Research Article
Volume 1 Issue 3 - 2018
Profile of Cardiovascular Risk in Patients with Subclinical and Overt Hypothyroidism with Special Reference to Carotid Intima Media Thickness (Cimt) and Hscrp (High Sensitive C - Reactive Protein) Level.
1Senior Resident in Medicine, RRMCH, Bangalore- 560074
2Professor & HOD, Department of General Medicine, RRMCH, Bangalore- 560074
3Associate Professor of Radiology, Department of Radiodiagnosis, RRMCH, Bangalore-560074
2Professor & HOD, Department of General Medicine, RRMCH, Bangalore- 560074
3Associate Professor of Radiology, Department of Radiodiagnosis, RRMCH, Bangalore-560074
*Corresponding Author: Anita Bhosale, Senior Resident in Medicine, RRMCH, Bangalore- 560074.
Received: June 15, 2018; Published: July 18, 2018
Abstract
Background: The present study was carried out to study various cardiovascular risks in both subclinical and overt hypothyroidism with special reference to carotid intima media thickness (CIMT) and high sensitive C-reactive protein (hsCRP) level. Carotid intima media thickness (CIMT) is a close marker of early atherosclerotic changes and is a widely accepted surrogate end point for cardiovascular events. This study showed that subjects with hypothyroidism have increased C-reactive protein values. Hypothyroidism also has been associated with increased risk for atherosclerosis.
Materials and Methods: A Prospective observational clinical study is done on hypothyroid (Subclinical and overt) patients involving 100 patients in the age group of > 18 years (of either sex) both overt (TSH level > 10 miu/l) and subclinical hypothyroidism (TSH level 4-10miu/l) group, then correlated CIMT and hSCRP in hypothyroid (Subclinical and overt) patients along with other atherosclerotic risk factors.
Results: In this study, age of patients ranged from 25 to 65 years and mean age was 42.64 ± 7.55 years.90 patients were females and 10 were males, mean BMI was 24.88 ± 2.02.53 patients were diagnosed as subclinical hypothyroidism while 47 patients were diagnosed to have overt hypothyroidism. In this study it was found that hypothyroidism is associated with hypercholesterolemia, hypertriglyceridemia and high serum LDL-C but there was no significant association between hypothyroidism and HDL-C.57 cases were having hSCRP level of > 3 mg/l suggestive of high risk, 36 cases were having hSCRP between 1-3 mg/l which is suggestive of average risk, 60 cases had high CIMT value of > 0.7, there was a positive association between hypothyroidism and diastolic hypertension, LVDD with a P value of < 0.001 which was significantly high. There was a positive correlation between hsCRP, CIMT with other atherosclerotic risk factors (diastolic hypertension, lipid parameters and LVDD), correlated values between CIMT and hSCRP which showed a positive correlation with a P value of < 0.001 which was highly significant.
Conclusion: Incidence of hypothyroidism is more common in females. Subclinical hypothyroidism (53%) is more common when compared to overt hypothyroidism (47%). High CIMT is associated with high cardiovascular risk. High hSCRP in hypothyroid both subclinical and overt hypothyroid subjects are at high risk for cardiovascular morbidity. High prevalence of LVDD in hypothyroidism. Dyslipidemia in hypothyroidism increases cardiovascular morbidity. Pearson correlation between TFT and CIMT, between TFT and hSCRP and between CIMT and hSCRP showed a positive correlation which increases cardiovascular morbidity in hypothyroidism. CIMT and hsCRP also showed positive correlation with other atherosclerotic risk factors such as high serum total cholesterol, high LDL-C and high triglycerides. CIMT is an important noninvasive marker of atherosclerosis which can be used for assessment of cardiovascular risk.
Introduction
Subclinical hypothyroidism is defined as an increased serum TSH level which is associated with normal total or free T4 and T3 values. The prevalence has been reported to range from 6-8% in women and 3% in men (up to 10% in women more than 60 years) [1]. In subclinical hypothyroidism, the serum TSH being increased but the circulating levels of thyroid hormones are within the normal range. Overt hypothyroidism is defined as a clinical syndrome of hypothyroidism associated with elevated TSH & decreased serum levels of T4 or T3.The onset of hypothyroidism is a progressive process starting from mild thyroid failure (subclinical hypothyroidism) to overt hypothyroidism & its effect on cardiovascular system have been well recognized.
The aetiologies of subclinical and overt hypothyroidism are identical. Chronic autoimmune thyroiditis (Hashimoto's disease) accounts for the majority of cases. Around 54% of patients with subclinical hypothyroidism have Hashimoto's disease with increased serum concentrations of ant thyroid microsomal or ant thyroid peroxidise antibodies [2]. Subclinical hypothyroidism increases the risk of coronary heart disease (CHD) by adversely affecting cardiovascular risk factors. A cross-sectional study showed that subjects with subclinical hypothyroidism have increased C-reactive protein values. Subclinical hypothyroidism also has been associated with increased risk for atherosclerosis. The most important fact is that the progression of subclinical hypothyroidism to overt hypothyroidism during its natural history. The Risk is more if the subject is positive for thyroid peroxidase antibody or if the serum TSH is more than 10uIU/ml. In a recent prospective study on the spontaneous course of patients with subclinical hypothyroidism by Gerold Huber and team they concluded that risk factors for progression to overt hypothyroidism were base line TSH > 12uIU/mL, decreased thyroid reserve and presence of thyroid peroxidase antibody [3].
Carotid intima media thickness (CIMT) is a close marker of early atherosclerotic changes and is a widely accepted surrogate end point for cardiovascular events. The association of CIMT with major cardiovascular risk factors has been well demonstrated. Nagasaki., et al. [4] demonstrated Carotid intima media thickening in patients with overt hypothyroidism and Kim., et al. [5] in subclinical hypothyroidism which was regressed after levothyroxine replacement [6]. Caka., et al. have demonstrated higher CIMT in primary hypothyroid patients. They also found positive correlation between lipids, CIMT, & TSH levels. They have concluded that CIMT is an objective sign of accelerated atherosclerosis in patients with primary hypothyroidism [6,7]
Other studies which showed regression of CIMT after thyroxin replacement are Monzani., et al. [8] Cakal., et al [9], and llknur., et al. [7] This study mainly focuses on cardiovascular risks in subclinical and overt hypothyroidism with special reference to CIMT and hSCRP level.
Aim and Objectives
- To study the clinical and lab profile of patients with subclinical and overt hypothyroidism.
- To study the CIMT and hSCRP level in patients with subclinical and overt hypothyroidism.
Materials and Methods
A Prospective observational clinical study is done on hypothyroid (Subclinical and overt) patients attending General Medicine out patients clinics at Rajarajeswari Medical College and Hospital, Bengaluru. We consecutively included 100 patients both overt (TSH level >10 miu/l) and subclinical hypothyroidism (TSH level 4-10miu/l) group. We then correlated CIMT and hSCRP in hypothyroid (Subclinical and overt) patients along with other atherosclerotic risk factors. The duration of study was of 12 months (1 year).
Inclusion criteria
- Patients with subclinical and overt hypothyroidism, diagnosed based on serum TSH level in the age group of > 18 years (of either sex)
- TSH level 4-10 miu/l:Subclinical hypothyroidism
- TSH level >10 miu/l:Overt hypothyroidism
Exclusion criteria
- Diabetes Mellitus
- Pregnancy
- Patients taking levothyroxine, Oral Contraceptive Pills , statins within 3 months before enrollment
- Primary dyslipidemia
- Critically ill patients
- Patients with concomitant inflammatory disease
- Smokers
- Alcoholics
- Patients with pituitary –hypothalamic disorders
- Malignancy
Methodology of Study
Prospective observational clinical study was conducted on 100 patients selected based on those satisfying the inclusion criteria. After the approval by the ethical clearance committee, written informed consent was obtained from all the patients included in the study. Detailed history including medication, smoking, alcohol intake, anthropometric measurements like height, weight, BMI were noted. Laboratory data consisted of blood sugar, blood urea, serum creatinine, T3, T4, TSH, and fasting lipid profile. T3, T4 and TSH were measured by IMMULITE 1000 immunoassay. Fasting lipid profile was done with the ERBA XL300 auto analyser. hSCRP was analysed using Immunoturbidometry-ELISA method.
Prospective observational clinical study was conducted on 100 patients selected based on those satisfying the inclusion criteria. After the approval by the ethical clearance committee, written informed consent was obtained from all the patients included in the study. Detailed history including medication, smoking, alcohol intake, anthropometric measurements like height, weight, BMI were noted. Laboratory data consisted of blood sugar, blood urea, serum creatinine, T3, T4, TSH, and fasting lipid profile. T3, T4 and TSH were measured by IMMULITE 1000 immunoassay. Fasting lipid profile was done with the ERBA XL300 auto analyser. hSCRP was analysed using Immunoturbidometry-ELISA method.
Patients were subjected for 2D ECHO.CIMT thickness will be done by using high resolution B mode ultrasonography system having an electrical linear transducer mid frequency of 7.5 MHz scans will be performed on both right and left extra cranial carotid arteries. The IMT is measured as a distance from the leading edge of the 1st echogenic line to the 2nd echogenic line. The 1st echogenic line represents the luminal intimal interface and the second line is produced by collagen containing upper layer of intimal adventitia. At each longitudinal projection determination of IMT’s were conducted at the side of greatest thickness and at 2 points 1 cm upstream and 1 cm downstream from side of greatest thickness as described. The mean of 6 IMT measurements from both sides will be used as representative value for each subject. The cut off for normal CIMT was taken as 0.8 mm in Indian population as in different studies the cut off was found to correlate with vascular risks.
Results
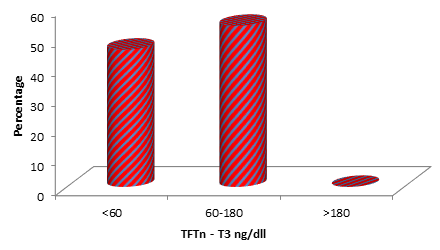
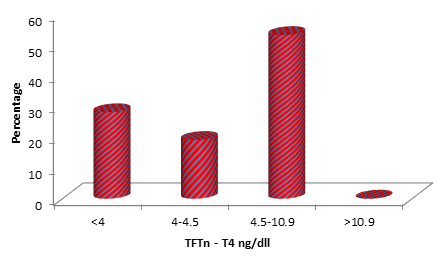
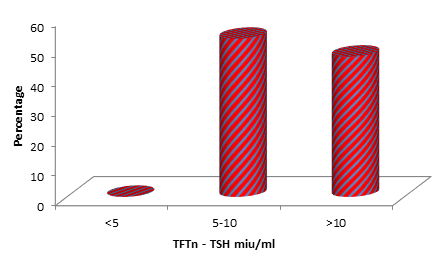
Among 100 patients, age ranged from 25 to 65 years and mean age was 42.64 ± 7.55 years, 90 patients were females and 10 were males. 40 % of patients (n = 40) were having BMI between 18.5-25 (overweight) and 60% of cases (n = 60) were having BMI between 25-30 (obese). Mean BMI was 24.88 ± 2.02. Out of 100 cases studied 53% of cases (n = 53) had T3 value between 60-180 ng/dl, 47% of cases (n = 47) had T3 value of < 60 ng/d (Figure 1a) l. While 28% of cases (n = 28) had T4 value of < 4 mcg/dl, 19% of cases (n = 19) had T4 value between 4-4.5 mcg/dl, 53% of cases (n = 53) had T4 value between 4.5-10 mcg/dl (Figure 1b). 53% of cases (n = 53) had TSH value between 5-10 miu/ml and 47% of cases (n = 47) had TSH of >10 miu/ml (Figure 1C).
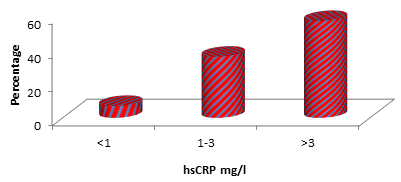
Out of 100 cases 71% (n = 71) had high serum total cholesterol which was between 200-280 mg/dl, 5% (n = 5) had very high serum total cholesterol which was >280 mg/dl and 24% (n = 24) had normal serum total cholesterol (< 200).66% of patients (n = 66) had serum HDL of > 40 mg/dl and 34% of patients had serum HDL level between 30-40 mg/dl.84% of patients (n = 84) had serum LDL between 100-160mg/dl, 7% of cases (n = 7) had > 160 mg/dl and 9% of cases (n = 9) had serum LDL of < 100 mg/dl. 55% of patients (n = 55) had serum TGS between 150-199 mg/dl, 42% of cases (n = 42) had serum TGS between 200-499 mg/dl and 3% (n = 6) of cases had serum TGS of < 150mg/dl. Among 100 cases, LVDD was present in 64% of cases (n = 64) on 2DECHO while 2DECHO was normal in 36% of cases (n = 36). Among 100 cases studied 57% of cases (n = 57) were having hSCRP level of > 3 mg/l, 36% of cases (n = 36) were having hSCRP between 1-3 mg/l and 7% of patients (n = 7) had hSCRP level of < 1 mg/l (Figure 2).
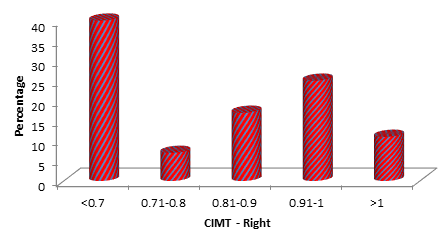
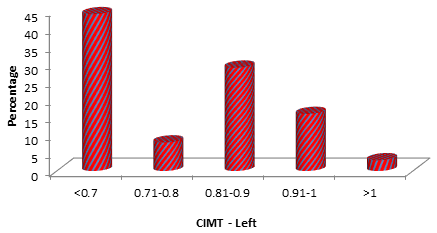
Among 100 cases 40% of cases (n = 40) had CIMT mean value of < 0.7, 60% of cases had CIMT value of > 0.7 (8 cases had CIMT between 0.71-0.8, 21 cases had 0.81-0.9, 22 cases had 0.91-1 and 9 cases had CIMT value of > 1) Figure 3a and b.
| Pair | r value | P value |
| hsCRP (mg/l) vs. T3 (ng/dl) | -0.698 | < 0.001** |
| hsCRP (mg/l) vs. T4 (mcg/dl) | -0.796 | < 0.001** |
| hsCRP (mg/l) vs. TSH (miu/ml) | 0.702 | < 0.001** |
Table 1: Pearson correlation of HSCRP with TFT parameters.
When we correlated values of hSCRP with serum T3, T4 and TSH levels the P value found to be < 0.001 which is highly significant (Table 1)
| Pair | r value | P value |
| CIMT (Mean) vs. T3 (ng/dl) | -0.648 | < 0.001** |
| CIMT (Mean) vs. T4 (mcg/dl) | -0.693 | < 0.001** |
| CIMT (Mean) vs. TSH (miu/ml) | 0.645 | < 0.001** |
Table 2: Pearson correlation of CIMT with TFT parameters.
The correlation between CIMT and TFT (T3, T4 and TSH) levels found to be highly significant with a P value of < 0.001. (Table 2)
| r value | P value | |
| hsCRP (mg/l) vs. CIMT Right | 0.758 | < 0.001** |
| hsCRP (mg/l) vs. CIMT Left | 0.752 | < 0.001** |
| hsCRP (mg/l) vs. CIMT (Mean) | 0.756 | < 0.001** |
Table 3: Pearson correlation of HSCRP with CIMT.
The correlation between values of hSCRP and CIMT (right, left and mean) was found to be highly significant with a P value of < 0.001. (Table 3)
Discussion
In our study, the age of patients ranged from 25 to 65 years and mean age was 42.64 ± 7.55 years.90 patients were females and 10 were males. Hypothyroidism is much more common in females [1]. The mean BMI in our study was found to be 24.88 ± 2.02. Among 100 cases 53 patients were diagnosed as subclinical hypothyroidism (high TSH and normal T4 and T3 values) while 47 patients were diagnosed to have overt hypothyroidism (high TSH and reduced T3 and T4). Subclinical hypothyroidism is much more common than overt hypothyroidism [10]. In our study it was found that hypothyroidism is associated with hypercholesterolemia, hypertriglyceridemia and high serum LDL-C but there was no significant association between hypothyroidism and HDL-C. Ibrahim M., et al. showed that among subjects with subclinical hypothyroidism, there was a significant increase (P< 0.001) in the levels of total Cholesterol, and triglycerides when compared with the controls. The LDL-C levels were also found to be high in the subclinical hypothyroid group (P < 0.03). No differences in the levels of HDL-C were observed among the study groups [11]. In our study, 57 cases were having hSCRP level of > 3 mg/l suggestive of high risk, in this 24 cases were subclinical hypothyroidism and 33 cases were overt hypothyroidism. 36 cases were having hSCRP between 1-3 mg/l which is suggestive of average risk. Tuzcu., et al. in 2005 in their study of 77 subclinical hypothyroid patients of Tokyo, Japan also found to have elevated hSCRP levels and was significant (P Value = 0.0001) [12]. Among 100 cases 60 cases had CIMT value of > 0.7 (8 cases had CIMT between 0.71-0.8, 21 cases had 0.81-0.9, 22 cases had 0.91-1 and 9 cases had CIMT value of > 1) with a P value of < 0.001 which was highly significant. Caka., et al. have demonstrated higher CIMT in primary hypothyroid patients. They also found positive correlation between lipids, CIMT, & TSH levels. They have concluded that CIMT is an objective sign of accelerated atherosclerosis in patients with primary hypothyroidism [6,7]. Nagasaki., et al. [4] demonstrated carotid artery intima media thickening in patients with overt hypothyroidism. Increased risk of cardiovascular morbidity like left ventricular diastolic dysfunction in subclinical and overt hypothyroidism with dyslipidaemia and increased hSCRP and increase CIMT was looked in to in our study. Incidence of LVDD was significantly high, about 64% of hypothyroid patients had LVDD in our study. Biondi B., et al. in 1999 did a similar study in Naples, Italy on 26 subclinical hypothyroid subjects and the results were similar with high incidence of LVDD and was significant (P value 0.001) [13]. There was a positive correlation between hsCRP, CIMT with other atherosclerotic risk factors (diastolic hypertension, lipid parameters and LVDD). We also correlated values between CIMT and hsCRP which showed a positive correlation with a P value of < 0.001 which was highly significant. Similar study was done by R Karoli and group which was the first Hospital based study tried to correlate CIMT and hsCRP in patients with hypothyroidism with a P value of < 0.001 which was highly significant. They found that CIMT and hsCRP showed positive correlation with other atherosclerotic factors (diastolic hypertension, and LDL-C) [14].
Conclusions
Most of subjects (47%) were in the age group of 30-40 years, as primary hypothyroidism is more common among this age group.Incidence of hypothyroidism is more common in females. Subclinical hypothyroidism (53%) is more common when compared to overt hypothyroidism (47%). 60% of cases had high CIMT value, High CIMT is associated with high cardiovascular risk. hsCRP was elevated (> 3 mg/dl) in 57% of cases (24 cases were subclinical hypothyroidism and 33 cases were overt hypothyroidism), indicating hypothyroid both subclinical and overt hypothyroid subjects are at high risk for cardiovascular morbidity. Left ventricular diastolic dysfunction was present in 64% of hypothyroid subjects in our study indicating high prevalence of LVDD in hypothyroidism. Left ventricular diastolic dysfunction was present in high risk subjects (hsCRP > 3 mg/dl and CIMT value of > 0.7mm). Lipid abnormalities are seen in hypothyroidism subjects in the form of significant elevation of total cholesterol, LDL and triglycerides while changes in HDL are not significant. Follow up of treated patients are necessary to assess the benefit of thyroxin in reverting the lipid abnormalities.Dyslipidemia in hypothyroidism increases cardiovascular morbidity.
Pearson correlation between TFT and CIMT showed a positive correlation. Pearson correlation between TFT and hsCRP showed a positive correlation. Pearson correlation between CIMT and hsCRP showed a positive correlation which increases cardiovascular morbidity in hypothyroidism. CIMT and hsCRP also showed positive correlation with other atherosclerotic risk factors such as high serum total cholesterol, high LDL-C and high triglycerides. CIMT is an important noninvasive marker of atherosclerosis which can be used for assessment of cardiovascular risk. So it is important to screen high risk population for hypothyroidism especially subclinical and its adverse effects on cardiovascular system so that therapy can be initiated early and the risks minimized. It is very important to follow up the treated cases for assessing the benefit of thyroxin replacement on different aspects of subclinical hypothyroidism namely the effect on symptoms, improvement in lipid abnormalities and also to avoid over treatment. Untreated cases have to be followed up for evidence of progression of disease.CIMT is an important noninvasive marker of atherosclerosis which can be measured by noninvasive method. So it is important to screen high risk population for hypothyroidism especially subclinical and its adverse effects on cardiovascular system so that therapy can be initiated early and the risks minimized.
It is very important to follow up the treated cases for assessing the benefit of thyroxin replacement on different aspects of subclinical hypothyroidism namely the effect on symptoms, improvement in lipid abnormalities and also to avoid over treatment. Untreated cases have to be followed up for evidence of progression of disease.CIMT is an important noninvasive marker of atherosclerosis which can be measured by noninvasive method. So it is important to screen high risk population for hypothyroidism especially subclinical and its adverse effects on cardiovascular system so that therapy can be initiated early and the risks minimized. It is very important to follow up the treated cases for assessing the benefit of thyroxin replacement on different aspects of subclinical hypothyroidism namely the effect on symptoms, improvement in lipid abnormalities and also to avoid over treatment. Untreated cases have to be followed up for evidence of progression of disease. CIMT is an important noninvasive marker of atherosclerosis which can be measured by noninvasive method.
References
- Harrison’s Principles of Internal Medicine, 19th edition. Chapter 335. 2230.
- Hamburger JI., et al. “Factitious elevation of thyrotropin in euthyroid patients”. NEJM 313 (1985): 267-268.
- Huber G., et al. “Prospective Study of the Spontaneous Course of Subclinical Hypothyroidism: Prognostic Value of Thyrotropin, Thyroid Reserve, and Thyroid Antibodies”. The Journal of Clinical Endocrinology & Metabolism 87.7 (2002): 3221-3226.
- Nagasaki T., et al. “Decrease in carotid intima media thickness in hypothyroid patients after normalization of thyroid function”. Clinical Endocrinology 59.5 (2003): 607-612.
- Kim SK., et al. “Regression of the increased common carotid artery intima media thickness in subclinical hypothyroidism replacement”. Endocrine Journal 56.6 (2009): 753-758.
- Biondi B and Klein I. “Hypothyroidism as a risk factor for cardiovascular disease”. Endocrine system 24.1 (2004): 1-13.
- llknur ozturk Unsal., et al. “Effect of levothyroxine on the progression of carotid intima-media thickness in subclinical hypothyroidism patients: a meta-analysis”. Diabetes and endocrinology 7.10 (2017).
- Monzani F., et al. “Effect of levothyroxine replacement on lipid profile and intima media thickness in subclinical hypothyroidism: a double blind, placebo-controlled study”. The Journal of Clinical Endocrinology & Metabolism 89.5 (2004): 2099-2106.
- Cakal E., et al. “Effect of levothyroxine replacement therapy on carotid intima –media thickness in patients with primary hypothyroidism”. Experimental and Clinical Endocrinology & Diabetes 117.6 (2009): 294-300.
- TK Mishra., et al. “Left Ventricular Dysfunction in Patients with Subclinical Hypothyroidism and its Reversibility after Hormone Therapy”. The Journal of the Association of Physicians of India 53 (2005): 943-946.
- Ibrahim M., et al. “Effects of subclinical hypothyroidism on important serum lipids values of Sudanese women”. Journal of Chinese Clinical Medicine 5.7 (2010).
- Alpaslan Tuzcu et al. “Subclinical hypothyroidism may be associated with elevated high-sensitive c-reactive protein (low grade inflammation) and fasting hyperinsulinemia”. Endocrine journal 52.1 (2005): 89-94.
- Biondi B., et al. “Left ventricular diastolic dysfunction in patients with subclinical hypothyroidism”. The Journal of Clinical Endocrinology & Metabolism 84.6 (1999): 2064–2067.
- R Karoli. “Hospital based study of carotid intima media thickness and high sensitivity C-reactive protein in young hypothyroid patients”. JIACM 15.2 (2014): 116-119.
Citation:
Anita Bhosale., et al. “Profile of Cardiovascular Risk in Patients with Subclinical and Overt Hypothyroidism with Special
Reference to Carotid Intima Media Thickness (Cimt) and Hscrp (High Sensitive C - Reactive Protein) Level.” Archives of Endocrinology
and Diabetes Care 1.3 (2018): 120-128.
Copyright: © 2018 Anita Bhosale., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.