Research Article
Volume 1 Issue 4 - 2017
Ethibond Suturing of the Extensor Retinaculum as a New and Effective Alternative for Interfragmentary K-Wires in Fixation of Transverse Patellar Fractures with Tension Band Wiring
1Junior Resident, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
2Asso. Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
3Professor & Head, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
4Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
5Asst. Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
2Asso. Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
3Professor & Head, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
4Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
5Asst. Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of Medicine, Navi Mumbai
*Corresponding Author: Dr. Mishil S Parikh, Asst. Professor, Department of Orthopaedic Surgery, D Y Patil University’s School of
Medicine, Navi Mumbai.
Received: March 17, 2017; Published: May 09, 2017
Abstract
Purpose of the study: Modified tension band wiring has become the surgical method of choice today, for treating displaced transverse patellar fractures. However, the post-operative complications like symptomatic implants, infection, bursitis and implant failure are very common and additional procedures are often necessary to treat these complications. The purpose of this study is to evaluate the efficacy of a relatively metal-free technique using a non-absorbable suture material (Ethibond-5) instead of K-wires, to avoid the above complications.
Methods and Materials: A total of 29 patients of displaced transverse patellar fractures were selected for this study. A circumferential running stitch suturing of the extensor retinaculum with Ethibond number 5 for approximation of the fracture fragments along with an anterior figure-8 stainless steel wiring through the patellar and quadriceps tendons. All of them were treated with this technique. The clinical outcomes of these patients were evaluated using simple radiographs and on WEST’s criteria.
Results: Out of the 29 patients operated, none of them had a post-operative complication. This technique provided satisfactory clinical outcomes and very good knee function.
Conclusion: This technique provides good fixation, allows early motion exercises and in addition, prevents the post operative complications caused by the conventional interfragmentary K-wires.
Keywords: Patella Fracture; Ethibond Suturing; Tension Band; Novel Technique
Introduction
Patella is the largest sesamoid bone in the human body. It is a thick circular-triangular bone which articulates with the femur and covers and protects the anterior surface of the knee joint. It is also referred as kneecap because the patella acts like a shield for your knee joint, hence it can easily be broken. Falling directly onto your knee, for example, is a common cause of patellar fractures.
Patella fractures represent 1% of all skeletal injuries. The male-to-female ratio is (2:1) and the most common age group 20 to 50 years old. The modes of injury are direct (trauma), indirect (contraction of the quadriceps) or combined. [1,2]
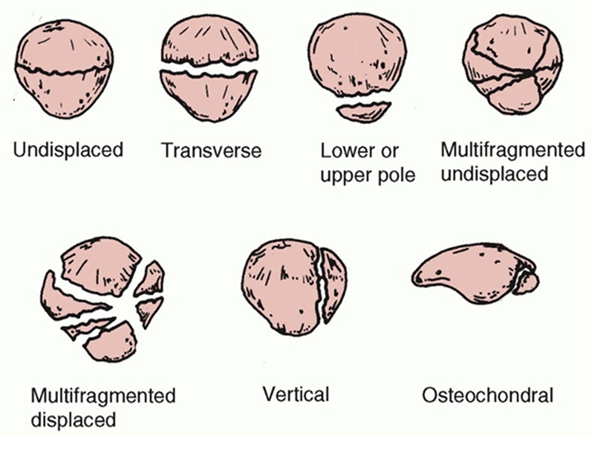
Patella fractures are classified on basis of the pattern of fracture as: stellate, comminuted, transverse, vertical (marginal), polar or osteochondral (Figure 1). Patellar fractures should be radiographically evaluated with anteroposterior, lateral, and axial (Merchant) views. Transverse fractures usually are best seen on a lateral view, whereas vertical fractures, osteochondral fractures, and articular incongruity are best evaluated on axial views. A comparison view of the opposite knee sometimes is necessary to differentiate an acute fracture from a bipartite patella, which is a failure of fusion of the superolateral portion of the patella and usually is bilateral.
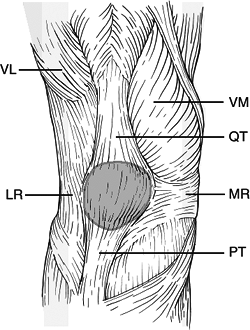
Although these fractures appear to be simple injuries, the soft tissue attachments to the patella have a great deal of bearing on the
final knee function. The medial and lateral extensor retinaculae are strong longitudinal expansions of the quadriceps and insert directly
onto the tibia (Figure 2). If these remain intact in the presence of a patella fracture, then active extension will be preserved.
Patellar fractures generally are associated with a hemarthrosis and localized tenderness. In fractures that are displaced or have concomitant retinacular tears, a palpable defect may be present. Inability of the patient to extend the affected knee actively usually indicates a disruption of the extensor mechanism and a torn retinaculum, which require surgical treatment. Occasionally, if active knee extension is limited by pain, the hemarthrosis can be aspirated under sterile conditions and followed by intra-articular injection of lidocaine. In patients without significant impairment of the extensor mechanism, active knee extension should be restored. An open wound in the vicinity of a patellar fracture may be a sign of a surgical emergency. [3]
Treatment options include non-operative and operative. Undisplaced or fractures with minimum articular disruption are subjected to non-operative treatment in the form of a cylindrical cast or knee immobilizer. Operative method includes open reduction and internal fixation. Indications for open reduction and internal fixation include > 2-mm articular incongruity, > 3-mm fragment displacement, or open fracture. [4]
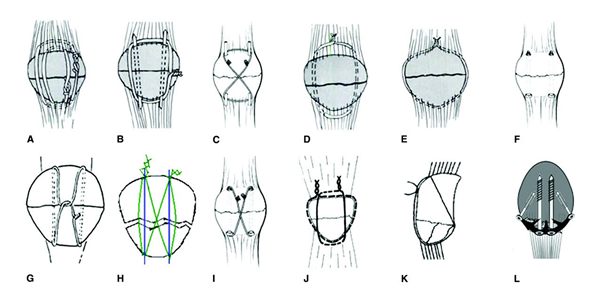
There are multiple methods of operative fixation, including tension banding (using parallel longitudinal Kirschner wires or cannulated screws) as well as circumferential cerclage wiring. (Figure 3) Retinacular disruption should be repaired at the time of surgery for good knee function after fracture union. [5]
Orthopaedic surgeons have been using various modifications of the existing ways of operative surgery to treat these fractures operatively. But there is no consensus on a particular modality. Hence there is no universally accepted technique of fixing a patella fracture. Modified tension band wiring has become the surgical method of choice today, for treating displaced transverse patellar fractures [6]. However, the post-operative complications like symptomatic implants, infection, bursitis and implant failure are very common and additional procedures are often necessary to treat these complications [6]. The purpose of this study is to evaluate the efficacy of a relatively metal-free technique using a non-absorbable suture material (Ethibond-5) instead of K-wires, to avoid the above complications.
Surgical Technique
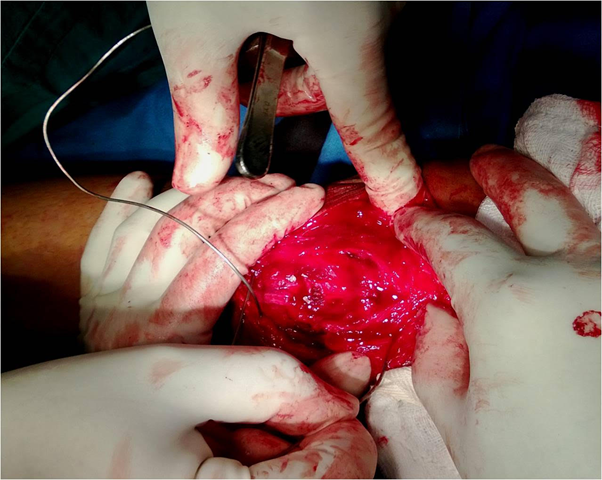
The conventional approach was used for the reduction of the fracture. We made a longitudinal midline approximately 2.5 cm longer from the superior and inferior poles of the patella. This gives enough exposure for reduction of the fracture and repair of the ruptured extensor expansion and synovium. The skin and subcutaneous tissue was reflected proximally and distally to expose the entire anterior surface of the patella and the quadriceps and patellar tendons. If the fracture fragments were significantly separated, it was presumed that there would be tears in the extensor expansion and these must be carefully explored medially and laterally. All small and detached fragments of bone were removed and the interior of the joint and especially the patellofemoral groove for an osteochondral fracture. Thoroughly irrigate the interior of the joint inspected to remove blood clots and small particles of bone. The fracture fragments were anatomically reduced using large towel clips or appropriate bone-holding forceps (Figure 4). Inspect the articular surface after fixation to ensure that the reduction is anatomical.
The conventional approach was used for the reduction of the fracture. We made a longitudinal midline approximately 2.5 cm longer from the superior and inferior poles of the patella. This gives enough exposure for reduction of the fracture and repair of the ruptured extensor expansion and synovium. The skin and subcutaneous tissue was reflected proximally and distally to expose the entire anterior surface of the patella and the quadriceps and patellar tendons. If the fracture fragments were significantly separated, it was presumed that there would be tears in the extensor expansion and these must be carefully explored medially and laterally. All small and detached fragments of bone were removed and the interior of the joint and especially the patellofemoral groove for an osteochondral fracture. Thoroughly irrigate the interior of the joint inspected to remove blood clots and small particles of bone. The fracture fragments were anatomically reduced using large towel clips or appropriate bone-holding forceps (Figure 4). Inspect the articular surface after fixation to ensure that the reduction is anatomical.
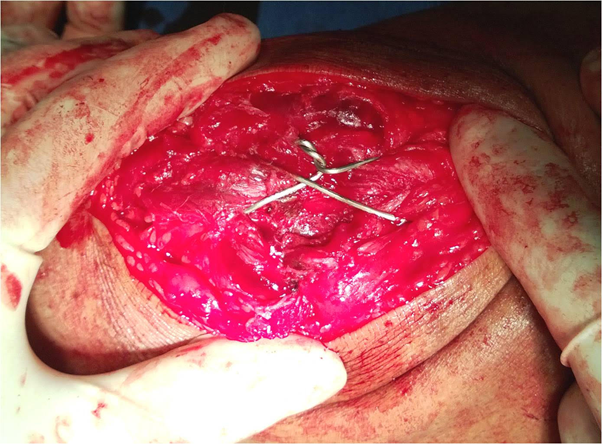
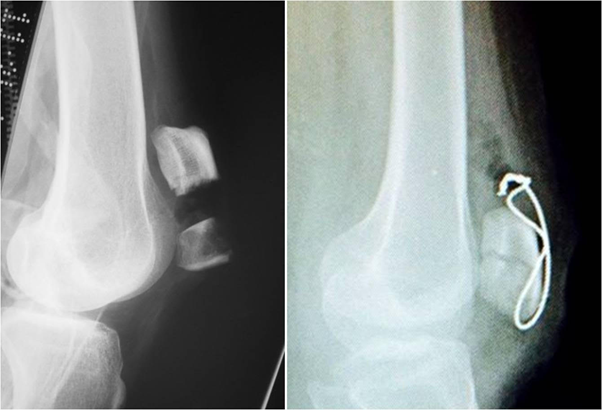
Now the extensor retinaculum was sutured with a No. 5 Ethibond from their outer ends toward the midline of the joint. (Figure 5). After the extensor mechanism was sutured, with fracture reduction held, Stainless Steel wire was passed anteriorly in a Figure of 8 fashion beneath the patellar and quadriceps tendons as done in a modified Tension Band Wiring. (Figure 6,7)
The only difference being that K-wires were not used to help maintain the fracture fragments in anatomical reduction. A thorough wash was given. The whole assembly and fracture reduction was checked under Image Intensifier (C-arm). Subcutaneous closure was done in a single layer with an absorbable suture material (Vicryl 2-0) and skin was closed with a non-absorbable suture material (Ethilon 2-0). A No.14 drain was put and kept for 24-48 hours.
After Treatment
Phase 1: (0-2 weeks) – Knee immobilizer, Range of Motion 0-30 degrees, assisted weight bearing, Static Quadricep & Dynamic Quadricep exercises. Drain is removed on the second post-operative day. Sutures are removed on the 14-15th post-operative day.
Phase 1: (0-2 weeks) – Knee immobilizer, Range of Motion 0-30 degrees, assisted weight bearing, Static Quadricep & Dynamic Quadricep exercises. Drain is removed on the second post-operative day. Sutures are removed on the 14-15th post-operative day.
Phase 2: (2-6 weeks) – Knee brace, ROM – add 15 degrees each week – Goal was to reach 90 degrees by end of 6th week, assisted weight bearing.
Phase 3: (6-10 weeks) – Unlocked knee brace worn only with weight bearing activities, full WB, full ROM.
Phase 4: (10-12 weeks) – Discontinue brace, start stationary bicycling.
Phase 5: (3-6 months) – Return to full activities as tolerated.
Material and Method
In this prospective study over a period of two years (from 2012 to 2014) twenty nine patients with displaced transverse patellar fractures were selected. All of them were closed injuries. Of these 29 patients, 23 were males (79.3%) and 6(20.7%) were females. The average age was 35.4 years (range 19-62). All of them were operated with this novel technique. The patients were put on the above mentioned post-operative mobilization protocol. These patients were followed up regularly. The first follow-up was on day 14, followed by monthly follow-ups for 3 months and then at the end of 6 months and 1 year after the surgery. Clinical and radiological evaluation was done on every visit. (Figure 8) The functional outcome was assessed by the WEST Criteria as Excellent, Good and Poor.
Results
Of the 29 patients operated for closed, displaced transverse patellar fractures, one patient had superficial infection which settled after intravenous antibiotics for 5 days. As per the WEST criteria, 26 patients (89.65%) had excellent function at the end of 3 months and 3 (10.34%) had a good outcome (Table 1). Of these 3, 2 had a loss of 15-20° of flexion while one had an extensor lag of 5°. There was no case of non-union. All the patients eventually returned to an active lifestyle.
| Resuts | No. of Cases | Percentage |
| Excellent | 26 | 89.66% |
| Good | 3 | 10.34% |
| Poor | 0 | 0% |
Table 1:
Discussion
Although these fractures appear to be simple injuries, it is at times difficult to get a good result after treatment of these fractures. The soft tissue attachments to the patella have a great deal of bearing on the final knee function. In addition to the quadriceps femoris tendon and femoral fascia attached to the superior pole of the patella and the patellar tendon at the inferior pole, the femoral fascia, vastus medialis muscle and vastus lateralis tendon form the patellar retinaculum to aid extension of the knee. The medial and lateral extensor retinaculae are strong longitudinal expansions of the quadriceps and insert directly onto the tibia. The patella works as a lever arm by separating the point of action of the knee extension system from the rotation centre to increase the extension efficiency [7].
Prior studies on patella fracture fixation have reported reoperation rates between 20% and 50% following use of Kirschner wires [8-10]. A recent study with 6.5 years mean follow-up by LeBrun reported a rate of 56% in a cohort similar to that used as a control in our study 27. Interestingly, all hardware removals in our study occurred in the K-wire group, accounting for 93% of all reoperations in the cohort; the remaining reoperations were indicated due to treatment failure.
The repair of the retinaculum, not only helps regain knee function sooner after the surgery but also helps in maintaining the reduction of the fractured fragments. In this way the use of metal can be minimized and hence the complications associated with it. It decreases the intraoperative surgical time also. Ethibond is a Polybutyrate coated braided polyester suture [11]. It is a non-absorbable suture with high tensile strength. It is generally inert, though some allergic reactions have been reported [12]. In our study we did not encounter any allergy to the suture material.
This study demonstrates that transverse patella fractures treated surgically compared similarly with regards to functional outcome, range of motion, and healing. It avoided complications associated with K-wires. The fractures treated with Ethibond suture technique did not necessitate removal of hardware unlike existing studies with K-wires which required another operation [13,14]. Suture fixation was also associated with a lower overall reoperation rate. Our results indicate that transverse patella fractures are successfully treated with heavy braided non-absorbable suture and SS wire fixation and achieve outcomes better than the conventional modified Tension Band Wiring and K-wire fixation.
Conclusion
This novel technique provides good stable fixation, allows early motion exercises and in addition, prevents the post operative complications caused by the conventional interfragmentary K-wires.
References
- Melvin JS and Mehta S. “Patella fractures in adults”. The Journal of the American Academy of Orthopaedic Surgeons19.4 (2011): 198-207.
- Bostrom A. “Fracture of the patella: a study of 422 patellar fractures”. Acta Orthopaedica Scandinavica 143 (1972): 1-80.
- Harris RM. Fractures of the patella and injuries to the extensor mechanism. In: Bucholz., et al. (eds) Rockwood and green’s fractures in adults. 6th ed, Lippincott and Williams & Wilkins, Philadelphia, (2006): 1969-1997.
- Carpenter JE., et al. “Biomechanical evaluation of current patella fracture fixation techniques”. Journal of Orthopaedic Trauma 11.5 (1997): 351-356.
- Galla M and Lobenhoffer P. “Patella fractures”. Chirurg 76.10 (2005): 987-997.
- Muller ME AM., et al. Springer: Berlin; 1979. Internal fixation: techniques recommended by the AO Group.
- Insall JN. New York: Churchill Livingstone; 1984. Surgery of the knee.
- Hung LK., et al. “Fractured patella: operative treatment using the tension band principle”. Injury16 (1985): 343-347.
- Lebrun CT., et al. “Functional outcomes after operatively treated patella fractures”. Journal of Orthopaedic Trauma 27.6 (2012): 422-426.
- Kastelec M and Veselko M. “Inferior patellar pole avulsion fractures: osteosynthesis compared with pole resection”. The Journal of Bone and Joint Surgery America87.1(pt 1) (2004): 696-701.
- Capperauld I. “Ethibond--a new polybutylate coated polyester suture”. Polimery w Medycynie 6.4 (1976): 167-171.
- Wüst DM., et al. “Mechanical and handling properties of braided polyblend polyethylene sutures in comparison to braided polyester and monofilament polydioxanone sutures”. Arthroscopy22.11 (2006): 1146-1153.
- Smith ST., et al. “Early complications in the operative treatment of patella fractures”. Journal of Orthopeadic and Trauma 11.3 (1997): 183-187.
- Gosal HS., et al. “Clinical experience of patellar fracture fixation using metal wire or nonabsorbable polyester-a study of 37 cases”. Injury 32.2 (2001): 129-135.
Citation:
Mishil S Parikh., et al. “Ethibond Suturing of the Extensor Retinaculum as a New and Effective Alternative for Interfragmentary
K-Wires in Fixation of Transverse Patellar Fractures with Tension Band Wiring”. Orthopaedic Surgery and Traumatology 1.4
(2017): 126-132.
Copyright: © 2017 Mishil S Parikh., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.





































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.