Research Article
Volume 1 Issue 1 - 2018
Correlation Between Hyperprolactinemia and Magnetic Resonance image of Pituitary. A Retrospective Single Centre Study in Saudi Community Based Hospital.
Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia. PO Box 9862. Jeddah 21159. Kingdom of Saudi Arabia
*Corresponding Author: Khalid S Aljabri, MD, FRCPC, FRCPC (Endo), FACP, ABIM, ABEM. Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia. PO Box 9862. Jeddah 21159. Kingdom of Saudi Arabia.
Received: March 10, 2018; Published: March 28, 2018
Abstract
Background: Data on hyperprolactinemiaprevalence in Saudi Arabia are very scarce.
Objective: To estimate the correlation between hyperprolactinemia and magnetic resonance image of pituitary in a well-defined population.
Design: Retrospective analysis of radiological and hormonal data of patients with pituitary magnetic resonance image (MRI) between January 2008 and December 2017.
Settings: Departments of Endocrinology and Radiology at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia.
Patients: 516 patients with clinical, hormonal and radiological data.
Main outcome measures: Correlation between hyperprolactinemia and magnetic resonance image of pituitary.
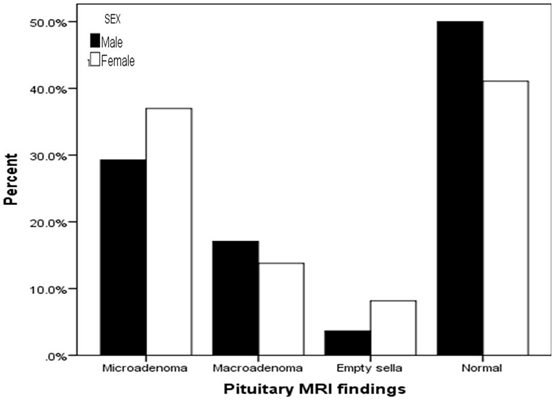
Results: Over the 9-year period, out of 516 patients; 401 (78%) subjects, 152 (30%) males and 364 (70%) females, were diagnosed to have hyperprolactinemia with mean age 36.3 ± 14.5. Out of hyperprolactinemia subjects, prolactinoma was present in 200 (39%) of cases whereas microadenoma and macroadenoma were seen in 142 (28%) and 58 (11%) subjects respectively. Microadenomas were not significantly more seen in females, 118 (37%) vs. 44 (14%) where as macroadenomas were not significantly more seen in males 24 (29%) vs. 14 (17%), p = 0.2. Subjects with macroadenoma have significantly higher serum prolactin than subjects with microadenoma 3715 ± 10283 vs. 1818 ± 2085 respectively, p = 0.02. 172 (33%) subjects have normal pituitary MRI. Most of the subjects presented in third and fourth decades of life. Advanced age was significantly associated with larger PA size, r = 0.4, p < 0.0001.
Conclusion:This is the first study reporting the epidemiology of hyperprolactinemia in Saudi Arabia. It showed that PA was more than previously reported. This increased prevalence may have important implications when prioritizing funding for research and treatment of PA.
Limitations: Question of clustering of cases within the study region and limited study sample size.
Keywords: Hyperprolactinemia; MRI pituitary; Saudi Arabia
Introduction
Hyperprolactinemia is the most common endocrine disorder of the hypothalamic-pituitary axis. It is estimated to occur in 9%-17% of women with reproductive disorders [1,2]. The differential diagnosis of hyperprolactinemia includes hypothalamic/pituitary tumors, of which the prolactinoma is the most common [3]. Prolactinomas comprise 40% to 57% of all pituitary adenoma. MRI imaging is the procedure of choice in the evaluation of sellar masses [4]. The diagnostic approach to a suspected Pituitary adenomas (PA) depends on the presenting symptoms and abnormal hormone values. There is no evidence from controlled trials to guide a specific investigative approach, and recommendations are based largely on expert opinion and extrapolation from observational studies [5-10].
PA are a diverse group of tumors arising from the pituitary gland. Historically, PA have been classified according to size and If the tumor is 10 mm or larger, it is considered a macroadenoma; if it is less than 10 mm, it is considered a microadenoma. Microadenomas are slightly more common than macroadenomas [57.4% vs. 42.6%] [11]. The uncertainty regarding the true correlation between hyperprolactinemia and magnetic resonance image of pituitary led us to undertake an intensive, retrospective epidemiological study in a tightly defined geographical area in Jeddah, Saudi Arabia.
Methods
All MRI pituitary records were collected from the radiology department data base between January 2008 and December 2017 at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia. MRI and clinical Records of patients were thoroughly analyzed. Out of the initial screening of 630 subjects, 114 subjects were excluded from the study as they were either incomplete clinical records or MRI was repeated for the same patients. Patients with abnormal thyroid function tests, renal failure or pregnancy were excluded. The remaining 516 subjects constitute the subject material for the study. Information was collected from two resources such as clinical case records of subjects of hyperprolactinemia seen at the endocrinology or other services. Serum prolactin < 324 mU/l was considered to be normal for our laboratory reference. PA were divided according to their size on MRI scan into microadenoma (less than 10 mm in diameter) and macroadenoma (more than or equal to 10 mm in diameter).
Statistical Analysis
Continuous variables were described using means and Standard Deviations. Univariate analysis of baseline demography both between groups, were accomplished using unpaired t-test and Chi square test were used for categorical data comparison. Pearson correlation was used for correlation. P value < 0.05 indicates significance. The statistical analysis was conducted with SPSS version 22.0 for Windows.
Continuous variables were described using means and Standard Deviations. Univariate analysis of baseline demography both between groups, were accomplished using unpaired t-test and Chi square test were used for categorical data comparison. Pearson correlation was used for correlation. P value < 0.05 indicates significance. The statistical analysis was conducted with SPSS version 22.0 for Windows.
Results
Over the 9-year period, out of 516 patients; 401 (78%) subjects, 152 (30%) males and 364 (70%) females, were diagnosed to have hyperprolactinemia with mean age 36.3 ± 14.5 (table 1). Out of hyperprolactinemia subjects, prolactinoma was present in 200 (39%) of cases whereas microadenoma and macroadenoma were seen in 142 (28%) and 58 (11%) subjects respectively, (table 2). Microadenomas were not significantly more seen in females, 118 (37%) vs. 44 (14%) where as macroadenomas were not significantly more seen in males 24 (29%) vs. 14 (17%), p = 0.2, figure. Subjects with macroadenoma have significantly higher serum prolactin than subjects with microadenoma 3715 ± 10283 vs. 1818 ± 2085 respectively, p = 0.02. 172 (33%) subjects have normal pituitary MRI. Most of the subjects presented in third and fourth decades of life. Advanced age was significantly associated with larger PA size, r = 0.4, p < 0.0001.
| Parameters | Total | Hyperprolactinemia | P value | ||
| Present | Absence | ||||
| Numbers | 516 | 401 (78) | 115 (22) | ||
| Age | 36.3 ± 14.5 | 35.4 ± 12.6 | 39.4 ± 19.3 | 0.008 | |
| Gender | Male | 152 (30) | 82 (54) | 70 (46) | < 0.0001 |
| Female | 364 (70) | 319 (88) | 45 (12) | ||
Data are number (%) and mean ± standard deviation
Table 1: Demographic data.
Table 1: Demographic data.
| Parameters | Total | Hyperprolactinemia | P value | |||
| Present | Absence | |||||
| Tumor diameter (mm) | 9.7 ± 8.9 | 8.6± 7.1 | 15.4 ± 14.0 | 0.009 | ||
| MRI findings | Total pituitary adenoma | 245 | 200 (82) | 45 (18) | ||
| Pituitary macroadenoma | 76 (15) | 58 (11) | 18 (3) | 0.006 | ||
| Pituitary microadenoma | 169 (33) | 142 (28) | 27 (5) | |||
| Empty sella | 48 (9) | 29 (6) | 19 (4) | |||
| Normal | 223 (43) | 172 (33) | 51 (10) | |||
Data are number (%) and mean ± standard deviation
Table 2: Subtypes of pituitary adenomas.
Table 2: Subtypes of pituitary adenomas.
Discussion
This study demonstrated excellent correlation between radiologic abnormalities and in prolactin secreting PA. Although the majority of patients with prolactin secreting PA have been women, endocrinologic evaluation of men has been prompted by symptoms of impotence, gynecomastia, and, in some cases, galactorrhea. The seemingly low incidence of these tumors in men may well increase as this possibility is more frequently considered in evaluation of male sexual dysfunction.
PA are the most common cause of hyperprolactinemia, which results from either direct production by the adenoma (prolactinoma) or the stalk effect. Prolactinomas are the most common PA and are classified into two types based on size: microadenomas (less than 10 mm) and macroadenomas (10 mm or greater) (12). As shown in our report, Circulating prolactin levels usually parallel tumor size, such that microadenomas rarely result in prolactin levels higher than 4255 mIU/L and macroadenomas usually result in prolactin levels higher than 4255 mIU/L (13).
In this sample, the mean ages were 36 years old. Females were younger than males in keeping with previous data from surgical series and immunohistochemical studies of autopsy data. We showed that 71% of prolactinoma were microadenomas which are higher than previously reported (57%), in contrast, 29% of prolactinoma were macroadenoma which are lower than previously reported (43%) [11]. Hyperprolactinemia were more prevalent in female (88% vs. 54%). It should be taken into account that prolactinoma mostly affect young and economically active individuals in whom diagnostic delay translates into loss of productivity. These data highlight the need for increasing the awareness of these treatable conditions, thereby minimizing the adverse sequelae of late diagnosis. The higher prevalence of prolactinoma is probably attributed not only to the advances and the easier access to diagnostic tools (imaging and hormonal assays), but also, and most importantly, to the increased awareness and suspicion rate of these more, underdiagnosis of this condition cannot be excluded, in addition, is likely because most of our patients were referred to endocrinology service for evaluation of hyperprolactinemia and our department protocol to obtain MRI pituitary for all cases of high serum prolactin if persisted on two samples.
Hyperprolactinemia were identified in a population of 300,000 individuals eligible for the care of King Fahad Armed Forces hospital in Jeddah; it translates to mean prevalence of 134 cases per 100,000 population. 200 patients with clinically relevant PA were identified translates to mean prevalence of 67 cases per 100,000 population that are within the reported literature [14,15]. Furthermore, data extracted from tertiary referral centres are influenced by selection bias and by the wide variations in referral patterns.
MRI imaging is the procedure of choice in the evaluation of sellar masses [23]. The diagnostic approach to a suspected PA depends on the presenting symptoms and abnormal hormone values. There is no evidence from controlled trials to guide a specific investigative approach, and recommendations are based largely on expert opinion and extrapolation from observational studies [9,10]. A patient who presents with symptoms of hormone excess likely has a functioning adenoma. Evaluation can be geared toward the specific hypersecretory syndrome.
We found a partially empty sella in 6% of patients, which is a much lower incidence than that reported [16]. In conclusion, the current study is the first report indicates high frequency of hyperprolactinemia and prolactinoma. In the absence of registry data, larger cooperative studies involving diverse population samples from multiple centers could help to provide further information on the true epidemiology of hyperprolactinemia nationally.
Acknowledgement
The author would like to thank all colleagues from the Department of Endocrinology for helping in data collection.
The author would like to thank all colleagues from the Department of Endocrinology for helping in data collection.
Conflict of interests
The authors declare no conflict of interests.
The authors declare no conflict of interests.
References
- Miyai K., et al. “Asymptomatic hyperprolactinaemia and prolactinoma in the general population: mass screening by paired assays of serum prolactin”. Clinical Endocrinology 25.5 (1986): 549 –54.
- Biller BM., et al. “Guidelines for the diagnosis and treatment of hyperprolactinemia.” The Journal of Reproductive Medicine 44.12 (1999): 1075-1084.
- Mah PM and Webster MA. “Hyperprolactinemia: etiology, diagnosis, and management”. Seminars in Reproductive Medicine 20.4 (2002): 365–73.
- Seidenwurm DJ. “Neuroendocrine imaging”. International Journal of Endocrine Oncology 2.2 (2008): 613-615
- Vance ML., et al. “Diagnosis and Management of Pituitary Tumors”. The Humana Press Inc in Totowa (2001): 165-172.
- Freda PU., et al. Endocrine Society. Pituitary incidentaloma: an Endocrine Society clinical practice guideline. The Journal of Clinical Endocrinology & Metabolism 96.4 (2011): 894-904.
- Nieman LK., et al. “The diagnosis of Cushing’s syndrome: an Endocrine Society clinical practice guideline”. The Journal of Clinical Endocrinology & Metabolism 93.5 (2008): 1526-1540.
- Fainstein Day P., et al. “Retrospective multicentric study of pituitary incidentalomas”. Pituitary 7.3 (2004): 145-148.
- Vilar L., et al. “Diagnosis and management of hyperprolactinemia: results of a Brazilian multicenter study with 1234 patients”. Journal of Endocrinological Investigation 31.5 (2008): 436-444
- Melmed S., et al. “Endocrine Society. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline”. The Journal of Clinical Endocrinology & Metabolism 96.2 (2011): 273-288.
- Daly AF., et al. “High prevalence of pituitary adenomas: a cross-sectional study in the province of Liege, Belgium”. The Journal of Clinical Endocrinology & Metabolism 91.12 (2006): 4769-4775.
- Klibanski A. Clinical practice. Prolactinomas. The New England Journal of Medicine 362.13 (2010):1219-1226.
- Wenyu Huang and Mark E Molitch. “Evaluation and management of galactorrhea”. American Family Physician Journal85.11 (2012): 1073-1080.
- Davis JR., et al. “Pituitary tumours”. Seminars in Reproductive Medicine 121.5 (2001): 363–371
- Fernandez A., et al. “Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK)”. Clinical Endocrinology 72.3 (2010): 377-382.
- Richmond IL., et al. “Prolactin-secreting pituitary adenomas: correlation of radiographic and surgical findings”.American Journal of Roentgenology 134.4 (1980): 707-710.
Citation:
Khalid S Aljabri., et al. “Correlation Between Hyperprolactinemia and Magnetic Resonance image of Pituitary. A Retrospective
Single Centre Study in Saudi Community Based Hospital.” Archives of Endocrinology and Diabetes Care 1.1 (2018): 13-17.
Copyright: © 2018 Khalid S Aljabri., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.