Review Article
Volume 1 Issue 3 - 2017
Choosing a Classification System for the Management of Patients with Diabetic Foot Problems
1,2,3,4Department of Orthopaedic Surgery, National University Health System, Singapore
*Corresponding Author: Associate Professor Aziz Nather, Senior Consultant, University Orthopaedics, Hand & Reconstructive Microsurgery Cluster, National University Health System, Singapore.
Received: January 09, 2017; Published: January 11, 2017
Abstract
A good classification system must take into account all three elements of the diabetic foot triad–vasculopathy, neuropathy and immunopathy. It will also serve as a guide to the treatment needed for each patient. In managing diabetic foot problems, one must adopt a classification system to provide better documentation and communication between members of the diabetic foot team.
For clinical purposes, the Wagner-Meggitt and the King’s Classification are useful to adopt because of their simplicity. They also provide a guide to the clinical outcome of patients and to the treatment needed. The Texas and the PEDIS Classification are more complicated and perhaps more suited for research purposes.
Keywords: Choice; Classification system; Management; Diabetic foot problems
Introduction
A good classification system takes into account the major risk factors involved in causing a diabetic foot problem–namely vasculopathy, neuropathy and immunopathy, elements of the diabetic foot triad [1]. A good classification is useful as a guide to the treatment needed for each patient.
It is important to adopt a classification system to provide better documentation and communication between members of the diabetic foot team.
Several classification systems have been used. These include: -
- Wagner-Megitt Classification [2,3]
- King’s Classification [4]
- University of Texas Classification [5]
- PEDIS Classification [6]
- Amit Jain’s Classification [7]
This paper discusses the advantages and disadvantages of each system that is commonly used. The objective of this paper is to guide healthcare professionals select a useful classification.
Wagner-Meggitt Wound Classification [2,3]
This classification (Table 1 and Figure 1) was first described by Meggitt in 1976 [2] and popularised by Wagner in 1981 [3]. It is a six-grade system that classifies ulcers according to the depth and extent of wound.
This classification (Table 1 and Figure 1) was first described by Meggitt in 1976 [2] and popularised by Wagner in 1981 [3]. It is a six-grade system that classifies ulcers according to the depth and extent of wound.
The advantages of the Wagner-Meggitt Wound Classification include its simplicity in usage. It also provides a guide for practitioners to plan treatment.
Its disadvantages include the fact that infection is only taken into account in Grade 3 and ischaemia in Grades 4 and 5 wounds. There is also controversy on the validation of this classification system [8,9].
| Grade | Description of ulcer |
| Grade 0 | Pre- or post-ulcerative lesion completely epithelialised |
| Grade 1 | Partial/full-thickness ulcer confined to the dermis, not extending to the subcutis |
| Grade 2 | Ulcer of the skin extending through the subcutis with exposed tendon or bone No abscess formation or osteomyelitis |
| Grade 3 | Deep ulcer with abscess formation or osteomyelitis |
| Grade 4 | Localised gangrene of the toes or partial foot gangrene |
| Grade 5 | Whole foot gangrene |
Table 1: Wagner-Meggitt Wound Classification.
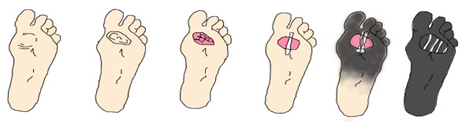
| Grade 0: No open lesion | Grade 1: Superficial ulcer | Grade 2: Deep ulcer | Grade 3: Deep Abscess/OM | Grade 4: Partial foot gangrene | Grade 5: Whole foot gangrene |
Figure 1: Wagner-Meggitt Wound Classification.
King’s College Classification [4]
The King’s College Classification (Table 2) is a simple staging system. It is based on the types of clinical presentation of the diabetic foot-ulcer, cellulitis, gangrene and amputation.
The King’s College Classification (Table 2) is a simple staging system. It is based on the types of clinical presentation of the diabetic foot-ulcer, cellulitis, gangrene and amputation.
The advantage of this system is that it is simple to use and is useful for planning the appropriate treatment for each stage.
Its disadvantage is that it has not been well-validated.
| Stage | Description |
| Stage 1 | Normal foot |
| Stage 2 | High risk foot |
| Stage 3 | Ulcerated foot |
| Stage 4 | Cellulitic foot |
| Stage 5 | Necrotic foot |
| Stage 6 | Major amputation |
Table 2: King’s College Classification.
Stage 1: Normal Foot
There is no risk factor in the normal foot (Figure 2). There is no neuropathy. Both foot pulses are palpable. There is no deformity, callosity or swelling.
There is no risk factor in the normal foot (Figure 2). There is no neuropathy. Both foot pulses are palpable. There is no deformity, callosity or swelling.
Stage 2: High-Risk Foot.
One or more risk factors for ulceration are present– namely sensory neuropathy or ischaemia (Figure 3). In the latter, one or both distal pulses are not palpable. There may be deformity, callosity, previous ulceration or previous amputation in the foot.
One or more risk factors for ulceration are present– namely sensory neuropathy or ischaemia (Figure 3). In the latter, one or both distal pulses are not palpable. There may be deformity, callosity, previous ulceration or previous amputation in the foot.
Stage 3: Ulcerated Foot
This stage (Figure 4) presents with skin breakdown or an ulcer. Ulceration usually occurs on the plantar surface in the neuropathic foot and on the dorsum of the foot in infection.
This stage (Figure 4) presents with skin breakdown or an ulcer. Ulceration usually occurs on the plantar surface in the neuropathic foot and on the dorsum of the foot in infection.
Stage 4: Cellulitic Foot
There is cellulitis with infection of the skin and subcutaneous tissue (Figure 5).
There is cellulitis with infection of the skin and subcutaneous tissue (Figure 5).
Stage 5: Necrotic Foot
This is characterised by the presence of necrosis or gangrene (Figure 6). Common sites of involvement are toes (one or more) and heel of the foot. They present as dry gangrene (no superimposed infection) or as wet gangrene (with superimposed infection).
This is characterised by the presence of necrosis or gangrene (Figure 6). Common sites of involvement are toes (one or more) and heel of the foot. They present as dry gangrene (no superimposed infection) or as wet gangrene (with superimposed infection).
Stage 6: Major Amputation
Major amputation (Figure 7) is defined as one taking place above the ankle joint–namely below knee, through knee and above knee amputation. Causes of below knee amputation include agonising pain in the foot, overwhelming infection in the foot and extreme necrosis or gangrene involving the foot.
Major amputation (Figure 7) is defined as one taking place above the ankle joint–namely below knee, through knee and above knee amputation. Causes of below knee amputation include agonising pain in the foot, overwhelming infection in the foot and extreme necrosis or gangrene involving the foot.
University of Texas Wound Classification [5]
The University of Texas (UT) Wound Classification (Table 3) evaluates the wound for depth, infection, and ischaemia. Wounds are first graded as 0, 1, 2, or 3 according to the depth of the wound. It is further categorised in four stages (A to D) according to the presence of infection and ischaemia.
The University of Texas (UT) Wound Classification (Table 3) evaluates the wound for depth, infection, and ischaemia. Wounds are first graded as 0, 1, 2, or 3 according to the depth of the wound. It is further categorised in four stages (A to D) according to the presence of infection and ischaemia.
| Grade | |||||
| Stage | 0 | 1 | 2 | 3 | |
| A | Pre- or post-ulcerative lesion completely epithelialised | Superficial wound not involving tendon, capsule or bone | Wound penetrating to tendon or capsule | Wound penetrating to bone or joint | |
| B | With infection | With infection | With infection | With infection | |
| C | With ischaemia | With ischaemia | With ischaemia | With ischaemia | |
| D | With infection and ischaemia | With infection and ischaemia | With infection and ischaemia | With infection and ischaemia | |
Table 3: University of Texas Wound Classification.
The UT system has been well validated. Armstrong., et al. [10] found patients whose wounds probed to bone to be 11 times more likely to receive a mid-foot or higher level amputation. Patients with infection and ischaemic were approximately 90 times more likely to receive a mid-foot or more proximal amputation.
Its disadvantage is that it is complex and difficult to use in clinical practice. It is perhaps better suited for research. Another disadvantage is that it does not take into account the presence or absence of neuropathy.
PEDIS Classification [6]
| Perfusion | |
| Grade 1 Grade 2 Grade 3 |
No symptoms of peripheral arterial disease (PAD) Symptoms or signs of PAD, but not critical limb ischaemia (CLI) Evidence of CLI |
| Extent/size | |
| Wound size in cm2 | |
| Depth/tissue loss | |
| Grade 1 Grade 2 Grade 3 |
Superficial, full-thickness ulcer Deep ulcer, penetrating to subcutaneous structures, involving fascia, muscle or tendon Bone or joint exposed |
| Infection | |
| Grade 1 Grade 2 Grade 3 Grade 4 |
No symptoms or signs of infection Infection involving skin and subcutaneous tissue only Erythema > 2 cm Infection involving deeper structures eg. abscess, osteomyelitis, septic arthritis or fasciitis Foot infection with signs of systemic response |
| Sensation | |
| Grade 1 Grade 2 |
No loss of protective sensation Loss of protective sensation |
Table 4: PEDIS Classification.
The PEDIS Classification (Table 4) was developed by the International Working Group of the Diabetic Foot (IWGDF) in 2003 for clinical research purposes [6]. It includes five categories: Perfusion, Extent/size, Depth/tissue loss, Infection and Sensation. Within each category, wounds are graded based on severity using objective techniques described in The International Consensus on the Diabetic Foot.
Developed for research purposes, the system is highly complicated to use. The PEDIS system relies on up-to-date investigations for classification, including ankle-brachial index (ABI), toe-brachial index (TBI) and transcutaneous oxygen pressure (TcPO2).
The Infectious Disease Society of America (IDSA) Guidelines have used the PEDIS system to recommend treatment according to the severity of the infection [11]. For Infection, Grade 1 does not usually require antibiotics. Grades 2 and 3 with less severe infections can be continued with oral antibiotics. Grade 4 with severe infection and critical limb ischaemia usually require hospitalization and intravenous antibiotics.
Amit Jain’s Classification [7]
A new classification for classifying diabetic foot complication has been described in 2012 (6).
A new classification for classifying diabetic foot complication has been described in 2012 (6).
| No. | Type of diabetic foot complications | Lesions |
| 1 | Type 1 (caused by infection) | Cellulitis, wet gangrene, abscess, necrotising fasciitis, osteomyelitis etc |
| 2 | Type 2 (not caused by infection) | Non-healing ulcers, peripheral arterial disease, hammer toes, entrapment neuropathies, diabetic neuro-osteoarthropathy etc |
| 3 | Type 3 (mixed) | Example: non-healing ulcer with osteomyelitis |
Table 5: Amit Jain’s Classification.
It is simple [12] and easy to understand. However, it is not predictive of clinical outcome and does not provide a guide to appropriate treatment and follow-up action. It has also not been validated.
Conclusion
A good classification system must take into account all three elements of the diabetic foot triad – vasculopathy, neuropathy and immunopathy. It is important to adopt a classification system to provide better documentation and communication between members of the diabetic foot team. For clinical purposes, the Wagner-Meggitt and the King’s Classification are useful to adopt because of their simplicity. They also provide a guide to the clinical outcome of patients and to the treatment needed. The Texas and the PEDIS Classification are more complicated and perhaps more suited for research purposes.
References
- Aziz Nather., et al. “Healing of Diabetic Foot Wounds – The Role of Basic Science and Underlying Pathology in Management of Diabetic Foot Wounds”. Orthopaedic Surgery and Tramuatology 1.2 (2016): 51–62.
- Meggitt B. “Surgical management of the diabetic foot”. British Journal of Hospital Medicine 16 (1976): 227-32.
- Wagner FW. “The vascular foot: a system for diagnosis and treatment”. Foot and Ankle 2.2 (1981): 64-122.
- Edmonds ME, Foster AVM. Managing the Diabetic Foot. Blackwell Science. 2000.
- Lavery LA., et al. “Classification of diabetic foot wounds: the University of Texas San Antonio diabetic wound classification system”. Ostomy Wound Management 43.2 (1977): 44-53.
- Schaper NC. “Diabetic foot ulcer classification system for research purposes: a progress report on criteria for including patients in research studies”. Diabetes/Metabolism Research and Reviews 20(S1) 2004: 590-595.
- Jain AKC. “A new classification of diabetic foot complication: a simple and effective teaching tool”. Journal of Diabetic Foot Complications 4.1 (2012): 1–5.
- Calhoun JH., et al. “Treatment of diabetic foot infections: Wagner classification, therapy, and outcome”. Foot and Ankle 9.3 (1988): 101-106.
- Oyibo SO., et al. “A comparison of two diabetic foot ulcer classification systems: the Wagner and the University of Texas wound classification systems”. Diabetes Care 24.1 (2001): 84-8.
- Armstrong DG., et al. “Validation of a diabetic wound classification system. The contribution of depth, infection, and ischaemia to risk of amputation”. Diabetes Care 21.5 (1998): 855-859.
- Lipsky BA., et al. “IDSA guidelines: Diagnosis and treatment of diabetic foot infections”. Clinical Infectious Diseases 39 (2004): 885-910.
- Dhubaib HA. “Understanding diabetic foot Complications: In praise of Amit Jain’s Classification”. The Diabetic Foot Journal Middle East 1.1 (2015): 10-11.
Citation:
Aziz Nather., et al. “Choosing a Classification System for the Management of Patients with Diabetic Foot Problems”. Orthopaedic
Surgery and Traumatology 1.3 (2017): 104-110.
Copyright: © 2017 Aziz Nather., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.









































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.