Research Article
Volume 1 Issue 1 - 2016
Team Approach in the management of Diabetic Foot Wounds- the National University Hospital Experience
1,2,4,5,6Division of Foot and Ankle, University Orthopaedics, Hand and Reconstructive Microsurgery Cluster, National University Health System, Singapore
3Department of Biostatistics, Yong Loo Lin School of Medicine, National Singapore of Singapore, Singapore
3Department of Biostatistics, Yong Loo Lin School of Medicine, National Singapore of Singapore, Singapore
*Corresponding Author: Aziz Nather, Senior Consultant, Division of Foot and Ankle, University Orthopaedics, Hand and Reconstructive Microsurgery Cluster, National University Health System, Singapore.
Received: August 15, 2016; Published: August 30, 2016
Abstract
In NUH, an interdisciplinary diabetic foot team combined with a clinical pathway was formed in May 2003 to manage patients with diabetic foot wounds. The objective of this paper is to evaluate the effectiveness of this team in managing diabetic foot problems.
2 cohorts of patients were studied. The first cohort consisted 61 patients admitted from January to December 2002 (pre-team formation). The second cohort consisted of 206 patients admitted from January 2014 to December 2014.
The parameters studied to compare the results of pre-team and post team (in 2014) included Length of Stay, Major Amputation Rate, Re-admission Rate and Complication Rate.
Statistical analysis was performed using the Mann-Whitney U Test and chi-square test. Mann-Whitney U Test was used to compare length of stay between 2002 and 2014, while the chi-square test was used to compare the amputation rate, readmission rate, and complication rate. Multiple comparisons with Bonferroni adjustment were utilized to compare year 2002 and 2014.
NUH Team Approach coupled with a clinical pathway showed significant reduction in the length of stay, major amputation rate and readmission rate compared to the results seen before the team was formed. However, it did not show any difference in complication rate.
Keywords: Team Approach; Management of Diabetic Foot Wounds; Length of Stay; Major Amputation Rate; Re-admission Rate
Abbreviations: NIL
Introduction
Diabetes is a national problem in Singapore. Singapore has an estimated 400,000 diabetics in 2014 [1]. It is currently the 2nd highest cause of ill-health and mortality, next to Ischemic Heart Disease [1]. Singapore is currently the nation with the 2nd highest incidence of diabetes amongst all the developed countries, second to the United States of America [2].
NUH adopts a 2-prong strategy to manage the Diabetic Foot Wounds. The 1st strategy is prevention, by way of education and annual foot screening for all diabetics. However, once prevention fails and a foot complication develops, the latter is best treated by an Interdisciplinary Diabetic Foot Team.
NUH formed an Interdisciplinary Diabetic Foot Team (DFT) in May 2003 [3]. The Team Approach is implemented with a clinical pathway. The effectiveness of this team, coupled with the implemented pathway was evaluated in 2010. The team approach was found to be effective in reducing Length of Stay, Major Amputation Rate, as well as complication rate of our patients. We continued to manage patients with diabetic foot complications using the team system, coupled with the clinical pathway. The objective of this paper is to evaluate the effectiveness of the team approach some 12 years later.
Materials and Methods
Study Populations
2 cohorts of patients were studied, the first cohort consisting of 61 patients admitted to the team from January to December 2002 (Pre-Team formation). The second cohort consisted of 206 patients admitted to the team from January to December 2014.
2 cohorts of patients were studied, the first cohort consisting of 61 patients admitted to the team from January to December 2002 (Pre-Team formation). The second cohort consisted of 206 patients admitted to the team from January to December 2014.
Methodology
Medical records of all patients in the 2 cohorts were retrieved. Parameters studied included patient profile (age, gender, HbA1c). Other parameters studied included:
Medical records of all patients in the 2 cohorts were retrieved. Parameters studied included patient profile (age, gender, HbA1c). Other parameters studied included:
- Type of diabetic foot problems
- Length of stay
- Major amputation (defined as amputation above the ankle) rate
- Re-admission rate
- Complication rate
Statistical Analysis
Mann-Whitney U Test was used to compare length of stay between 2002 and 2014, while the chi-square test was used to compare the amputation rate, readmission rate, and complication rate. Multiple comparisons with Bonferroni adjustment were utilized to compare year 2002 and 2014.
Mann-Whitney U Test was used to compare length of stay between 2002 and 2014, while the chi-square test was used to compare the amputation rate, readmission rate, and complication rate. Multiple comparisons with Bonferroni adjustment were utilized to compare year 2002 and 2014.
NUH Diabetic Foot Team
NUH formed an interdisciplinary diabetic foot team in May 2003, consisting of an orthopaedic surgeon, an endocrinologist, a vascular surgeon, an infectious disease consultant, a podiatrist and a wound care nurse [3]. Patients admitted to the team, were treated following the diabetic foot clinical pathway implemented. All patients were classified using King’s College Classification [4]. The pathway included documentation of detailed medical history, meticulous clinical examination, including assessment of all 3 components of Diabetic Foot Triad- Neuropathy, Vasculopathy and Immunopathy [3].
NUH formed an interdisciplinary diabetic foot team in May 2003, consisting of an orthopaedic surgeon, an endocrinologist, a vascular surgeon, an infectious disease consultant, a podiatrist and a wound care nurse [3]. Patients admitted to the team, were treated following the diabetic foot clinical pathway implemented. All patients were classified using King’s College Classification [4]. The pathway included documentation of detailed medical history, meticulous clinical examination, including assessment of all 3 components of Diabetic Foot Triad- Neuropathy, Vasculopathy and Immunopathy [3].
Investigations performed included full blood count; erythrocyte sedimentation rate; C-reactive protein; urea, and electrolytes; HbA1c; capillary blood glucose; blood culture and wound culture. Referral was made to relevant members of the team, including the podiatrist, vascular surgeon, and infectious disease consultant [3]. The team performed weekly ward rounds to discuss management, including endocrine control, antibiotic treatment, choice of wound dressing to be used and the need for surgery. Before discharge, education on diabetes, foot care and footwear will be provided. Patient and caregivers were taught to do their own dressings.
During each team ward round, all cases discussed are seen by all members of the team and important clinical decision on management of the patient are made with input from all specialists in the team – endocrine, infectious disease, podiatry, nursing and vascular surgery. Joint decision is made on need for surgery, choice of antibiotics, choice of dressing etc.
Results and Discussion
Patient Demographics
| 2002 | 2014 | P value | |
| Mean Age | 60.77 | 61.79 | 0.991 |
| Mean HbA1c | 9.545 | 9.607 | 0.758 |
| Gender Composition | 33 males, 28 females | 121 males, 85 females | 0.415 |
Table 1: Patient Demographics.
Statistical evaluation of the Demographic composition of the two cohorts in 2002 and 2014 in terms of mean age, gender composition and HbA1c showed no significant difference. Valid comparison could be performed between the two groups.
Length of Stay
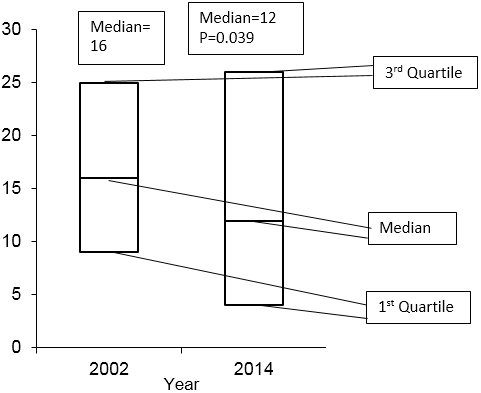
Figure 1 shows the 1st Quartile, Median and 3rd Quartile of Length of Stay (LOS).
Figure 1 shows the 1st Quartile, Median and 3rd Quartile of Length of Stay (LOS).
Distribution of length of stay (in days)
LOS in terms of days was 12 days in 2014, significantly lower (p=0.039 after Bonferroni Correction) compared to 16 days in 2002.
Amputation Rate
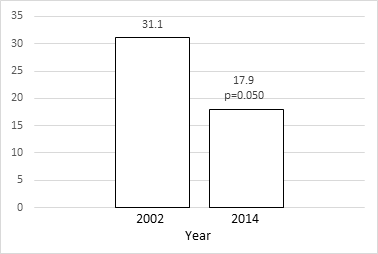
Figure 2 shows the Major Amputation Rates
Figure 2 shows the Major Amputation Rates
Amputation rate/%
The major amputation rate in 2014 was 17.9%, significantly lower than the rate in 2002 of 31.1% (p=0.050 after Bonferroni correction).
Re-admission Rate
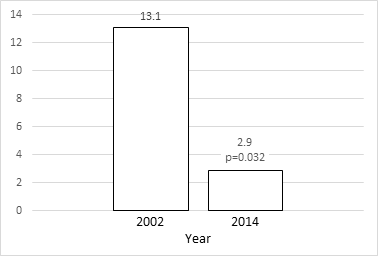
Figure 3 shows the Re-admission Rates.
Figure 3 shows the Re-admission Rates.
Readmission rate/%
The re-admission rate was 2.9% in 2014, significantly lower than that in 2002, of 13.1% (p= 0.032 after Bonferroni correction).
Complication Rate
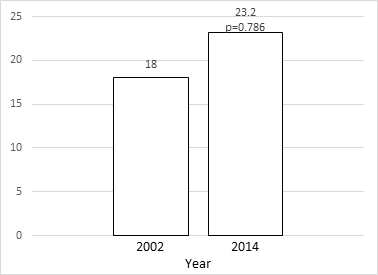
Figure 4 shows the Complication Rates.
Figure 4 shows the Complication Rates.
Complication rate/%
However, the complication rate in 2014 was 23.2%, higher than the complication rate in 2002 of 18%. This difference was not statistically significant (p = 0.786 after Bonferroni correction).
Discussion
Evaluation of the NUH team approach with its coupled clinical pathway performed in 2010 showed the average LOS to be significantly reduced (12.20 days post team to 20.36 days pre-team, p = 0.0005). The major amputation rate was significantly reduced (11.01% post team to 31.15% pre-team, p < 0.0005). The mean hospitalization cost per patient was not significantly different after the team formation ($8383.79 post team to $8847.17 pre-team). The complication rate was significantly lower (7.34% post team to 19.67% pre-team, p = 0.005). The readmission rate was not significantly reduced (8.26% post team to 13.11% pre-team, p = 0.510) [3]. This paper evaluated the effect of the same team on a cohort in 2014, 12 years after the team formation.
Length of Stay
Lavery,. et al. reported a significant reduction in length of stay from 4.75 to 3.72 days (p < 0.05) [5]. Gibbons et al also showed reduction in overall length of stay from 38.5 to 21.9 days (p < 0.001) [6]. In contrast, Martinez et al did not report any significant reduction in the Average LOS [7]. However, our team approach coupled with the clinical pathway, did show a significant reduction in the median length of stay (16 days pre-team to 12 days post team, p = 0.039).
Lavery,. et al. reported a significant reduction in length of stay from 4.75 to 3.72 days (p < 0.05) [5]. Gibbons et al also showed reduction in overall length of stay from 38.5 to 21.9 days (p < 0.001) [6]. In contrast, Martinez et al did not report any significant reduction in the Average LOS [7]. However, our team approach coupled with the clinical pathway, did show a significant reduction in the median length of stay (16 days pre-team to 12 days post team, p = 0.039).
Major Amputation Rate
Several studies showed significant reduction in the major amputation (amputation above the ankle) rate, as the most beneficial outcome of the team approach [7,8,9]. Krishnan., et al. reported a significant reduction of 82% in major amputation rate from 36.4 to 6.7 per 10,000 diabetics over an 11-year period [8]. Larsson et al found the incidence of major amputations to decrease by 78% (p < 0.001) [9].
Several studies showed significant reduction in the major amputation (amputation above the ankle) rate, as the most beneficial outcome of the team approach [7,8,9]. Krishnan., et al. reported a significant reduction of 82% in major amputation rate from 36.4 to 6.7 per 10,000 diabetics over an 11-year period [8]. Larsson et al found the incidence of major amputations to decrease by 78% (p < 0.001) [9].
Martinez., et al. showed that the team approach implemented with a clinical pathway reduced the rate of major amputation from 17.4% to 9.7% [7]. Likewise in NUH, the use of interdisciplinary team coupled with a clinical pathway also significantly reduced major amputation rate from 31.1% in 2002 to 17.9% in 2014 (p = 0.050).
Re-admission Rate
Few researchers studying the effect of the team approach, evaluated re-admission rate. Martinez et al did not find any significant reduction in re-admission rate (9.3% before team approach to 6.5% after team approach) [7]. In our study, our re-admission rate was significantly reduced from 13.1% in 2002 to 2.9% in 2014 (p = 0.032).
Few researchers studying the effect of the team approach, evaluated re-admission rate. Martinez et al did not find any significant reduction in re-admission rate (9.3% before team approach to 6.5% after team approach) [7]. In our study, our re-admission rate was significantly reduced from 13.1% in 2002 to 2.9% in 2014 (p = 0.032).
Complication Rate
Also, few researchers studying team approach evaluated the complication rate. Hedetoft., et al. suggested that the team approach could reduce foot complication rate [10]. Our complication rate in the 2014 cohort was 23.2% but compared to the 2002 cohort this difference was not statistically significant (p = 0.786).
Also, few researchers studying team approach evaluated the complication rate. Hedetoft., et al. suggested that the team approach could reduce foot complication rate [10]. Our complication rate in the 2014 cohort was 23.2% but compared to the 2002 cohort this difference was not statistically significant (p = 0.786).
Conclusion
NUH Team Approach coupled with a clinical pathway continued to show significant reduction in the length of stay, major amputation rate and re-admission rate. It did not show any difference in complication rate.
Acknowledgements
NIL
NIL
Conflict of interest
NIL
NIL
References
- “More effort to Promote Healthy Living Habits.” The Straits Times. N.p., 13 Apr/ 2016. Web. 12 Aug. 2016.
- “IDF Diabetes Atlas Seventh Edition.” International Diabetes Federation. N.p., n.d. Web. 12 Aug 2016.
- Nather Aziz., et al. “Value of Team Approach Combined with Clinical Pathway for Diabetic Foot Problems: A Clinical Evaluation”. Diabetic Foot & Ankle 1 (2010).
- Edmonds ME and Alethea VM. “Foster. Managing the Diabetic Foot. Malden, MA: Blackwell Pub., 2005. Print.
- Lavery Lawrence A., et al. “Disease Management for the Diabetic Foot: Effectiveness of a Diabetic Foot Prevention Program to Reduce Amputations and Hospitalizations”. Diabetes Research and Clinical Practice 70.1 (2005): 31-37.
- Gibbons and Gary W. “Improved Quality of Diabetic Foot Care, 1984 vs 1990”. Archives of Surgery128.5 (1993): 576.
- D Martiniz., et al. “Impact of a Clinical Pathway for the Diabetic Foot in a General Hospital”. Anales de Medicina Interna 21.9 (2004): 420-424.
- Krishnan S., et al. “Reduction in Diabetic Amputations Over 11 Years in a Defined U.K. Population: Benefits of Multidisciplinary Team Work and Continuous Prospective Audit”. Diabetes Care 31.1 (2007): 99-101.
- Larsson J., et al. “Decreasing Incidence of Major Amputation in Diabetic Patients: A Consequence of a Multidisciplinary Foot Care Team Approach?” Diabetic Medicine 12.9: (1995): 770-776.
- Hedetoft., et al. “Four-fold Increase in Foot Ulcers in Type 2 Diabetic Subjects without an Increase in Major Amputations by a Multidisciplinary Setting”. Diabetes Research and Clinical Practice 83.3 (2009): 353-357.
Citation:
Aziz Nather., et al. “Team Approach in the management of Diabetic Foot Wounds- the National University Hospital Experience”. Orthopaedic Surgery and Traumatology 1.1 (2016): 29-34.
Copyright: © 2016 Aziz Nather., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.