Research Article
Volume 2 Issue 1 - 2018
Effect of Various Stress Relaxation Exercises on Electroencephalography, Sympathetic Skin Response and Type-2 Diabetes Mellitus
1MD (Internal Medicine), Senior Consultant, Department of Internal Medicine,
2MD (Community Medicine & Biostatistics), honorary consultant
3B.H.M.S. Resident Doctor
4M. SC. PGDYHS Department Yoga and Physical education
5MD (Pathology), senior consultant, department of Pathology and Biochemistry Mittal Hospital and Research Centre, Ajmer, Rajasthan, India
2MD (Community Medicine & Biostatistics), honorary consultant
3B.H.M.S. Resident Doctor
4M. SC. PGDYHS Department Yoga and Physical education
5MD (Pathology), senior consultant, department of Pathology and Biochemistry Mittal Hospital and Research Centre, Ajmer, Rajasthan, India
*Corresponding Author: Tarun Saxena, MD (Internal Medicine), Senior Consultant, Department of Internal Medicine, Mittal Hospital and Research Centre, Ajmer, Rajasthan, India.
Received: September 01, 2018; Published: September 13, 2018
Abstract
Background/objectives: Type 2 diabetes is a multifactor disease. Various studies have linked stress and diabetes. Still prospective study assessing the effect of various stress relaxation methods on glycemic parameters, lipid profile, EEG and SSR is lacking. Therefore the study was planned to see the effects of various stress relaxation methods in management of diabetes.
Methods: This is a randomized double-blind, interventional, active control trial. Arbitrarily, a sample of 50 confirmed cases of type-2 diabetes mellitus was selected for the study. Cases were randomly divided into 2 groups; group 1 (n = 30 control). Group 2 interventional group (n = 20). Group 2 was again subdivided into two subgroups 2A (n = 10) who practiced yogic relaxation exercises like pranayama, asanas and kriyas, subgroup 2B (n = 10) who practiced Vipassana mental relaxation technique. Stress scaling (perceived stress scale/ PSS), mental health life style factors (i.e. working mental hours, sleep duration etc. were assessed. Examination included, Waist: Hip ratio (W: H), EEG (electroencephalography), SSR (sympathetic skin response), fasting and post prandial glucose (FBG/PPBG), Glycosylated hemoglobin (HbA1c) and lipid profile initial and after 12 weeks.
Results: Initially all groups were comparable, in W: H ratio, FBG/PPBG/HbA1c, lipid profile, EEG and SSR findings. (Desynchronized activity in EEG, increased basal sympathetic discharge, high FBG/PPBG/HbA1c, impaired lipid profile). After 12 weeks sub group 2 B who practiced Vipassana showed synchronization in EEG, reduction in basal sympathetic discharge, and significant improvement in FBG/PPBG/HbA1c and lipid profile.
Conclusion: Chronic mental exhaustion and chronic stress are desynchronized state of brain, associated with increased basal sympathetic discharge. Increase in sympathetic discharge produces insulin resistance, impaired insulin release and diabetes. Vipassana/mental rest reduces expenditure of neurotransmitters, reduces stress, synchronizes brain, reduces basal sympathetic discharge and helps in control of diabetes.
Keywords: Stress; Type- 2 diabetes mellitus; Electro-encephalography; Sympathetic skin response
Introduction
Type 2 diabetes mellitus is a disease characterized by chronic hyperglycemia and multisystem complications, which is an important cause of morbidity and mortality. Besides sedentary lifestyle/physical inactivity, genetic defect, obesity, diet, environmental factors, stress is an important risk factor in causation or initiation of the disease. (Park & Park 2017) [1]
According to Dorland’s medical dictionary, stress is the sum of biological reactions to any adverse stimulus, physical, mental or emotional, internal that tends to disturb an organism’s internal homeostasis. [2] It may be external (environmental, psychological, or social situations) or internal (illness).
During past few years many working people have documented association between stress and type- 2 diabetes mellitus. Saxena., et al. (2013) have found a clear association between chronic stress, mental exhaustion and diabetes. The study also has correlated findings with EEG (electroencephalography) and SSR (sympathetic skin response) [3]. Another study by Harris et al. has found that stress increases the rise of tye-2 diabetes onset in women [4]. Few more studies have linked stress and diabetes [5-11]. Demoski (1970) also reported that stress intensifies the known preexistent diabetes mellitus, brings the unrecognized diabetes to clinical recognition and may convert pre-diabetes to frank diabetes mellitus [12]. All these previous studies indicate the role of stress in diabetes. Still there is insufficient literature about prospective work assessing reduction in stress and mental exhaustion and its effect on glycemic parameters, lipid profile, EEG and SSR. Therefore the study was planned to assess the effect of various stress relaxation methods to reduce stress/mental exhaustion in management of diabetes [13-18].
Materials and Methods
Study type: This is a randomized, double-blind, interventional, parallel group, active control trial. The study was done in the department of Internal Medicine and the department of Yoga and Physical health in Mittal hospital and Research Centre, Pushkar road Ajmer, and Keshvam hospital Maharana pratap Nagar Ajmer, Rajasthan, India. Patients in these institutes come from all the parts of the city and nearby villages (encompassing an area of 20-25 kilometers) representing a population of twenty lakhs.
Case selection, study period and study methods: Arbitrarily, a sample of 50 confirmed cases of type-2 diabetes mellitus coming regularly to the hospital for the last two years were selected for the study. Informed written consent and approval of the institutional ethical committee was taken (Initial diagnosis based on glycosylated hemoglobin (HbA1c > 6.5%). Cases were randomly divided into 2 groups; group 1 (n = 30 control). Group 2 interventional group (n = 20) (group 2). Group 2 was again randomly subdivided into two subgroups; subgroup 2A (n = 10) who practiced various yogic relaxation exercises like pranayama, asanas and kriyas, subgroup 2B (n = 10) who practiced Vipassana mental relaxation technique. The age group of the selected cases was between 45-50 years, comprising both males and females. All groups and subgroups were age and sex matched. The patients were studied from January 2015 to December 2017. The symptoms, anthropometric measurements (W: H ratio-waist hip ratio) stress scaling, and EEG, SSR was recorded by specific technician in the hospital and checked by a consultant on that day. The following parameters were taken into consideration-.
Detailed history including family history
Anthropometric measurements (W: H ratio-waist hip ratio)
Vital parameters (resting pulse rate, blood pressure, respiratory rate)
Anthropometric measurements (W: H ratio-waist hip ratio)
Vital parameters (resting pulse rate, blood pressure, respiratory rate)
Stress scaling: Various factors were analyzed through a questionnaire based mainly on PSS (Perceived stress scale) with rating 0,1,2,3 or 4 which indicates severity; 0= never, 1= almost never,2 = sometimes, 3 = fairly often, 4 = very often (total 17 items/points in stress with maximum score of 68; normal range 0-16, mild stress 17-20, moderate 21-30, severe > 30/68). Various points examined were – attached with anxiety, tension, flow/crowding of ideas, loss of control etc. [19]
Subjective assessment: History of various mental health life style factors (i.e. working mental hours, sleep duration etc. duration of presence of above habit [3]
EEG (Electroencephalography): initial and after 12 weeks EEG was done on a 16 channel system in a dark silent room. Basal rhythm was observed in eye closure after few minutes in a relaxed state. (RMS Recorder and Medicare system) [3]
SSR (sympathetic skin response) initial and after 12 weeks; SSR was done with standard protocol in supine, relaxed, semi darkened room with ambient temperature control at 22-24°C, in the upper limbs. Hand grip and cold presser was used as provocative methods. Skin potential changes during and between the tests were analyzed by a computer. Latency was measured from the onset of stimulus artifact to the beginning of response. Amplitude was recorded peak to peak. (RMS Recorder and Medicare system) [20,21]
Blood investigations: Dry Chemistry (vitros 250 by ortho) method was used.
Glycemic parameters
FBG- Fasting blood glucose (Glucose oxidase method) [22]
PPBG- Post prandial blood glucose (Glucose oxidase method) [22]
HbA1c-Glycosylated hemoglobin (Turbid metric immunoassay method) [23]
Glycemic parameters
FBG- Fasting blood glucose (Glucose oxidase method) [22]
PPBG- Post prandial blood glucose (Glucose oxidase method) [22]
HbA1c-Glycosylated hemoglobin (Turbid metric immunoassay method) [23]
Lipid profile
Tgl- Triglyceride (Enzymatic method) [24]
HDL (High density lipoprotein)cholesterol (Non HDL precipitation method followed by enzymatic reaction method)
LDL (low density lipoprotein) & VLDL (very low density lipoprotein) Estimations- Calculated
Tgl- Triglyceride (Enzymatic method) [24]
HDL (High density lipoprotein)cholesterol (Non HDL precipitation method followed by enzymatic reaction method)
LDL (low density lipoprotein) & VLDL (very low density lipoprotein) Estimations- Calculated
Exclusion Criteria: Patients on insulin therapy, having a history of thyroid disorders, smoking, ischemic heart disease, hypertension, other medical disorders, and those who did not participate regularly for the period of 12 weeks were excluded from the study.
Intervention: The patients practiced exercises after completing routine activities in the morning and at least 4 hours after lunch in the evening. No change in dosage of drugs was done during 12 weeks period.
Group 1(control n = 30) who performed walking 45 minutes twice daily at a normal pace in a ground.
Group 2 (study group n = 20) who performed various relaxation exercises.
Sub group 2A (n = 10)who performed various yogic relaxation exercises[13-18]
Group 2 (study group n = 20) who performed various relaxation exercises.
Sub group 2A (n = 10)who performed various yogic relaxation exercises[13-18]
Pranayama: These exercises consists of various respiratory inhalation- exhalation techniques- various pranayama practiced were
- Nadi Suddhi
- Anuloma-Viloma
- Bhramari
Asanas: These exercises involve fixed postures predominantly affecting abdominal musculature- various asanas practiced were (figure 1).
Asanas practiced in standing position:
- Ardha Cakrasana (half-wheel posture)
- Pada Hastasana (Forward-bend posture)
Asanas practiced in sitting position:
- Sasankasana (Moon posture)
- Pacimatanasana (Posterior stretching)
- Ardha matsyendrasana (The half-twist posture)
Asanas practiced in lying position:
- Bhujangasana (Serpent posture)
- Salabhasana (Locust posture)
Kriya: These exercises involves active movement of abdominal wall muscles-
- Agnisar kriya
Vipassana: Sub group 2B (n = 10) who performed Vipassana relaxation technique 45 minutes twice daily for 12 weeks. Vipassana is also known as silent meditation retreat. It requires the novice to maintain strict silence. Main steps of Vipassana are [25,26]
- Not killing any species.
- Not lying, therefore you pledge to remain fully silent (most important step, silence preserves mental energy).
- No sexual misconduct (men and women are strictly separated).
- No intoxicants.
- In simple words it is a method that is based upon spending less from brain i.e. no active mental work viz- reading, writing, and speaking. No distraction- no Television, no mobile, no laptop etc. Though it is said to be meditation but it is a relaxation technique. Person is asked not to concentrate actively. It rejuvenates exhausted brain and reduces stress.
Outcome measurement Changes in glycemic parameters, lipid profile, EEG and SSR after 12 weeks.
Results
| Group 1 | Subgroup 2A | Subgroup 2B | |
| Mean age (years) | 47 | 46 | 46 |
| Male % | 52% | 53% | 51% |
| Female % | 48% | 47% | 49% |
| Positive family history | 35% | 33% | 32% |
| Good physical activity | 84 % | 91% | 90% |
| Pulse rate/minute | 84 ± 3 | 80 ± 3 | 82 ± 4 |
| Blood pressure mm Hg | 132 ± 4/78 ± 3 | 126 ± 6/76 ± 4 | 138 ± 4/78 ± 3 |
| Respiration rate/min | 18 ± 3 | 17 ± 2 | 16 ± 2 |
| W:H ratio initial | 0.843 ± 0.037 | 0.831 ± 0.037 | 0.844 ± 0.029 |
| After 12 weeks | 0.849 ± 0.040 | 0.835 ± 0.040 | 0.803 ± 0.012 |
| Significance (P) value | 0.324 | 0.001 |
Table 1: Vital parameters & Waist: Hip ratio.
| Mental health life style factors | Group 1 | Sub group 2A | Sub group 2B |
| a) Working mental hours | |||
| >7 hours | 85% | 82% | 91% |
| b) Mental rest | |||
| Week end | 14% | 15% | 17% |
| Month end | 26% | 24% | 28% |
| No clear rest | 60% | 61% | 55% |
| c)Sleep duration | |||
| < 7 hours | 48% | 51% | 50% |
| d)Presence of above factors | |||
| >5 years | 92% | 88% | 86% |
| e)PSS (perceived stress scale) >34/68 | 81% | 92% | 90 % |
Table 2: Assessment of stress factors/mental health.
| Groups | Group 1 | Sub group 2A | Sub group 2B |
| Initial FBG mg% | 164.77 ± 19.89 | 155.20 ± 20.78 | 166.40 ± 19.31 |
| FBG after 12 weeks mg% | 154.33 ± 19.41 | 152.2 ±19.81 | 88.40 ± 6.85 |
| Statistical significance | ---- | P 0.76 | P < 0.001 |
| Initial PPBG mg% | 252.17 ± 38.20 | 233.00 ± 21.1 | 255.50 ± 39.86 |
| PPBG after 12 weeks mg% | 237.60 ±37.80 | 223.6±24.4 | 165.40 ±15.63 |
| Statistical significance | ----- | P 0.27 | P < 0.001 |
| Initial HbA1c % | 11.65 ± 1.19 | 11.10 ± 0.58 | 10.6 ± 0.81 |
| HbA1c after 12 weeks % | 11.56 ± 1.26 | 10.83 ± 0.60 | 6.36 ± 0.76 |
| Statistical significance | ------ | P 0.02 | P < 0.001 |
Table 3: Glycemic parameters.
| Groups | Group 1 | Subgroup 2A | Subgroup 2B |
| Mean serum cholesterol in mg% | |||
| Initial | 217.60 ± 20.48 | 211.90 ± 15.90 | 217.40 ± 25.31 |
| After 12 weeks | 219.00 ± 21.63 | 207.30 ± 15.17 | 205.00 ± 25.04 |
| Statistical significance | P 0.123 | P 0.096 | |
| Mean serum HDL mg% | |||
| Initial | 36.93 ± 6.44 | 34.50 ± 5.40 | 33.20 ± 4.31 |
| After 12 weeks | 37.20 ± 5.64 | 35.40 ± 3.66 | 44.90 ± 3.90 |
| Statistical significance | P 0.353 | P < 0.001 | |
| Mean serum LDL mg% | |||
| Initial | 151.80 ± 17.06 | 146.80 ±16.17 | 157.60 ± 20.88 |
| After 12 weeks | 151.73 ± 16.14 | 145.40 ± 14.39 | 139.90 ± 19.62 |
| Statistical significance | P 0.278 | P 0.065 | |
| Mean serum VLDL mg% | |||
| Initial | 28.60 ± 6.95 | 31.40 ± 7.60 | 26.60 ± 6.19 |
| After 12 weeks | 28.20 ± 8.31 | 27.90 ±7.95 | 21.60 ± 5.56 |
| Statistical significance | P 0.921 | P 0.025 | |
| Mean serum Triglycerides mg% | |||
| Initial | 143.00 ± 34.75 | 157.00 ± 38.02 | 133.30 ± 30.93 |
| After 12 weeks | 137.67 ± 38.92 | 136.00 ± 38.77 | 108.00 ± 27.81 |
| Statistical significance | P 0.907 | P 0.032 |
Table 4: Lipid profile.
Statistical Analysis
Collected data were entered in computer based Microsoft Excel sheet. Statistical analysis was done by SPSS 20.0
Collected data were entered in computer based Microsoft Excel sheet. Statistical analysis was done by SPSS 20.0
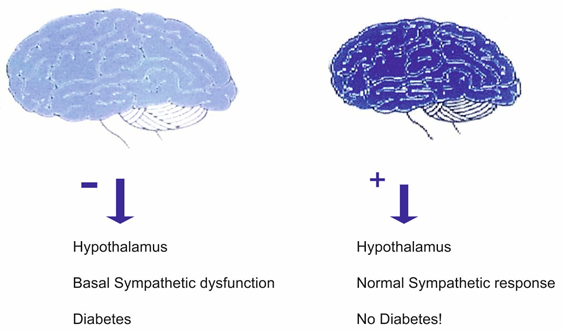
Figure 2: Faded appearance of brain- chronic exhaustion/stress Normal appearance of brain after Vipassana.
Discussion
Worldwide, the incidence of type-2 diabetes is on the rise. The role of chronic mental stress/exhaustion in diabetes remains unclear. A few studies have found association of chronic mental stress/mental exhaustion in diabetes patients. Changes in the blood glucose levels associated with transient stress are also reported [3-12]. Still data is lacking in using stress relaxation methods in management of diabetes. Therefore, this prospective study was planned to observe effect of various stress relaxation methods on glycemic control, lipid profile, EEG and basal sympathetic discharge; and a possible correlation among all these.
The study was done in Mittal hospital and Keshvam hospital Ajmer, India. 50 confirmed cases of type-2 diabetes were taken for the study. The study period was from January 2016 to December 2017. The cases were randomly divided into two groups; group 1 (control n = 30) and group 2 (study n = 20). The group 2 was further subdivided into 2 subgroups 2A (n = 10) and subgroup 2B (n = 10). Throughout the 12 weeks period, the patients were closely observed for symptoms and any discomfort.
The intervention was done in the form of various stress relaxation methods to all the groups and subgroups. Group 1 performed walking 45 minutes twice daily for 12 weeks. Group 2 was divided into 2 subgroups, subgroup 2A performed Pranayama, Asanas and Kriyas exercises and subgroup 2B performed purely mental relaxation exercise like Vipassana. Subgroup 2 an exercises, Pranayama aims at conservation and control of bioenergy by respiration and nervous control. Asanas and Kriyas consist mainly of postural exercises help in to conserve energy. In subgroup (2B) Vipassana gives rest to mind, a person is not supposed not to concentrate instead asked to allow the thoughts to float. Group 1 was asked to walk at a normal pace. Each group performed respective exercises for 45 minutes twice daily for 12 weeks.
Initially all groups and subgroups had comparable vital parameters and W: H ratio there was no statistical significant difference. (Group 1v/s/2A, 1v/s2B p > 0.05) (Table 1) After 12 weeks in W: H ratio there was statistical significant reduction in W: H ratio in sub group 2 B. (Group 1v/s/2A p > 0.05, 1v/s 2B p < 0.05). (Table 1) Initially stress scaling and mental health life style factors were suggestive of chronic stress and chronic mental exhaustion in all groups and subgroups. (Table 2)
In the present study all groups and subgroups had poor glycemic control and deranged lipid profile at the beginning. (Table 3, 4) Initial FBG/PPBG/ HbA1c there was no statistical significant difference among groups and subgroups (group 1v/s 2A, 1v/s 2B p > 0.05). (Table 3) After 12 weeks FBG/PPBG/ HbA1c there was statistical significant reduction in glycemic parameters in sub group 2 B. (group 1v/s 2A p>0.05, 1v/s 2B p < 0.001). (Table 3) Initial Tgl, LDL, HDL there was no statistical significant difference among groups and subgroups. (Group1v/s 2A, 1v/s 2B p > 0.05) (Table 4)
After 12 weeks there was statistical significant improvement in lipid profile parameters in sub group 2 B. There was reduction in Tgl and increase in HDL levels in sub group 2 B. (Group 1v/s 2A p > 0.05, 1v/s 2B p < 0.001) (Table 4)
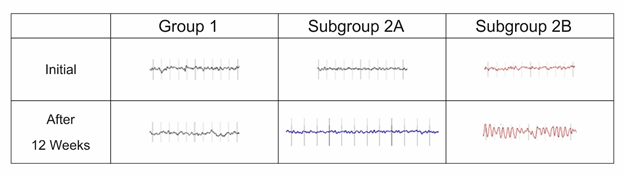
Initial EEG was suggestive of low voltage fast Beta activity in eye closure state in all groups and subgroups. This was suggestive of desynchronized activity found in stress and mental exhaustion.
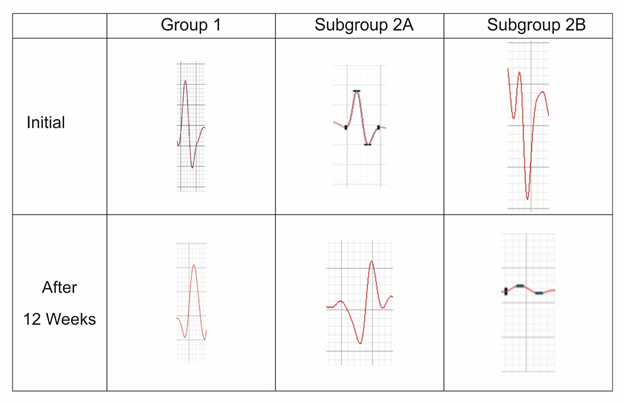
After 12 weeks EEG showed increase in amplitude/voltage and synchronization in sub group 2 B. (Table 5) Initial SSR was suggestive of spike activity (high basal discharge in all groups and subgroups)
After 12 weeks SSR showed reduction in spike voltage and a dome shaped response in sub group 2 B. (Table 6)
We summarize the findings
Initially all groups and subgroups were comparable, there was no statistical difference in W: H ratio, glycemic parameters (FBG, PPBG, HbA1c) lipid profile, EEG, SSR findings viz:
Initially all groups and subgroups were comparable, there was no statistical difference in W: H ratio, glycemic parameters (FBG, PPBG, HbA1c) lipid profile, EEG, SSR findings viz:
- Chronic stress
- Chronic mental exhaustion
- Desynchronized activity (fast Beta) in EEG
- Increased basal sympathetic discharge (spike in SSR)
- Deranged glycemic parameters
- Deranged lipid profile
After 12 weeks sub group 2 B who practiced Vipassana showed
- Synchronization (8-10 Hz alfa activity) and increase in amplitude/voltage in EEG
- Reduction in basal sympathetic discharge (dome in SSR)
- Reduction in W: H ratio
- Significant improvement in glycemic parameters
- Significant improvement in serum Tgl and HDL values
The findings clearly indicate that initially patients had chronic stress/exhaustion (suggested by PSS, questionnaire and EEG changes), increased basal sympathetic activity (suggested by SSR) and diabetes. After 12 weeks correction of these parameters in mental relaxation group (subgroup 2B) clearly indicates presence of central role in diabetes. Whereas no significant change occurred in sub group 2A i.e. those who performed abdominal/respiratory exercises.
How changes occurred- Possible mechanism
- Synchronization in EEG- Initial EEG had low voltage fast Beta activity in eye closure state was suggestive of desynchronized activity found in stress and mental exhaustion [3]. After Vipassana there was synchronized 8-10 Hz alfa activity in EEG in subgroup 2B. Vipassana (mental inactivity, observe silently what is happening) technique gives rest to mind/reduces stress, by not speaking, writing, reading, in a peaceful environment. By reducing mental activity improves physiologically depleted neuro- transmitters and reduces stress. Synchronization improves over all cortical control over lower centers, cortical-hypothalamic signals. [3, 27-30]
- Reduction in basal sympathetic discharge- Initially SSR was associated with spike response in all groups, along with normal resting pulse rate suggestive of high basal sympathetic activity. After 12 weeks in subgroup 2B there was reduction in basal sympathetic discharge. (Dome shaped response in SSR) This possibly results from improvement in signals to hypothalamus from various cortical areas (neo cortex, cingulate gyrus) [3,30,31]. Hypothalamus is the highest centre generating basal autonomic rhythm.
- Correction of W: H ratio – Reduction in basal sympathetic discharge reduces insulin resistance and therefore acquired obesity. [32]
- Improvement in glycemic parameters, lipid profile- (correction in insulin metabolism) Reduction in basal sympathetic discharge is responsible for reduction in insulin resistance and improvement in insulin release via inhibition of increased sympathetic discharge at alfa 1 and alfa 2 sympathetic receptors. Increased sympathetic activity is associated with insulin resistance in liver, muscles, tissues via stimulation of alfa 1 receptors and impaired insulin release via alfa 2 receptors in pancreas [3]. Reduction in basal sympathetic discharge normalizes activity of Na+/K+ (sodium/potassium) pump, shift of K+, insulin release, insulin sensitivity, and supports glucose entry into liver, muscle and tissues. [3, 33-35]
Conclusion
Chronic mental exhaustion (physiological depletion of neurotransmitters) and chronic stress are desynchronized state of brain, associated with increased basal sympathetic discharge. Increase in sympathetic discharge produces insulin resistance, impaired insulin release and diabetes. Vipassana/mental rest reduces expenditure of neurotransmitters, reduces the increased mental speed, reduces stress and helps in synchronization of brain. Therefore reduces basal sympathetic discharge and helps in control of diabetes. (Improvement in glycemic and lipid parameters) (figure 2)
Clinical implications
Prevention/treatment of diabetes Pandemic
The study gives 2 important messages:
Prevention/treatment of diabetes Pandemic
The study gives 2 important messages:
- Clear central role in etio-pathogenesis of diabetes
- Role of mental rest/reduction in stress is helpful in controlling diabetes. Vipassana is one method to reduce stress and exhaustion. Other methods which are helpful in day to day life can also be used.
1) Prevent chronic mental exhaustion (burn out)/stress
- Avoid excess use of laptop, mobile, computers and television.
- Spend less; avoid unnecessary speaking/reading/writing, to prevent depletion of neuro- transmitters, if you have already excess mental work.
- All efforts must start from school days, adequate balance between mental/physical activities.
- Take adequate mental rest daily/at week end/at month end.
- Listening light music
- Avoid hurriedness in completing work.
2) Replenish neurotransmitters
- Good sound sleep for around 7 hours to prevent/control diabetes. [36]
- Practice mental relaxation/ Vipassana
- Spending some time in garden to produce calmness in mind.
Acknowledgement: Arvind Sharma (EEG/SSR technician), Mrinalini Apurva (computer assistance)
Conflict of Interest: None
References
- K. Park. “In Park’s textbook of preventive and social medicine”. Diabetes Mellitus (2017): 411-413.
- Stress/definition of stress by medical dictionary. https://medical–dictionary. The free dictionary
- Saxena TK., et al. “Aetiopathogenesis of type-2 diabetes mellitus; could chronic stress play an important role?” The Journal of the Association of Physicians of India 62.6 (2014): 484-489.
- Harris ML., et al. “Stress increases the risk of type 2 diabetes onset in women: A 12- year longitudinal study using causal modeling”. PLos One 12.2 (2017): e0172126.
- Surwit RS., et al. “Stress and diabetes mellitus”. Diabetes care 15.10 (1992): 13-22.
- Kelly Sj and Ismail M. “Stress and type 2 diabetes: a review of how stress contributes to the development of type 2 diabetes”. Annual Review of Public Health 36 (2015): 441-462.
- Cathy Lloyd., et al. “Stress and Diabetes: A Review of the Link”. Diabetes spectrum 18.25 (2015): 121-127.
- Janice Wood. “Permanent stress linked to type 2 Diabetes in men”. (2013).
- Marcora SM., et al. “Mental fatigue impairs physical performance in humans”. Journal of Applied Physiology 106.3 (2009): 857-864.
- WR. Carter., et al. “Psychological Stressors Impact on Blood Glucose”. Diabetes Journal of diabetes association of America (1984): 71-72.
- Wood J. “permanent Stress Linked to Type 2 diabetes in Men”. Psych Central (2013).
- TS Danowski. “The evolution of diabetes from pre diabetes”. Postgraduate Medical Journal 46 (1970): 125-13015.
- The science of Yoga what research reveals.
- Lee S. Schwartz and Joseph A. Flaherty. A biosocios treatment.
- Vidya., et al. “A right Nostril Breathing Yoga Practice Brings about an Improvement in Patients with Type 2 Diabetes mellitus”. 46.1 (1998).
- Suresh C Jain., et al. “A study response pattern of non-insulin diabetes to yoga therapy”. Diabetes research and clinical practice 19.1 (1993): 69-74.
- Sahay BK., et al. “Effect of yogic practices on the exercise tolerance in diabetics”. Diabetes 40.1 (1991): 398.
- V Malhotra., et al. “Effects of yoga asanas and pranayama in non-insulin dependent diabetes mellitus.” Indian Journal of Traditional Knowledge 3.2 (2003): 162-167.
- Cohen S., et al. “A global of perceived stress”. Journal of health and social behavior 24.4 (1983): 386-396.
- Roberto Vetrugno., et al. “Sympathetic skin response”. Clinic autonomic Research 13 (2003): 256-270.
- Salvador M Guinjoan., et al. “Cardiovascular tests of autonomic function and sympathetic skin responses in patients with major depression”. Journal of Neurology, neurosurgery and psychiatry 59.3 (1995): 299-302.
- Glucose Trinder P. “Determination of glucose in Blood using Glucose Oxidase with an alternative Oxygen Acceptor”. Annals of Clinical Biochemistry 6 (1969): 24.
- Hoelzel W., et al. “IFCC reference system for measurement of hemoglobin A 1 c in human blood and the National Standardization schemes in the United states, japan and Sweden: a method comparison study.” Clinical chemistry 50.1 (2004): 166-174.
- Triglyceride Fossaati P and Prenciple L. “Serum Triglycerides Determined Calorimetrically with an Enzyme that Produces Hydrogen Peroxide”. Clinical Chemistry 28.10 (1982): 2077-2080.
- Ala Aldin Al-Hussaini., et al. “Vipassana meditation: A naturalistic, preliminary observation in Muscat”. Journal of Research in Medical Sciences 3.2 (2001): 87-92.
- Chiesa A. “Vipassana meditation: systematic review of current evidence”. Journal of Alternative and Complementary Medicine 16.1 (2010): 37-46.
- Wolfgang Klimesch. “EEG Alpha and theta oscillations reflect cognitive and memory performance: a review and analysis”. Brain Research Reviews 29.2.3 (1999): 169-195.
- Pfurtscheller G and Lopes da silva FH. “Event related EEG/MEG synchronization and de synchronization: basic principles”. Clinical Neurophysiology 110.11 (1999): 1842-1857.
- Stress and EEG. WWW.intechopen-com/download/pdf/1098
- Saxena T. “Possible clinical Implications of High Left Ventricular Ejection Force and exaggerated Sympathetic Skin Response in Hypertensive patients”. Annals of Clinical and Experimental Hypertension 4.1 (2016): 1035.
- Saxena T., et al. “Assessment of left ventricular ejection force and sympathetic skin response in normotensive and hypertensive subject: A double observation comparative case-control study”. Indian Heart Journal 68.5 (2015): 685-692.
- Tarun Saxena., et al. “Constitutional obesity v/s acquired obesity and their cardiovascular risk. Tarun S, Azeema o, Manjari S. constitutional obesity v/s acquired obesity and their cardiovascular risks.” Advancements in Cardiovascular Research 1.2 (2018): 000107.
- Westfall TC and Westfall DP. Neurotransmission: the autonomic and somatic motor nervous system. In: Goodman and Gilman’s. The pharmacological basis of therapeutics (2011): 1239-1243.
- McCarty MF. “Elevated sympathetic activity may promote insulin resistance syndrome by activating alpha- 1 adrenergic receptors on adipocytes”. Medical Hypotheses 62.5 (2004): 830-832.
- Tarun Saxena., et al. “Development of Diabetes: Possible Role of potassium”. International Journal of Diabetes & its Complications 1.3 (2017): 6.
- S Ramnathan Iyer. “Sleep and Type 2 Diabetes Mellitus-Clinical Implications.” Journal of the Association of Physicians of India 60 (2012): 42-47.
Citation:
Tarun Saxena., et al. “Effect of Various Stress Relaxation Exercises on Electroencephalography, Sympathetic Skin Response
and Type-2 Diabetes Mellitus”. Archives of Endocrinology and Diabetes Care 2.1 (2018): 164-175.
Copyright: © 2018 Tarun Saxena., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.