98% (N=295) of the patients who attended the hospital for the treatment of substance use disorders were males (N=295). Females constituted only 1.67 %( N=5).About 60 % of the patients in our study were unmarried (N=181) and about 40 % of the patients were married (N=119).The majority number of patients (50.33%) in our study presented in the age range 21-30 years (N=151). About 10% presented in the age group greater than 40 years (N=29).The mean age at time of presentation was 28.99years.Maximum number (about 66%) of the patients in the study were the resident of urban and semi urban areas (N=199). Most of the patients in our studies were Muslims only few of the patients(6.34%) who attended Psychiatric Disease Hospital for the treatment belonged to the religion other than Islam (N=19). In our study about 31 %( N=94) were gainfully Engaged with some kind of business. About 25% (N=76) of the patients were doing some kind of job either government or private.14.66% (N=44) were students. In our study 60% (N=180) came from nuclear family. Only 18% (N=54) belonged to joint family. From the table it is clear that most of the patients [62% (N=216)] were belonging to the middle class family. Only 6% (N=18) came from either upper or lower class.
It can be inferred from the table that many patients 36% (N=108) had passed primary and only few 3% (N=9) were post graduates. Illiterate (N=61) formed 20.33% and 29.33% studied up to higher secondary. Most of the people 59.67% (N=179) in our study came to hospital were motivated for the treatment by the family and referred by one of the family member or sought treatment by themselves. Others which formed 10.67% (N=32) of the study were referred by friend, treated patient, media etc. The table shows that most common reason for seeking treatment for substance use disorder was social problems 41% (N=123). This was followed by comorbidity 31% (N=93) and withdrawal 19.67% (N=59).Most of the patients 84.34% (N=253) were dependent on substances. Only 15.63% (N=47) of the patients were only abusing the drugs. From the table it is clear that significant number of people 46.34% (N=139) in our study started using substance in the age group of 16 to 20 years. Only less number of 3% (N=9) started using substance beyond the age of 31 years. The mean age of onset of substance use was 19.66 years. A significant number of patients 32.34% (N=97) were using more than one substance. Opioid derivatives which constituted 24.34 %( N=73). Cannabis was used by 17.67 %( N=53) and alcohol was used by 15 %( N=45).Other included antihistaminic (Avil) etc.
Among the opiod derivatives the most common drug abused was codeine (cough preparations) and formed 64.38% (N=47). Spasmoproxyvon (each capsule containing propoxyphene 100mg+dicyclomine 50mg+acetoemenophen 400mg) abuse was also high 23.28% (N=17). Diacetyle morphine that is heroin was used by 6.84% (N=5).Among the polysubstance abusers or dependents [32% (N=97)].The most common combination was codeine and benzodiazepines (BZD) 34.02% (N=33). Three or more substances were used by 19.58% (N=19). This was followed by cannabis and alcohol 8.24% (N=8) and spasmoproxyvon and benzodiazepines 7.2 %( N=7). Common parental drugs used were pentazocine 39.28 %( N=11), tramadol 32.14 %( N=9), benzodiazepines 25 %( N=7). Others include antihistaminic. Most of the patients in the study were smokers 93.34 %( N=281) and only few of them were non- smokers 6.67 %( N=19). Most common route of administration used by the patients in our study was oral 57.91% (N=172) followed by oral and smoking (inhalational) 18.18 %( N=54) and smoking 16.49 %( N=49). Parental drug users were 9.34 %( N=28). Only 2.67 % (N=8) were sharing needles. Among the psychiatric comorbidity, patients with Major Depressive Disorder (MDD) were 32.06 %( N=42), Bipolar Affective Disorder (BPAD) were 31.29 %( N=41), anxiety and adjustment disorders were 27.48% (N=39). These three groups formed the bulk of patients with psychiatric comorbidity.
Out of the 300 patients only 13% (N=39) of the patients had previous history of hospitalization or treatment for substance abuse. Rest of the patients 87% (N=261) had come to the hospital first time. Family history for the psychiatric disorders was present in 12% (N=36) of the patients, family history of substance abuse of the same nature or other substance was present in 9.67% (N=29) and family history of some form of medical disorder especially hypertension and diabetes was present in 10% (N=10) of the patients.
Discussion
Prolonged and regular use of illicit substances is harmful to both individual and to the society. Drug use in any society varies considerably across socioeconomic groups, across time and regions, and reflects the cultural practices of different sections of the society [7]. Substance use disorders as reflected by the number of substance abuse patients attending the sole psychiatric disease hospital from the whole valley have shown a substantial increase [8]. Many developing countries have seen rapid increase in the use of opioids, cocaine and psychotropic drugs. In a number of these countries injectable drugs are becoming very common [9].
In our study most of the patient 85 % (N=253) were drug dependents at the time of presentation. Drug related withdrawal symptoms and other personal, family and social problems associated more with drug dependence than abuse, could be a reason for higher number of dependents in our study because of the increased treatment seeking in this group. Most of our patients [50.5 % (N=151)] presented in the age group of 21 to 30 years, followed by 24 %( N=72) in the age group of 31 to 40 years. These findings are consistent with Khantzian M D et al [10], who observed 49.6 % patients in the age group of 25-29 years and 17.3 % in 20-24 years age group. Our findings are also consistent with Drug Abuse Monitoring System (DAMS) where most of the people (70%) presented in the age group of 21-40 years. In our study 74% (N=223) of the people were in the age groups of 21-40 years. Age below 20 years at the time of presentation constituted 16 %( N=48) in our study which is consistent with Drug Abuse Monitoring System [7] for Jammu and Kashmir state (18.5%).
The reason for presentation by the young age group could be because of younger age of onset of substance use in our sample. Mean age of the patients in our study at the time of presentation was 28.99 years lesser compared to 35.3 years in Drug Abuse Monitoring System [11] and 33 years in the study by Thomas J Crawley et al. [12] Majority of the patients in our study were male i.e. 98.33% (N=295) and only 1.67% (N=5) were females (p=0.00). This finding is consistent with DAMS where most of the respondents 97.2% were males and 2.8% were males. [7] Most of the studies except Crawley., et al. [12] (who reported 56% females), have reported majority of males in their studies [10,13-15]. Most of the patients in our study were unmarried [60.34 %( N=181)] and 39.67% (119) were married (p=0.00). None of the patients in our study was divorcee or widower. Similar results were found in other studies [16-18]. But as per Drug Abuse Monitoring System [7], 71.9% were married and only 22.8% were unmarried, which is contrary to our study. Drug Abuse Monitoring System also reported only 1.2 % divorced.
The reason for more unmarried patients in our study could be due to more number of younger age group patients as compared to the current marriageable age. Maximum number 46% (n=138) and 20.34 % (n=61) belonged to urban and semi urban areas respectively. Only 30.64% (N=101) were residents of rural areas. These findings are similar to Drug Abuse Monitoring System where 48.3% of the people belonged to urban areas [7]. Margoob et al reported 57.14% of the patients were residents of urban areas [19]. The reason for higher urban presentation in our study may be because the sole psychiatric disease hospital is situated in the centre of capital city Srinagar catering higher proportion of patients from adjoining urban or semi urban areas and migration of people from rural to urban areas. 93.67 % (N=281) of the patients in our study were Muslims. Only 3.34% (N=10) were Hindu and 3% (N=9) were Sikhs. This can be explained by the fact that in Kashmir valley most of the population is constituted by Muslims. In our study, 60 % (N= 180) belonged to nuclear family, 22% (N= 66) to extended nuclear and 18% (N=54) to joint family.
This is consistent with Baljeet singh saluja et al who reported that 63.5% of his patients belonged to nuclear families [21]. 72% (N=216) the people in our study came from middle class families [upper middle class 43% N=129 and lower middle class 29% (N=89)] and 25% (N=75) of the patients came from lower class. Only 3% (N=9) belonged to upper class. Some of these findings were consistent with Kadri A M., et al. [21] where upper class was reported to 3.5% and lower class 5.4%. Upper lower class formed bulk of the study (47.3%) which is contrary to our study. In our study 36% (N=108) were primary pass followed by higher secondary educated 29.33% (N=88) and illiterate 20.33% (N=61). Only 3% (N=9) were post graduates. As per Drug Abuse Monitoring System, 42% of the people had completed higher secondary and above followed by 12% graduates and 15% illiterate [7]. In our study social support was good in 93% (N=279), and minimal in 7% (N=21) (p<0.05). Other study reported good social support in about 97.6% of the patient with substance abuse [21], which is consistent with our study. This can be explained by the fact that there is high social bonding in our society. Most of the times more than one person used to accompany the patient for consultation.
The attendants were always ready to act as caretakers of the patient and provide every kind of support including the emotional and the financial help. In our study 59.67% (N=179) were referred by the family or by themselves. 20% (N=60) were referred by the physicians in whom most of them were in withdrawal state or some medical complication. Similar results were reported by Sandeep Grover were most of the subjects (55%) were referred for the treatment by the family. 23.5% of the patients were referred from the other departments [22]. Baljeet., et al. [21] observed that 69.9% of the subjects were brought by relative and only 21.2% sought help on their own, rest of the people were referred by physicians. The reason for higher family referral in our study could be due to the concern for the patient and also may be the family’s awareness regarding the fact that drug abuse is a treatable disease and have serious consequences if not taken care at proper time.
In our study social factors and rejection 41% (N=123) formed main reason for seeking the treatment, followed by comorbidity 31% (N=93) and complications like withdrawal 19.67 % (N=59). Weisner et al reported that most of the people enter the treatment due to family pressure, employer pressure or health professional advice [23]. In our study most of the patients were having social problems like inability to fulfill the obligations of family, relatives and neighbors. All these factors could be the reason for seeking treatment. Most of the patients in our study 46.34% (N=139) started substance use in the age group of 16 – 20 followed by 21 % (N=63) in the age group 11 – 15 years and 17% (N=51) in the age group of 21 – 25 years. The mean age of starting substance use was 19.66 years. Similar results were found by Ho-wai so., et al. [24], who reported the mean age of first use as 19.2 years. Lamptey et al reported 56.3% of the patients started drug abuse in the age group of 15-19 years. This can be akin to our study [25]. Drug Abuse Monitoring System [7] reported mean age for first use for males 23 years and females 24 years which is slightly higher than our study. About 75% started using drug in the age group of 16 – 30 years in DAMS which is similar to our study were 74.34% of the people started drug use in the age group of 16 – 30 years. Kadri., et al. [21] reported 39.6% of the substance abusers who initiated the drug use in the age group of 16 – 20 years which is slightly lesser than in our study [46.34% (N=139)].
Polysubstance use formed the most common form of abuse in our study. 34% (N=97), followed opiods 24.24% (N=73), Cannabis 17.67% (N=53), Alcohol 15% (N=45). Among the polysubstance abusers (N=97), the most common pair combination was codeine and benzodiazepine 34.02% (N=33) and 19.58% (N=19) of the patients used to have three or more substances per day. This was followed by combination of cannabis and Alcohol 8.84% (N=8), Spasmoproxyvon 7.2% (N=7) and benzodiazepines. Among the opioid derivatives the most common drug abused was codeine (cough preparations) and formed 64.38% (N=47). Spasmoproxyvon abuse was also high 23.28% (N=17). Diacetyle morphine that is heroin was used by 6.84% (N=5) only. Baljeet., et al. [21] reported that the commonest substance used was opioid 76.2% and the commonest opioid used was heroin 36.5%.which is consistent with our study where predominant substance abused was opioids. Our findings are not consistent Drug Abuse Monitoring System were Alcohol (43.9%) was predominant substance used followed by cannabis (11.6%) and opioid derivatives including Heroin, codeine etc (26%).
Alcohol use is very less in Kashmir as compared to the rest of India [7] which can be explained due to the predominant Muslim majority population who consider alcohol use as a taboo and in opposition to religion. Other study reported 60.11% of the patients of Narcotic analgesics use followed by stimulants 2.5% and cough mixture 6.94%. Only 1.39% of the patients were using Alcohol [24]. One of the main reasons of predominant opioid use in our set up can be explained by the fact that most of the treatment seekers attributed its use due to easily availability of the substance and were able to get the drug directly from the stockiest without prescribing by some doctor. One of the reasons given by opioid against alcohol use was that opioid preparations were not associated with smell and could be safely used at home without seeking family attention. 93.34% (N=281) were using or abusing Nicotine in the form of cigarettes, Huka, chewing, only 6.67% were nonsmokers or not using nicotine in any form in our study. Other study [26] reported the prevalence of smoking in community is very high (24.5%).
In addition to this 10.63% of the population abuse tobacco in other form like chilam, beedi, harg rolled cigar etc. A small percentage of the population abused tobacco in smokeless form like snuff 2.5%, zarda (0.47%) and pan Masala (1.63%). The tobacco can serve as a gateway drug to use and dependence of harder substance like heroin and other opioids preparations as was in our study. Majority of the patients 95% (N=190) were using substances daily. Only few i.e. 5% (N=10) used to have the drug only 2 – 4 times per week. Ho-Wai So et al reported that 90.77% of the people used drug every day and 4.62% of the patients were taking drug few times per week. These findings are consistent with our study [24]. The daily use of substances in our study could be due to the nature of the drugs used as most of them produce withdrawal symptoms in a short duration on stopping and as most of the patients in our study were dependents and therefore needed the substance every day to prevent the withdrawal symptoms which as described by the respondents were quite distressing and intolerable.
Most common route used was oral 57.91 % (N=172) followed by (oral + smoking / inhalation) 18.18% (N=54). Most of the patients in our study used codeine (liquid), benzodiazepine tablets, spasmoproxyvon capsules, alcohol and cannabis by smoking. About 9.67% (N=29) patients in our study used parenteral route for drug administration which included intravenous and intramuscular. 3 % (N=9) gave history of sharing of needles. Drug Abuse Monitoring System reported 14% of the sample using injectable drugs and only 9% used it in the last month. While as 4% of the patients reported sharing of needles in the last month [7]. In our study most common form of substance used was solid 37% (N=111) followed by liquid 30% (N=90) and solid and liquid combination 28% (N=84). Most common substances used were cannabis, tablets, capsules, alcohol, and liquid cough preparations.
In our study the predominant reasons for starting the substance was peer pressure 35.67%, excitement or out of curiosity 23.67% and psychiatric comorbidity 23%. Margoob et al (2004) reported that peer pressure was most common reason for starting the substance 44.44%, followed by curiosity 16.66%, which is consistent with our study. In contrast to our study, Doctor., et al. [27] reported that predominant reasons for starting the substance was family influence 41.8% followed peer pressure 27.87%. In our study only 9.67% of the people gave family history of drug abuse. Ho-Wai., et al. [24] reported that curiosity was the main reason for starting substance, followed by relief from negative mood state (20-29%), sensational excitement 17.39% and peer pressure 7.39%. As most of the patients in our study are of younger age group at which peer influence is more predominant than that of the family, so it could be a reason that most of the patients have started substance use under peer pressure.
Most of the patients 43.34% (N=130) in our study were using drugs for one to five years followed by 27.34% (82) for period of 6 – 10 years. Mean duration of substance abuse was 8.88 years. in a study [7] 53.5% of the people used drugs for the period of 5 – 10 years and 36.5% of the patients used the drug for duration of 1 – 5 years which is in contrast with our study. Wheeler at al reported 57% of the patient used the drug for more than 2 years [28]. Margoob.,et al. [19] reported 41.65% patients took substances for period of more than 5 years and only 5.94% took medication for less than 1 year. Most of the patients in our study [54% (N=162)] used the drug within 12 hours of seeking treatment. 28% of the patients presented to the hospital who have taken substance more than 2 days before see*king treatment and most of them presented in withdrawal. In our study 12 % (N=36) and 9.67 % (N=29) had family history of psychiatric disorder and substance abuse respectively. Drug Abuse Monitoring System reported family history of drug abuse in 48% of respondents which is contrary to our study [7].
Summary and Conclusion
- Most of the treatment seekers who attended the hospital for the substance use disorders were males in adult age group and most of them started using substance in adolescence.
- Bulk of the treatment seekers in our study was formed by businessmen, employees, students; most of which belonging to the nuclear family. Maximum were having good social support and referred by the family.
- Predominant substances used were opioids derivatives, cannabis, benzodiazepines and alcohol with significant number of polysubstance abusers using mostly opioid and benzodiazepine combination. So opioid derivative use is showing increasing trend in the treatment seekers in the valley.
- About forty three percent of the substance use disorders were having comorbid psychiatric disorder and more than one third having suicidal ideation although suicidal attempts were very less.
- Many of the patients were having high risk behavior, 9.34% percent were the parental drug users and 2.67% shared the needles and 19% of the patients had multiple sexual partners, 6.67% had sex with commercial sex worker. Both of these high risk behaviors form the fertile ground for the spread of deadly disease AIDS and other life threatening diseases.
References
- Arturo Qrtiz. “Development of a system for registry of information of drug use in Mexico”. Bulletin of Pan America Health Organization 24. 1 (1990): 46-52.
- Medino Mora ME., et al. “Epidemiological status of drug abuse in Mexico". Bulletin of Pan America Health Organization 24. 1 (1990): 1-11.
- Margoob MA and Dutta KS. “Drug abuse in Kashmir –experience from a psychiatric disease hospital”. Indian journal of Psychiatry 35. 3 (1993): 163-165.
- World Health Organization (WHO). Guide to drug abuse epidemiology. Geneva, Switzerland: Department of Mental Health and Substance Dependence, WHO; 2000.
- American Psychiatric Association: Practice guideline for the treatment of with substance use disorders-Alcohol, cocaine, opioids. Am J Psychiatry 152 (1995): 5-59.
- Booth BM., et al. “Social support and outcome of alcoholism treatment: An Exploratory Analysis”. American Journal of Drug Alcohol Abuse 18. 1 (1992): 87-101.
- Ray R, Mondal AB, Gupta K, et al, The extent, pattern and trends of drug abuse in India: National Survey. New Delhi. United Nations Office on Drugs and crimes and Ministry of Social Justice and Empowerment, Government of India.
- Margoob MA, Beg AA, Zaffar A. An evaluation of the recovery following treatment in drug abuse in only psychiatric disease hospital of Kashmir valley. Richmond fellowship Asia specific forum. International symposium Bangalore.23rd- 25th Nov. 1995).
- WHO Fact sheet no.127.
- khantzian M D and Treece PhD. “DSM III psychiatric diagnosis of narcotic addicts”. Archive of general psychiatry 42. 11 (1985): 1067-1071.
- Bendtsen P., et al. “Social consequences of alcohol dependence”. Addict Behav 27. 1 (2002): 21-33.
- Thomus J Crawley., et al. “Drug and alcohol abuse among psychiatric admissions”. Archive of general psychiatry Jan 30. 1 (1974): 13-20.
- Helen E Ross., et al. “The prevalence of psychiatric disorders in patients with alcohol and other drug problems”. Archive of general psychiatry 45. 11 (1988): 1023-1031.
- kishore P., et al. “a study of comorbidity in psychoactive dependence patients”. Indian Journal of Psychiatry, 36. 3 (1994): 133-137.
- Brooner K., et al. “antisocial behavior of intravenous drug abusers; implication for diagnosis of antisocial personality disorders”. American Journal of Psychiatry 149. 4 (1992): 482-487.
- Wheeler K., et al. “a profile of drug takers”. Medical Journal of Australia 2 (1969): 291-294.
- Najavitis M., et al. “cocaine dependence with or without PTSD among subjects in the national Institute of drug abuse; collaborative cocaine treatment study”. American journal of psychiatry 155. 2 (1998): 214-219.
- Hellikas A., et al. “Marijuana use and psychiatric illness”. Archive of general psychiatry 27 (1972): 162-164.
- Mushtaq ahmed margoob et al, use of TLC as broad spectrum screen for detection of drugs of abuse, JK practioner, 11. 4 (2004): 257-260.
- Saluja Baljeet Singh., et al. Drug dependence in adolescents 1978-2003: A clinical- based observation from North India. Indian Journal of Pediatrics 74. 5 (2007): 455-458.
- A.M. Kadri, A. Bhagyalaxmi, Geeta Kedia,socio-demographic characteristics of the substance abusers Indian Journal of Community Medicine Vol. XXVIII, No.2, Apr.-June, (2003).
- Sandeep Grover., et al. “Drug dependence in geriatric age group: a clinical based study”. German Journal of Psychiatry 11 (2008): 10-15.
- Weisner C., et al. Factors affecting the initiation of substance abuse treatment in managed care at Chemical Dependency program of a large group model health maintenance organization (HMO). Addiction.96. 5 (2001): 705-16.
- Ho-wai so., et al. substance abuse and psychiatric comorbidity: millon clinical multiaxial inventory-III profile of Chinese substance abusers. Hono kong Journal of Psychiatry 15; 3 (2005): 89-96.
- Lamptey J., et al. Socio-demographic characteristics of abusers and compares some of the characteristics to randomly selected non-substance abusers. Ghana Med J. 39. 1 (2005): 2-7.
- Margoob MA, Beg AA, Zaffar A. An evaluation of the recovery following treatment in drug abuse in only psychiatric disease hospital of Kashmir valley. Richmond fellowship Asia specific forum. International symposium Bangalore.23rd- 25th Nov. 1995.
- Doctor P P cross sectional epidemiological study of substance users in urban area field practice area in Mumbai, India; Calicut Medical Journal 2. 11 (2004): e8.
- Wheeler k, Edmonds e: A profile of drug takers. Medical journal of Australia 2 (1969): 291-294.
Citation:
Ajaz Ahmad Suhaff., et al. “Socio-demographic & Clinical Profile of Patients with Substance Use Disorders Seeking Treatment. A Hospital Based Study”.
Chronicles of Pharmaceutical Science 3.2 (2019): 828-838.
Copyright: © 2019 Ajaz Ahmad Suhaff., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.