Clinical Opinion Article
Volume 2 Issue 1 - 2018
Radiation Safety Alert
1Voluntary Clinical Professor, University of New Mexico School of Medicine, Albuquerque, New Mexico
Desert Institute for Spine care, Phoenix, Arizona, Executive director, International Endoscopic Therapy Spine Society (endosc+opicspinetherapy.org)
2MD, Desert Institute for Spine Care
2MD, Desert Institute for Spine Care
*Corresponding Author: Anthony T Yeung, Voluntary Clinical Professor, University of New Mexico School of Medicine, Albuquerque, New Mexico.
Received: December 28, 2017; Published: January 08, 2018
Abstract
Introduction: With the interest and adoption of percutaneous minimally invasive procedures becoming an integral part of spine procedures, an awareness of the biological effects of ionizing radiation is more important than ever. There should also be a concern for radiation safety in today’s minimally invasive spine platform. What are the effects of long-term radiation on the surgeon and staff? What measures can be taken to minimize exposure during surgery and pain procedures? What are the lesser-known effects of ionizing radiation? This opinion article discusses what practical and readily available shielding can be purchased, and how can custom lead shielding of imaging equipment be used to promote radiation safety.
Introduction
More awareness of Radiation safety is needed, as minimally invasive surgery is dependent on the frequent use of intra-operative fluoroscopy to guide needles, surgical equipment aides, cannulas, and implants used in minimally invasive spine surgery. [1,2,3] In spite of many radiation prevention measures available, optimal protection shielding in the operating suite is still lacking. It is also erroneously considered less urgent to protect the surgeon’s hands because bench testing of lead gloves created erroneous conclusions that while radiation is blocked, the gloves may actually trap ionizating radiation inside the glove and do not actually protect the surgeon’s hands as advertised.
It is common for surgeons and interventionists to wear lead shielding to their body and thyroid, but not lead gloves or lead glasses
while performing procedures. Hand radiation exposure is controversial because.bench testing reveals backscatter radiation from the
glove surface on the far side of the surgeon’s hand. Accordingly, actual measurement of radiation of the surgeon’s hands during surgery
is necessary to determine the practical protective efficacy of lead gloves as well as lead shielding [4,5]. There are no known or few studies
that specifically compare the radiation doses to the surgeon’s hands using fluoroscopy with and without lead gloves, under operating
conditions and exposure to personnel in the OR.
Study Method
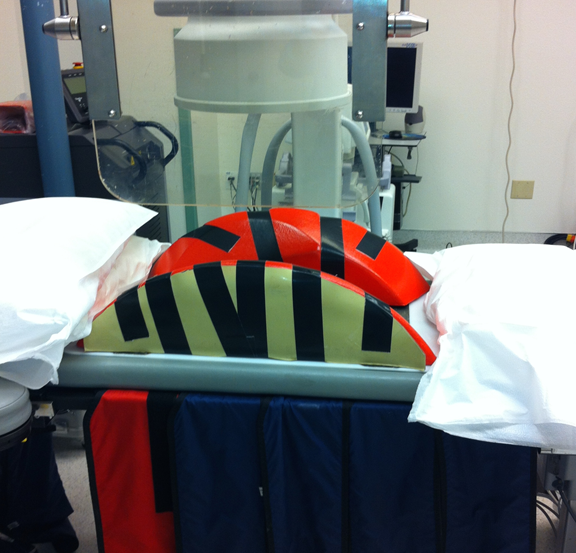
One Endoscopic practice’s simple steps to protect surgeon and staff included radiation safety measures installed in their operating suites. The methods start with protection in the operating room utilizing lead shielding of the operating table and patient positioning frames. Overhead mounted lead shields, lacking in most endoscopic operating suites, also helps reduce ionizating radiation to the surgeon and assistants in the operating room. The awareness of radiation scatter after it passes through the patient can also be minimized with available table and patient positioning frame shielding.
One Endoscopic practice’s simple steps to protect surgeon and staff included radiation safety measures installed in their operating suites. The methods start with protection in the operating room utilizing lead shielding of the operating table and patient positioning frames. Overhead mounted lead shields, lacking in most endoscopic operating suites, also helps reduce ionizating radiation to the surgeon and assistants in the operating room. The awareness of radiation scatter after it passes through the patient can also be minimized with available table and patient positioning frame shielding.
Radiation protection aprons, two piece garments and thyroid shields are routinely available. (Figure 1) However, lead glasses and operating room shielding is not commonly available. A Yeung built the first spine focused ambulatory surgical facility in the United States in 1998. He installed ceiling mounted lead shields in his operating rooms. Yeung anticipated the need for radiation safety due to the large number of endoscopic spine procedures being performed. Image guidance equipment such as ultrasound for the guidance of needles, and robotics, was not yet available for reducing radiation exposure. It was realized that radiation exposure would need maximum protection for the surgeon as well as the operating room personnel. A separate monitor measured room radiation with and without lead shielding of equipment estimated there was a reduction of 85% in and around the operating table with lead shielding and protection worn by the surgeon.
In 2010, a hand study was carried out prospectively in his Squaw Peak Surgical Facility in Phoenix from September 2008 to December 2009. The study was performed due to lectures at spine meeting by some respected key opinion leaders that lead gloves were not needed. This was due to bench testing of lead gloves thought to reduce radiation did not identify significant protection. Yeung wanted to actual radiation exposure to the dominant hand under actual Operating room conditions. The surgeon (ATY) wore a lithium fluoride thermo luminescent dosimeter ring on his ring finger on his the right (dominant) hand. The surgeon wore the same lead apron, thyroid shield and a pair of lead glasses in all the procedures. The same mobile C-arm fluoroscopy machine was used. The surgical procedures were endoscopic spine discectomy and spinal injections. The radiation time and dose to the dominant hand were measured in two separated periods. From September 2008 to November 2008, the surgeon performed the procedure without lead gloves. Then, from November 2008 to January 2009, the surgeon performed the procedures with lead gloves. (Figure 2) Total flouro time was the same for both periods. The cumulated data was tabulated and comparative statistical analysis was performed. Badge readings were compared.
Discussion
Answers to questions 1: What shielding and protective resources will decrease patient and staff exposure to X-rays? 2. What measures can be taken to minimize the surgeon’s exposure? 3. What basic knowledge is needed by the surgeon on the effects of ionizing radiation that may is not obvious? 4. What general principles during the training process are needed to protect trainees and us? 5. What technologies are being developed for endoscopic decompressive techniques other than hardware insertion?
When using a fluoroscope, the surgeon’s hands can be exposed both directly from the primary X-ray beam and secondly from scattered radiation reflected from the patient’s body and surrounding environment. Several studies did not recognize the risk of radiation exposure to the hands and concluded that the radiation dose to the hands may be worse with lead gloves than without because ionizing radiation because radiation that gets through is trapped inside the glove with bench testing. Others concluded that the effect of that radiation dose to the hands could be underestimated. A study reported that fluoroscopically assisted thoracolumbar pedicle screw placement exposes the spine surgeon to 10-12 times greater radiation levels than nonspinal musculoskeletal procedures. Another study by Wagner stated that forward-scattered and back scattered x-rays reduce the effectiveness of radiation-attenuating gloves, and lead gloves did not protect the surgeon’s fingers.
Our study results demonstrated that wearing lead gloves could reduce the radiation dose to the hands and fingers by 52%, which strongly supports using lead gloves for hand protection during endoscopic discectomy and spinal injections. Studies by Rampersaud (2000) and Mroz studying radiation exposure to the hands for vertebroplasty and pedicle screw insertion, concluded that surgeons would exceed the extremity dose limits without protection at approximately 300 procedures per year. Using lead shielding to protect the hands might allow a surgeon to perform up to 1000 or more procedures per year within safe limits. The author has performed over 10,000 surgical procedures, not counting at least 5 times as many injections in his 27 years practice in endoscopic spine surgery since 1991. Total radiation exposure is still below maximum recommended limits.
Conclusion
In addition to the obvious simple steps of radiation protection discussed, equipment for operating room shielding, image guidance, and robotics may be another answer to minimizing exposure for surgical procedures relying more on percutaneous and intra-operative imaging.
Based on our study demonstrating a decrease in radiation exposure to the hands, wearing lead gloves during endoscopic surgery and spinal injections is recommended. When shielding in the OR is used on the operating table, with Lead shielding mounted on the ceiling added to shield the surgeon’s face from scatter radiation, (Figure 3) over 85% of scatter radiation is eliminated to Surgeon and or personnel in additional to their the personal protective equipment.
Summary
- The use of table and surgical bolster shielding, ceiling mounted lead shields, all help reduce scatter radiation by 85% to the entire operating room (Figure 4)
- Face shield mounted on the OR ceiling protects further protects the surgeons thyroid, and eyes.
- The anesthesiologist gets negligible radiation when he further shields himself with a lead apron and lead shielding isolating the anesthesiologist from the OR table. Other personnel gets 15% of surgeon Radiation
- The glove data clearly demonstrate that for the approximate same exposure time using the ring dose-ometer, the radiation dose of hand can significantly attenuate 52% by wearing lead gloves.
References
- Synowitz M and Kiwit J. “Surgeon’s radiation exposure during percutaneous vertebroplasty”. Journal of Neurosurgery. Spine 4.2 (2006): 106-109.
- Rampersaud YR., et al. “Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion”. Spine 25.10 (2000): 2637-2645.
- Mroz TE., et al. “Radiation exposure to the surgeon performed the Spinal Disord Tech”. The Spine Journal 16.3 (2008): 343-354.
- Arnstein PM., et al. “The risk from radiation exposure during operative X-ray screening in hand surgery”. Journal of Hand Surgery 19.3 (1994): 393-396.
- Wagner LK and Mulhern OR. “Radiation-attenuating surgical gloves: effects of scatter and secondary electron production”. Radiology200.1 (1996): 45-46.
Citation:
Anthony T Yeung MD and Christopher A Yeung. “Radiation Safety Alert”. Orthopaedic Surgery and Traumatology 2.1 (2018):
264-268.
Copyright: © 2018 Anthony T Yeung MD and Christopher A Yeung. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.






































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.