Case Report
Volume 1 Issue 2 - 2018
A Case of an Ectopic Papillary Thyroid Carcinoma Located in the Midline of the Neck. A Case Report and Review of the Literature.
1Department of Endocrinology
2Department of Pathology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia
3Department of Ear, Nose and throat
4College of medicine, Um Al Qura University
2Department of Pathology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia
3Department of Ear, Nose and throat
4College of medicine, Um Al Qura University
*Corresponding Author: Khalid S Aljabri, Department of Endocrinology, King Fahad Armed Forces Hospital, Jeddah, Kingdom of Saudi Arabia, PO Box 9862. Jeddah 21159. Kingdom of Saudi Arabia.
Received: April 04, 2018; Published: April 26, 2018
Abstract
Ectopic thyroid tissue develops through the abnormal migration of thyroid tissue at the embryologic period. Malignant transformation has been reported in thyroglossal duct, pyramidal lobe and as well as in other ectopic thyroid. We report the incidental finding of a papillary thyroid carcinoma located in the midline of the neck in a 28-year old woman.
Keywords: Ectopic thyroid; Papillary thyroid carcinome
Introduction
Thyroid gland is located in front of the trachea between C5-T1 vertebrae. It’s derived from the foramen cecum at the back of the tongue and descends down [1]. Ectopic thyroid tissue develops through the abnormal migration of thyroid tissue at the embryologic period [2-4]. Thyroglossal duct remains open for a short time and then degenerate. Ectopic thyroid generally resides anywhere along its embryologic pathway of descent. It may be found at the base of the tongue as well as the supra- and sub hyoid bone. It is frequently found around the course of the thyroglossal duct (midline of neck) or laterally in the neck, as well as in distant places such as the mediastinum and the sub diaphragmatic organs [5-8]. It is often misdiagnosed as thyroglossal duct cysts [2-4]. Its prevalence is about 1 per 100 000-300 000 people, rising to 1 per 4000-8000 patients with thyroid disease [9-10]. However, in autopsy studies, the prevalence ranges from 7 to 10% [11-12]. More than 440 cases have been reported to date. In 70-90% of cases, it is the only thyroid tissue present [9-13]. Ectopic thyroid is most common in females, especially in populations of Asian origin [13-14]. It may occur at any age, from 5 months to 40 years, but it is most common at younger ages. Malignant transformation has been reported in thyroglossal duct, pyramidal lobe and as well as in other ectopic thyroid [4-15]. In the malignant transformation of an ectopic thyroid is not common, and in such cases, it is generally a papillary carcinoma, but this transformation of an ectopic thyroid without a presenting tumor in the thyroid gland is extremely rare [16-17]. We report the incidental finding of a papillary thyroid carcinoma located in the midline of the neck in a 28-year old woman.
Case Report
28-year old Saudi woman presented with a growing painless soft swelling mass located in the anterior midline of her neck. She noted the neck mass since childhood. The patient neither had any pre-existing diseases, nor a history of radiation exposure. Physical examination including lymph node palpation as well as x-ray of the chest were unsuspicious. Laboratory examination confirmed a euthyroid metabolic state without thyroid-specific medication. May 2017, Neck contrast computed tomography revealed a evidence of a well-defined lobulated outline hypo dense enhancing lesion, seen involving the infra hyoid soft tissue aspects of the anterior right para midline strap muscles of the lower neck, measuring 2 x 2.8 x 1.8 cm at its maximum dimensions with surrounding enhancing blood vessels with questionable small linear similar density in continuation to the thyroid isthmus (Figure 1). Six months later, Sistrunk procedure was performed. The histopathological examination of the resected tissue reveal thyroid parenchyma with papillary thyroid carcinoma. The neoplasm is formed of thyroid follicles and papillae lined by optically clear nuclei with nuclear grooves and occasional pseudo nuclear inclusions. Lymphovascular invasion is present. The tumour is inflitrative and reaches the inked margin. There is no evidence of thyroglossal cyst (Figure 2). After the diagnosis of ectopic thyroid with papillary thyroid carcinoma, a Tc - 99m thyroid scan showed no evidence of rounded photogenic nodule. After detailed discussion of the case, total thyroidectomy was performed. The histopathological examination of the resected thyroid tissue showed Focal lymphocytic thyroiditis with no evidence of papillary thyroid carcinoma. The patient was put on thyroid replacement therapy and remains well 2 months later. Subsequently, radioiodine ablation was recommended.
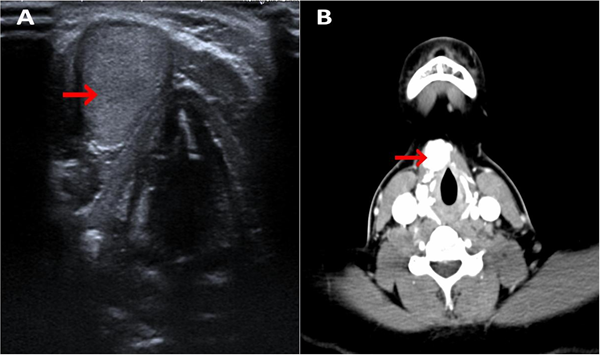
Figure 1: A. Neck ultrasound showed a 2.8 cm solid with thin and smooth outlines (Red arrow).
B: Neck contrast computed tomography showed an evidence of a well-defined enhanced lobulated outline hypo dense enhancing lesion, seen involving the infra hyoid soft tissue aspects of the anterior right para midline strap muscles of the lower neck, measuring 2 x 2.8 x 1.8 cm at its maximum dimensions with surrounding enhancing blood vessels ( Red arrow).
B: Neck contrast computed tomography showed an evidence of a well-defined enhanced lobulated outline hypo dense enhancing lesion, seen involving the infra hyoid soft tissue aspects of the anterior right para midline strap muscles of the lower neck, measuring 2 x 2.8 x 1.8 cm at its maximum dimensions with surrounding enhancing blood vessels ( Red arrow).

Figure 2: A. The nodule is composed of thyroid tissue exhibiting papillary thyroid carcinoma. There is no
identifiable cyst lining in the form of pseudo stratified columnar, squamous or cuboidal epithelium to suggest
a possible residual thyroglossal cyst (Arrow) [hematoxylin & eosin (H&E), 20X].
B. Well-formed papillae with fibro vascular core A lined by neoplastic follic ular cells of papillary thyroid carcinoma (H&E, 100X).
C. Papillary thyroid carcinoma exhibiting nuclear grooves and internuclear pseudo inclusion (H&E, 400X).
D. Lymphovascular invasion (H&E, 100X).
B. Well-formed papillae with fibro vascular core A lined by neoplastic follic ular cells of papillary thyroid carcinoma (H&E, 100X).
C. Papillary thyroid carcinoma exhibiting nuclear grooves and internuclear pseudo inclusion (H&E, 400X).
D. Lymphovascular invasion (H&E, 100X).
Discussion
Ectopic thyroid tissue in the midline of the neck, often occurs as a result of various defects during organogenesis or a result of post-surgical seeding. It was reported that this tissue becomes hypertrophic under the influence of increased thyrotrophin in thyroidectomized patients [18]. Ectopic thyroid tissue is rarely seen and often determined incidentally in asymptomatic patients [19]. The prevalence of ETT is about 1 per 100,000 - 300,000 people, and 1 in 4,000 to 8,000 patients with the thyroid diseases and being most common in females with male to female ratio is 1:4 [9-10, 20]. However, in autopsy studies, the prevalence was found 7-10% [11-12]. Ectopic thyroid tissue is most common in older than 40 years, especially in populations of Asian origin [13-14]. Anterior midline thyroid ectopia is most commonly derived from thyroglossal duct remnants, which are thyroglossal duct cyst and lingual thyroid, as well as pyramidal lobe [21]. Ninety percent of the reported cases of ectopic thyroid are found in the base of the tongue, while only 10% lie in the anterior aspect of the neck superficial to the hyoid bone. Being usually asymptomatic [22]. On histological examination, ectopic thyroid may be found within the wall of the cyst with an overall frequency of 5%. It produces thyroid hormones, but the concentrations are usually subnormal and patients may be hypothyroid [22-23].
Differential diagnosis of ETT in the midline of the neck is not always very easy. Probably, most of our cases may be thyroglossal duct remnant or pyramidal lobe. Approximately 1-3% of all ectopic thyroid tissue is located in the lateral neck [24]. However, incidence may be underestimated, since ectopic tissue is often found incidentally [25]. Primary malignant transformation of ectopic thyroid tissue is an exceedingly uncommon event; only 43 cases have been reported in the literature. From these cases, ten were identified as papillary thyroid carcinomas [26]. Carcinoma arising from ectopic thyroid tissue is comprising less than 1% of all thyroid carcinoma cases [20]. Papillary thyroid carcinoma is the most frequently identified subtype of carcinoma arising from ectopic tissue [25]. However, follicular, mixed follicular, and papillary Hurthle cell and medullary carcinomas have also been described [27]. Thyroglossal remnant carcinomas have been reported about 0.7-1.5% [28]. In 30%-70% of reported cases, the ectopic tissues were functionally hypothyroid or hashimoto’s thyroiditis [29].
Precise epidemiological data regarding the incidence and prevalence of lateral neck ectopic thyroid carcinomas are lacking, mainly due to the difficulty in distinguishing between metastatic diseases related to a thyroid primary carcinoma and true primary malignancy of the ectopic tissue [30]. Therefore, pathological analysis of tissue samples is paramount to accurately identify primary malignancies of ectopic thyroid tissue, once the clinical suspicion is established [30]. Our case presents an uncommon presentation by the fact that primary thyroid malignant lesion was located at the lateral ectopic tissue without evidence of active disease in the thyroid gland.
Clinical presentation of thyroglossal remnant carcinomas is very similar to benign masses and cannot be differentiated in terms of size, localization and appearance. Therefore, in many cases, the diagnosis of malignancy cannot be put until the operation [19]. However, if remnant is hard, fixed, or irregular or associated with pathologic lymphadenopathy, carcinoma should be suspected [31]. Additionally, increased risk of occult malignancy was reported in ETT especially when they include solid lesions [19]. In many studies, the diagnosis of malignancy was performed incidentally with histopathological evaluation after surgery [19]. Thus, the use of FNAB with ultrasound guidance may enhance the preoperative diagnosis. Carcinoma arising from the thyroglossal duct remnants constitutes a very uncommon histopathological entity [32]. CT and MRI are valuable tools in identifying the site of ectopy, especially when it is distant from the descending pathway of thyroid. Regarding CT imaging, thyroid tissue displays higher density on plain CT than the surrounding soft tissues, although enhanced images identify thyroid tissue more clearly than plain ones [33]. In MRI, ectopic thyroid appears as a rounded mass with higher signal intensity than that of the surrounding tissue in both the T1- and T2-weighed images [34]. CT and MRI are also useful modalities in cases when radioiodine uptake by normal thyroid gland masks the uptake of the ectopic thyroid tissue, especially in the midline [35].
There is no consensus about the optimal therapeutic strategy, perhaps due to the rarity of this clinical entity. Most authors agree that surgical treatment of ectopic thyroid in the neck (mainly lingual, sublingual, submandibular, and lateral cervical) depends on size and local symptoms (airway obstruction, dysphagia, and dysphonia), as well as on other parameters, such as patient’s age, functional thyroid status, and complications of the mass (ulceration, bleeding, cystic degeneration, or malignancy) [12,33, 36-39]. Some recommend complete surgical resection, considering the potential of malignant transformation [27]. For cases completely asymptomatic and euthyroid, regular follow-up is recommended in order to detect mass enlargement or development of complications [12,36-38,40]. For mild symptoms and hypothyroid states, levothyroxine replacement therapy may be effective, leading to considerable mass reduction [12, 36-38, 41]. With very few cases reported, it is difficult to assess the value of non-surgical management. Nonetheless, in cases when a surgical approach cannot be applied, suppressive hormone therapy with levothyroxine in order to avoid ectopic thyroid tissue growth and I-131 therapy for decreasing tumor’s size can be proposed [33,42].
In conclusion, developmental defects occurring at an early stage of embryogenesis generate ectopic thyroid tissue, residing anywhere along the gland’s embryological descending pathway. The majority of cases are asymptomatic, but symptoms related to tumor size and location may develop, as well as primary thyroid malignancy. The clinician should always take into account the potential of this rare entity and differentiate it from other masses in the neck.
Competing interests
The authors declare that they have no competing interests.
The authors declare that they have no competing interests.
References
- De Felice M and Di Lauro R. “Thyroid development and its disorders: genetics and molecular mechanisms”. Endocrine Reviews 25.5 (2004): 722-746.
- Ling L., et al. “Misdiagnosed ectopic thyroid carcinoma: report of two cases”. Chinese Medical Journal 117.10 (2004): 1588-1589.
- Gürer S., et al. “A rare thyroid carcinoma in ectopic thyroid tissue”. Journal of Islamic Academy of Sciences 4.2 (1991): 139-140.
- Lee HY., et al. “Thyroid papillary carcinoma in subhyoid ectopic thyroid tissue”. New Zealand Medical Journal 200.1 (2004): 17-18.
- Batsakis JG., et al. “Thyroid gland ectopias”. Annals of Otology, Rhinology & Laryngology 105.12 (1996):996-1000.
- Feisal TK., et al. “Unusual parapharyngeal lesion: aberrant thyroid gland”. Singapore Medical Journal 49.15 (2008): e137-e138.
- Subramony C., et al. “Follicular carcinoma arising in ectopic thyroid tissue: case report with fine-needle aspiration findings”. Diagnostic Cytopathology 16.1 (1997): 39-41.
- Sauk JJ., et al. “Papillary thyroid carcinoma in a lateral neck cyst: primary of ectopic thyroid tissue versus cystic metastasis”. The Journal of Laryngology and Otology 127.7 (2013): 724-727.
- Di Benedetto V. “Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: a case report”. Journal of Pediatric Surgery 32.12 (1997): 1745-1746.
- Babazade F., et al. “Thyroid tissue as a submandibular mass: a case report”. Journal of Oral Science 51.4 (2009): 655-657.
- Kousta E., et al. “Ectopic thyroid tissue in the lower neck with a coexisting normally located multinodular goiter and brief literature review”. Hormones 4.4 (2005): 231-234.
- Bersaneti JA., et al. “Ectopic thyroid presenting as a submandibular mass”. Head and Neck Pathology 5.1 (2011): 63-66.
- Gopal RA., et al. “Clinical profile of ectopic thyroid in Asian Indians: a single center experience”. Endocrine Practice 15.4 (2009): 322-325.
- Yoon JS., et al. “Clinical characteristics of ectopic thyroid in Korea”. Thyroid 17.11 (2007): 1117-1121.
- Choi YM., et al. “Papillary thyroid carcinoma arising from a thyroglossal duct cyst: a single institution experience”. Endocrine Journal 60.5 (2013): 665-670.
- Sidhu S., et al. “Thyroid papillary carcinoma in lateral neck cyst: missed primary tumour or ectopic thyroid carcinoma within a branchial cyst?” The Journal of Laryngology & Otology 114.9 (2000): 716-718.
- Matsumoto K., et al. “Thyroid papillary carcinoma arising in ectopic thyroid tissue within a branchial cleft cyst”. Pathology International 49.5 (1999): 444-446.
- Izenstark JL., et al. “The pyramidal lobe in thyroid imaging”. Journal of Nuclear Medicine 10.8 (1969): 519-524.
- Fish J and Moore RM. “Ectopic thyroid tissue and ectopic thyroid carcinoma: a review of the literature and report of a case”. Annals of Surgery 157.2 (1963): 212-222.
- Lianos G., “Ectopic thyroid carcinoma”. Giornale di Chirurgia 34.4 (2013): 114-116.
- Ranade AV., et al. “Anatomical variations of the thyroid gland: possible surgical implications”. Singapore Medical Journal 49.10 (2008): 831-834.
- Rao PN., et al. “Ectopic functioning thyroid tissue in the thyroglossal duct detected by radionuclide imaging”. Clinical Nuclear Medicine 30.9 (2005): 630.
- Lim-Dunham JE., et al. “Sonographic demonstration of a normal thyroid gland excludes ectopic thyroid in patients with thyroglossal duct cyst”. American Journal of Roentgenology 164.6 (1995): 1489-1491.
- Prado H., et al. “Lateral ectopic thyroid: a case diagnosed preoperatively”. Ear, Nose and Throat Journal 91.4 (2012): E14-E18.
- 25. Kushwaha JK., “Papillary carcinoma of thyroid arising from ectopic thyroid tissue inside branchial cleft cyst: a rare case”. BMJ Case Reports 9 (2012).
- Guerrissi JO. “Follicular variant of papillary carcinoma in submandibular ectopic thyroid with no orthotopic thyroid gland.” Journal of Craniofacial Surgery 23.1 (2012): 138-139.
- Shah BC., et al. “Ectopic thyroid cancer”. Annals of Thoracic and Cardiovascular Surgery 13.2 (2007): 122-124.
- Heshmati HM., et al. “Thyroglossal duct carcinoma: report of 12 cases”. Mayo Clinic Proceedings 72.4 (1997): 315-319.
- Go¨k U., et al. “Ectopic thyroid and Hashimoto’s thyroiditis arising from a thyroglossal duct cyst: a case report”. Kulak Burun Bogaz Ihtisas Dergisi 10.1 (2003): 29-32.
- Klubo-Gwiezdzinska., et al. “Ectopic cervical thyroid carcinoma-Review of the literature with illustrative case series”. Journal of Clinical Endocrinology and Metabolism 96.9 (2011): 2684-2691.
- Mazaferri EL. “Thyroid cancer in thyroglossal duct remnants: a diagnostic and therapeutic dilemma”. Thyroid 14.5 (2004): 335-336.
- Park MH., et al. “Papillary thyroglossal duct cyst carcinoma with synchronous occult papillary thyroid microcarcinoma”. Yonsei Medical Journal 51.4 (2010): 609-611.
- Talwar N., et al. “Lithiuminduced enlargement of a lingual thyroid”. Singapore Medical Journal 49.3 (2008): 254-255.
- Ohnishi H., et al. “Color Doppler ultrasonography: diagnosis of ectopic thyroid gland in patients with congenital hypothyroidism caused by thyroid dysgenesis”. Journal of Clinical Endocrinology and Metabolism 88.1 (2003): 5145-5149.
- Yang Y., et al. “Ectopic intratracheal thyroid”. Southern Medical Journal 103.5 (2010): 467-470.
- Toso A., et al. “Lingual thyroid causing dysphagia and dyspnoea. Case reports and review of the literature”. Acta Otorhinolaryngologica Italica 29.4 (2009): 213-217.
- Douglas PS and Baker AW. “Lingual thyroid”. British Journal of Oral the Maxillofacial Surgery 32.2 (1994): 123-124.
- Chawla M., et al. “Dual ectopic thyroid: case series and review of the literature”. Clinical Nuclear Medicine 32.1 (2007): 1-5.
- Nasiru Akanmu I and Mobolaji Adewale O. “Lateral cervical ectopic thyroid masses with eutopic multinodular goiter: an unusual presentation”. Hormones 8.2 (2009): 150-153.
- Galizia G., et al. “Ectopic thyroid: report of a case”. Giornale di Chirurgia 22 (2001): 85-88.
- Farrell ML and Forer M. “Lingual thyroid”. Australian and New Zealand Journal of Surgery 5.1 (1994): 135-138.
- Iglesias P., et al. Iodine 131 and lingual thyroid. Journal of Clinical Endocrinology and Metabolism 93.11 (2008): 4198-4199.
Citation:
Khalid S Aljabri., et al. “A Case of an Ectopic Papillary Thyroid Carcinoma Located in the Midline of the Neck. A Case Report
and Review of the Literature.” Archives of Endocrinology and Diabetes Care 1.2 (2018): 59-64.
Copyright: © 2018 Khalid S Aljabri., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.