Research Article
Volume 1 Issue 5 - 2017
Preventable Errors and Mortality in Elderly Hip Fracture Patients
1Trauma and Orthopaedic Surgery, Musgrove Park Hospital, UK
2Care of the Elderly, Musgrove Park Hospital, UK
3Anaesthetics, Musgrove Park Hospital, UK
2Care of the Elderly, Musgrove Park Hospital, UK
3Anaesthetics, Musgrove Park Hospital, UK
*Corresponding Author: Stephanie Buchan, Department of Trauma and Orthopaedic Surgery, Musgrove Park Hospital, UK.
Received: September 29, 2017; Published: October 03, 2017
Abstract
Introduction : Hip fracture is associated with a high 30-day mortality in the elderly. All perioperative deaths should be reviewed using clinical morbidity and mortality (M&M) processes. The aim of this study was to compare MDT findings with orthopaedic M&M findings, and identify preventable errors and their contribution to mortality.
Materials and Methods: A consultant led MDT (orthopaedic surgeon, anaesthetist, orthogeriatricians, and trauma specialist nurse and junior representatives) conducted standardised case note reviews of all 30-day neck of femur mortalities between January and November 2014. These were compared with findings from orthopaedic M&M meetings. System failures and errors in surgical, medical and anaesthetic care were noted. Predicted mortality was calculated using the Nottingham Hip Fracture Score and the MDT concluded if death was preventable.
Results: 30 patients (7.6%) died within 30 days of admission. 32 errors in care were identified at the MDT meeting: 1 (3%) surgical error, 19 (59%) medical errors, 4 (13%) anaesthetic errors and 8 (25%) system failures. Of the 30 patients, 1 death was considered definitely preventable, 2 probably and 8 possibly preventable. The Orthopaedic M&M detected 5 errors in care.
Conclusion: MDT M&M review is more sensitive for detecting errors in care. Routine review of mortality and non-surgical morbidity by orthopaedic surgeons should be abandoned as unfit for purpose. Mortality is almost exclusively related to existing medical co-morbidity and perioperative care so orthogeriatric management should begin as soon as practical after admission and MDT mortality review should be the standard of care for all fractured neck of femur patients.
Keywords: Mortality; Morbidity; Perioperative; Hip; Fracture; Elderly
Abbreviations: ASA: American Society of Anaesthesiology; NHFD: National Hip Fracture Database; NHFS: Nottingham Hip Fracture Score; NOF: Neck of Femur; M&M: Morbidity and Mortality; MDT: Multidisciplinary Team
Introduction
Significant morbidity and mortality is associated with hip fractures [1]. 64,864 patients sustained a hip fracture in England, Wales and Northern Ireland in 2015 and the national average 30-day mortality was 7.1% [2]. The National Hip Fracture Database (NHFD) identified that males were older with greater co-morbidities than females who fractured their hip and the mortality rate in males was double that of females [3]. Comorbidities have a direct impact on the outcome for hip fracture patients and create a challenge for those caring for the patient, hence a multi-disciplinary team approach is essential to improve care [4]. Moreover, optimal perioperative medical management with strict rehabilitation may improve outcome and reduce cost [5].
Hip fracture patients older than 80 have an increased mortality compared with younger patients [6], and a significant number of hip fracture patients die in hospital from preventable errors [7]. No significant difference in 30-day mortality rate has been noted between patients younger or older than 80, but the main predictors of 30-day mortality in hip fracture patients younger or older than 80 are ASA grade and in-hospital complications respectively [6].
Hip fracture patients who undergo surgery within 12 hours of admission have a significantly lower 30-day mortality rate [8], and a delay in surgery beyond 48 hours significantly increases mortality rate [9]. National Institute for Health and Care Excellence (NICE) guidance states that hip fracture surgery should be performed within 36 hours of admission [10] and reversible comorbidities should be treated immediately to avoid delay in surgery [1].
The British Orthopaedic Association states that all deaths should be recorded and monitored at mortality and morbidity (M&M) meetings [11]. All surgeons must participate in regular M&M meetings and involve other clinicians who care for the patients [12]. Moreover, consultant anaesthetists felt joint speciality meetings were key to undertaking effective M&M reviews [13]. Tarrant., et al. described a multidisciplinary team (MDT) approach to analyse hip fracture mortality case notes and provide a detailed review of care errors [7]. However, there is no evidence to prove if this MDT approach provides a more comprehensive view than the more common practice of departmental M&M meetings.
The aims of this study were:
- Compare the findings of orthopaedic M&M meetings with an MDT approach
- Identify any preventable errors contributing to mortality.
Materials and Methods
The study took place at Musgrove Park Hospital, a level 2 trauma centre with an orthogeriatric service. An MDT was designed to conduct standardised case reviews for patients who died within 30 days of admission following a neck of femur (NOF) fracture between 1st January 2014 and 30th November 2014. The MDT included a consultant orthopaedic surgeon, a consultant anaesthetist, consultant orthogeriatricians, a trauma specialist nurse, and junior doctor representatives.
The predicted 30-day mortality was calculated using the Nottingham Hip Fracture Score (NHFS). Key points of the standardised case note review highlighted errors in care, specifically system or communication errors, documentation, surgical technique, judgement in medical management and anaesthetic during the patient’s in-hospital stay. Time and type of surgery, type of anaesthetic, reason for any delay in surgery and cause of death were also noted.
Following thorough consideration the MDT concluded whether the death was unpreventable, possibly preventable, probably preventable or definitely preventable. The outcome from both MDT and orthopaedic M&M meetings were then compared to identify if the MDT approach provided a more comprehensive analysis of care concerns, providing key learning points from each case.
Results
30 of 395 patients (7.6%) admitted with NOF fractures died within 30 days of admission between 1st January 2014 and 30th November 2014. 18 (60%) underwent hemiarthroplasty, 11 (37%) had a dynamic hip screw and 1 (3%) died before surgery. The NHFS ranged from 4.4% to 34%; with the majority scoring 6.9-24%. 17 (57%) were male and 13 (43%) were female, and the mean age was 88 years (66-102). ASA grade ranged from 2-5, with 60% of patients scoring an ASA grade of 3.
In keeping with national studies [2, 14], anaesthetic type varied: 12 (41%) had a general anaesthetic, 10 (35%) had a spinal anaesthetic, 4 (14%) had a general anaesthetic and block and 3 (10%) had combined general and spinal anaesthetic. 10 (35%) of patients who underwent surgery had a significant delay in admission to theatre time (>36 hours) because they were not deemed medically fit.
Most patients who died within 30 days of admission with NOF fractures had bronchopneumonia or cardiovascular disease as the documented cause of death (see figure 1). Two patients who died in a nursing home following discharge were certified with dementia as their main cause of death.
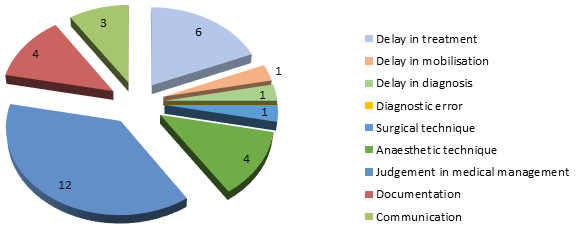
Orthopaedic M&M meetings identified 5 errors (3 errors of judgement in medical management, 1 documentation error and 1 communication error). 32 errors were noted at the NOF mortality MDT meeting (see figure 2). The most frequent error was judgement in medical management, accounting for 37.5% of care errors. Surgical errors accounted for 1 (3%) error, 19 (59%) were medical errors, 4 (13%) were anaesthetic errors and 8 (25%) errors occurred due to system failure (delay in mobilisation, error in documentation or error in communication).
Of the 30 deaths, 11 (37%) were considered preventable at the MDT meeting: 8 possibly, 2 probably and 1 definitely preventable according to the classification of Tarrant., et al. [7]; all MDT members agreed about the classification of all cases. A major error in medical management contributed to one death considered definitely preventable, whereby a patient who had myasthenia gravis was administered gentamicin which is contra-indicated; this error was also identified at the orthopaedic M&M meeting. Two deaths were probably preventable: 1 was due to an error in the type of anaesthetic, doses of drugs administered and treatment of hypotension intra-operatively; the other was due to a significant error in fluid management post-operatively. Factors contributing to the 8 possibly preventable deaths included 3 documentation errors, 1 delay in treatment, 7 errors of judgement in medical management, 2 errors in anaesthetic technique and 1 delay in diagnosis.
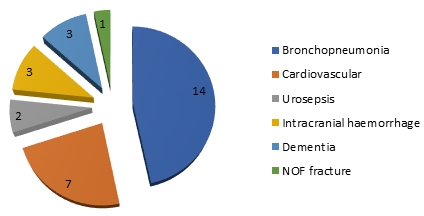
Figure 1: Principal cause of death for the 30 patients who died within 30 days of admission with NOF fracture.
Discussion
30-day mortality rates have fallen significantly since 2006, despite a rise in admission rates for patients with a hip fracture [15]. We found a 30-day mortality of 7.6% for hip fracture patients between 1st January 2014 and 30th November 2014, which is comparable to the national average 30-day mortality of 7.5% in 2014 and 7.1% in 2015 [2]. It is evident that there is still need for research and education to further improve mortality rates for patients who sustain a hip fracture.
The NHFS is useful for predicting 30-day mortality of patients with a hip fracture and NHFS of ≥6 (11.0% predicted mortality) indicates high risk [16,17]; 24 (80%) of patients in this study scored ≥ 11% so would be considered high risk. This study supported the findings by Chatterton., et al. [15] and Tarrant., et al. [7] that the leading causes of death for patients admitted with a hip fracture are bronchopneumonia and cardiovascular disease. We recommend mortality risk stratification on admission so high risk patients receive early senior orthogeriatric and anaesthetic input.
Just over one third of patient deaths occurring within 30 days of admission following a hip fracture were considered at least possibly preventable at our MDT meeting. A wide range of errors were highlighted in this study, with the majority being errors in judgement within the MDT caring for the patient in the perioperative period. The findings have launched several service improvements and by adopting a transparent no blame culture we can learn from errors in a constructive manner with the aim of reducing 30-day mortality following hip fracture. Significantly more errors were identified by the MDT than the orthopaedic M&M meeting in this study, indicating that orthopaedic surgeons are poor at detecting errors in medical and anaesthetic care and the MDT approach is a more sensitive format for reviewing hip fracture patient deaths within 30 days of admission. We have therefore abandoned the orthopaedic M&M review meeting in favour of the MDT approach for hip fracture patients, despite the greater time commitment this requires from clinicians [18].
The Royal College of Physicians suggests that hip fracture is a model marker condition for investigating and challenging care outcomes and quality provided to frail older patients in the NHS today [14]. Hip fracture is the most studied, but the challenges of perioperative management of frail older patients apply across other patterns of trauma and emergency surgical admissions. MDT mortality review is therefore likely to benefit frail older patients admitted under the care of other surgical specialties.
Limitations of this study include the small number of patients, that it was undertaken at 1 hospital and covered a relatively short time-frame. To allow a more comprehensive analysis of the 2 formats of meeting a multi-centre study with monitoring over several years would be required. Regardless, the findings of this study do not come as a surprise and show such a significant difference that it would be reasonable to widely adopt this MDT approach to optimise patient care based on the data we have presented.
Conclusion
MDT M&M review is more sensitive for detecting errors in care. Routine review of mortality and non-surgical morbidity by orthopaedic surgeons should be abandoned as unfit for purpose. Mortality is almost exclusively related to existing medical co-morbidity and perioperative care so orthogeriatric management should begin as soon as practical after admission and MDT mortality review should be the standard of care for all fractured neck of femur patients.
Conflict of interest
No conflict of interest exists.
No conflict of interest exists.
References
- National Institute for Health and Clinical Excellence (NICE). Hip Fracture: Management (2011) [Online]. [Accessed 26 Nov 2015].
- Royal College of Physicians. National Hip Fracture Database (NHFD) Annual Report 2016. London: HQIP (2016). [Online]. [Accessed 18 Sept 2016].
- Sterling, R. “Gender and Race/Ethnicity Differences in Hip Fracture Incidence, Morbidity, Mortality and Function”. Clinical Orthopaedics and Related Research469.7 (2011): 1913-1918.
- Boddaert JB., et al. “Perioperative Management of Elderly Patients with Hip Fracture”. Anaesthesiology 121 (2014): 1336-1341.
- Sharrock NE. “Fractured Femur in the Elderly: Intensive Perioperative Care is Warranted”. British Journal of Anaesthesia 84.2 (2000): 139-140.
- Mariconda M., et al.“The Determinants of Mortality and Morbidity During the Year Following Fracture of the Hip”.Bone Joint Journal97-B (2015): 383-390.
- Tarrant SM., et al. “Preventable Mortality in Geriatric Hip Fracture Inpatients”. Bone Joint Journal 96-B (2014): 1178-184.
- Bretherton CP and Parker MJ. “Early Surgery for Patients with a Fracture of the Hip Decreases 30-Day Mortality”. Bone Joint Journal 97-B (2015): 104-108.
- Moja, L., et al. “Timing Matters in Hip Fracture Surgery: Patients Operated within 48 hours Have Better Outcomes. A Meta-Analysis and Meta-Regression of over 190,000 Patients”. PLoS One 7.10 (2012): e46175.
- National Institute for Health and Clinical Excellence (NICE). Commissioning Guide: Management of Hip Fracture in Adults (2012).
- Helping Consultants get things right. The BOA Advisory Book. Editor J Dias. London: The Professional Practice Committee. The British Orthopaedic Association (2014).
- The Royal College of Surgeons of England. Morbidity and Mortality Meetings: A Guide to Good Practice. London: The Royal College of Surgeons of England (2015).
- Royal College of Anaesthetists. National Audits: Report Version 16. London: RCoA (2003).
- Royal College of Physicians. National Hip Fracture Database (NHFD) Annual Report 2015. London: HQIP (2015).
- Chatterton BD., et al. “Cause of Death and Factors Associated with Early In-Hospital Mortality After Hip Fracture”. Bone Joint Journal97-B (2015): 246-251.
- Rushton PRP., et al. “Independent validation of the Nottingham Hip Fracture Score and Identification of Regional Variation in Patient Risk within England”. Bone Joint Journal 96-B (2015): 100-103.
- Moppett IK., et al. “Nottingham Hip Fracture Score: longitudinal and multi-centre assessment”. British Journal of Anaesthesia 109.4 (2012): 546-550.
- Kobewka DM., et al. “Quality gaps identified through mortality review”. BMJ Quality and Safety 26.2 (2017): 141-149.
Citation:
Stephanie Buchan., et al. “Preventable Errors and Mortality in Elderly Hip Fracture Patients”. Orthopaedic Surgery and
Traumatology 1.5 (2017): 197-202.
Copyright: © 2017 Stephanie Buchan., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.