Review Article
Volume 2 Issue 3 - 2018
Thoracic Outlet Syndrome in the Common Orthopaedic Practice: A Review
Department of Orthopaedic Surgery, “G. Gennimatas” Hospital, 54635 Thessaloniki, Greece
*Corresponding Author: NK Sferopoulos, Department of Orthopaedic Surgery, “G. Gennimatas” Hospital, 54635 Thessaloniki, Greece.
Received: January 03, 2018; Published: June 30, 2018
Abstract
Thoracic outlet syndrome is an often overlooked or misdiagnosed cause of neck, shoulder, and arm impairment. It is due to compression disorders of the neurovascular bundle in its passage from the cervical spine toward the axilla and proximal arm. The major source of confusion with regard to diagnosis is cervical spine or peripheral compressive/entrapment neuropathies and shoulder pathology. A careful and detailed medical history and physical examination is essential in the diagnosis of the syndrome, which is mainly clinical. The purpose of this review is to present a range of the clinical appearances of the syndrome in both children and adults, and to review the related literature.
Review
Thoracic outlet syndrome (TOS) is due to irritation or compression of brachial plexus and/or subclavian vessels at various points between the base of the neck and the axilla. Neurovascular compression may be observed most commonly in the interscalene triangle, but it also has been described in the costoclavicular and the subcoracoid space. Therefore, two levels or kinds of TOS are defined.
The upper thoracic or most likely called cervical outlet syndrome is due to compression in the scalene triangle between the anterior and medius scalene muscles in the neck. The lower or true thoracic outlet syndrome involves compression of the brachial plexus between the clavicle and the first rib in the costoclavicular space. The TOS was first described by the Greek physician Galen and Vesalius in the 2nd century AD.
A surprising amount of confusion surrounds TOS in general. However, most of the controversy involves patients with compression of the brachial plexus. The evaluation and treatment of patients with TOS is usually performed by vascular surgeons or neurosurgeons, but occasionally neurologists, physiatrists, family physicians, thoracic surgeons, orthopaedic surgeons, general surgeons and sometimes psychiatrists may also be involved.
A high index of suspicion and thorough knowledge is necessary to diagnose the disease, especially among orthopaedic surgeons. Although the orthopaedic surgeon is not involved in the treatment of these patients, he may be helpful in the localization of the site of compression excluding other commonly involved areas or in the identification of overlooked clinical symptoms and signs. Despite the wide range of reports referring to the syndrome in the literature, most of the pictures of the reported cases usually refer to its imaging features rather than to the different aspects of the clinical appearance of the patients.
There are three main types of TOS: neurogenic, venous, and arterial. However, the medical literature reflects 5 types of TOS: arterial; venous; traumatic neurovascular; true neurogenic; and disputed. Neurogenic TOS includes disorders produced by compression of the brachial plexus elements (brachial plexopathy). It accounts for 95% of all cases of TOS. Arterial TOS results from obstruction of the subclavian artery with claudication, thrombus formation, and possible embolization and accounts less than 1% of all cases of TOS. Venous TOS, also referred as Paget-Schroetter syndrome or primary ‘effort-induced thrombosis’, involves subclavian-axillary venous intermittent/positional occlusion, thrombus formation, and rare embolization, accounting about 4% of all cases of TOS.
Common local anomalies include an elongated transverse process of the seventh cervical vertebra, variations in the insertion of the anterior scalene muscle (ASM) or scalenus minimus muscle, the presence of a cervical rib, fibrous and muscular bands or hypertrophic scar tissue after clavicle fracture, variations in insertion or local hypertrophy, in athletes, of pectoralis minor, atypical course of neurovascular structures or abnormalities of the first thoracic rib. An elongated transverse process of the seventh cervical vertebra is the most commonly recognized cause of TOS (Figure 1). It is considered elongated if it extends beyond the tip of the first thoracic vertebra process immediately below it, as seen on cervical radiographs. A fibrous band connecting it to the first rib may also be evident.

Figure 1: Cervical plain radiograph of a 10-year-old girl
indicated elongated C7 transverse process on both sides that
was more pronounced and symptomatic on the left side.
Some people are born with an extra incomplete and very small rib above their first rib, which protrudes out into the superior thoracic outlet space. This is called a ‘cervical rib’ because of its attachment to the seventh cervical vertebra. Most cases of cervical ribs vary widely in size and shape and are not clinically relevant since they do not have symptoms. Cervical ribs causing clinical symptoms are usually large and frequently fused to the first rib (Figure 2), and may be complicated by aneurysm formation or thrombosis. A rudimentary rib may be associated with fibrous changes around the brachial plexus nerves inducing compression and causing the symptoms and signs of TOS. On imaging, cervical ribs can be distinguished because their transverse processes are directed inferolaterally, whereas those of the adjacent thoracic spine are directed anterolaterally.
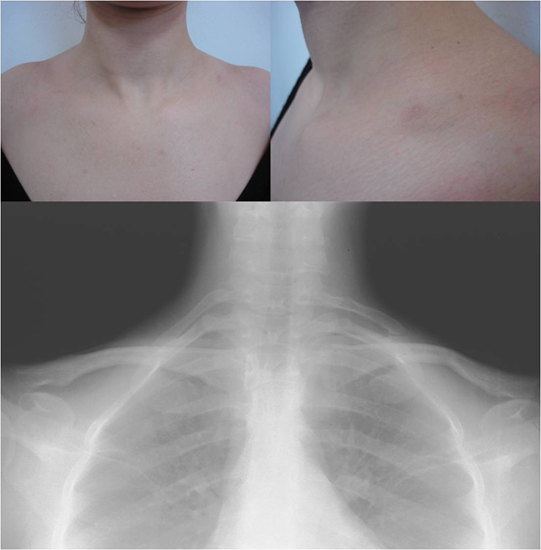
Figure 2: A 13-year-old girl demonstrated the typical findings of vascular thoracic outlet syndrome on
the right side. Abduction of the arms to 90 degrees in external rotation, in about one minute after the test,
caused pain, cyanosis and a feeling of cooler and swollen localized in the whole right upper extremity. The
radiograph indicated rudimentary short cervical ribs on both sides of the seventh cervical vertebra.
History, physical examination, provocative tests, ultrasound, radiological evaluation and electrodiagnostic evaluation are essential in the diagnostic investigation of TOS. Compression of the brachial plexus may be identified by pain, muscle spasm, weakness and a 'pins and needles' feeling and/or numbness, aggravated by overhead positions of the arms, in the cervical region, shoulder, arm, forearm or hand. Tenderness of brachial plexus in the supraclavicular area and occasionally painless wasting of intrinsic hand muscles may be evident. Compression of the subclavian artery results in pain, coldness, and paleness of the arm, while compression of the subclavian vein results in swelling, pain, and possibly a bluish coloration of the arm (Figure 3).
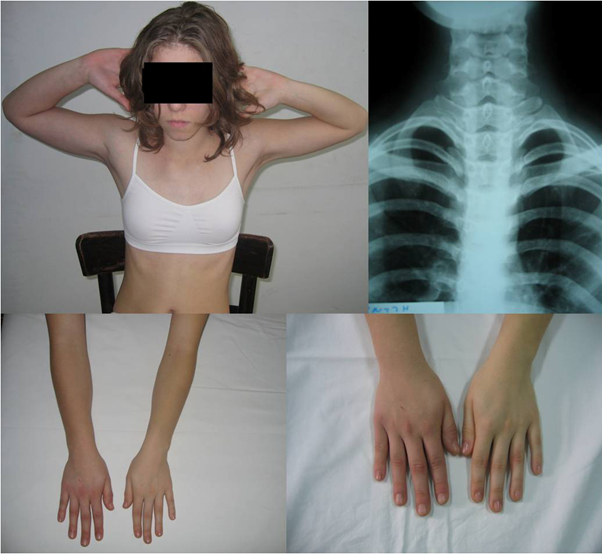
Figure 3: A 22-year-old woman complained for a painless bony lump over the medial border
of the left clavicle. Physical examination revealed brachial plexus nerve compression symptoms
that were more expressed in the left side, though they were also present on the right side too.
The radiograph showed fully developed symmetrical cervical ribs originating from the seventh
cervical vertebra. A joint process of the first rib at the place of insertion of the cervical rib was
clearly evident on the left side. The cervical column was not abnormally shaped.
There is currently no single clinical sign that makes the diagnosis of TOS with any degree of certainty. Loss or weakening of the radial pulse or signs of blanching of the skin in the hands may be evident during either abduction and external rotation of the shoulder while the elbow is flexed to 90 degrees, which is described as Wright's test, or during abduction with slight extension of the patient’s shoulder while he hyperextends the neck and turns the head toward the ipsilateral side, which is described as Adson's sign. The tingling sensation that may point to nervous system irritation caused by light percussion or by flicking specific nerves in the fingers or the wrists is described as Hoffman’s sign. The ‘compression test’ of the brachial plexus causes radiation of pain and/or numbness into the affected arm.
Therefore, the cervical spine, shoulder and distal peripheral nerves should be studied by radiological and electrophysiological studies in all cases. There is no laboratory test confirming TOS and radiological as well as electrophysiological testing is usually normal. Axial imaging, including computed tomography and magnetic resonance imaging, has not been proved sufficiently useful because no structural abnormality usually exists. In cases of suspected neurogenic TOS, electrophysiological nerve studies and ASM blocks provide guidance when screening for patients likely to benefit from surgical decompression.
A common diagnostic technique for vascular TOS is duplex ultrasonography, which has generally replaced more invasive angiographic techniques. Lesser degrees of arterial compression have been shown in normal individuals in various arm positions and are thought to be of little significance without other criteria of TOS. Venography may be both diagnostic and therapeutic in venous TOS. Helical computed tomography offers a three-dimensional view of the thoracic outlet, and may be valuable in the detection of anatomical variations, which may predispose patients to TOS.
TOS may also be due to acute or chronic injury. The most frequent cause is acute trauma following a clavicle fracture most likely caused by a car accident. The two groups of people most likely to develop chronic TOS are either those suffering from neck injuries or professionals who frequently raise their arms above the head, such as those working with computers in non-ergonomic postures for extended periods of time, athletes (swimmers, volleyball players, dancers, badminton players, baseball pitchers, and weightlifters), rock climbers, electricians and musicians. TOS can also be related to forward head posture.
Pediatric TOS may also be related to acute or chronic infection of the cervical lymph nodes and subsequent cervical inflammation. Other rarer acquired causes include tumors, hyperostosis, osteomyelitis and pregnancy. TOS can be related to cerebrovascular arterial insufficiency when affecting the subclavian artery. It can also affect the vertebral artery producing vision disturbances, including transient blindness, and embolic cerebral infarction.
TOS should be differentiated from other conditions that can produce similar symptoms including rotator cuff tear, cervical disc disorders, fibromyalgia, multiple sclerosis, and complex regional pain syndrome. TOS is often the underlying cause of refractory upper limb conditions like frozen shoulder and carpal tunnel syndrome that frequently defy standard treatment protocols. Increased awareness of the clinical symptoms and signs of TOS is essential for the orthopaedic surgeon to secure that the syndrome will not be underrated, overlooked and misdiagnosed at the discharge of the patient and that appropriate treatment will be offered.
Furthermore, Paget-Schroetter disease, also known as Paget-von Schrötter disease, or primary ‘effort-induced thrombosis’ remains largely an unfamiliar disease and the incidence of patients leaving the hospital undiagnosed is high. It is a form of upper extremity deep vein thrombosis, a medical condition in which blood clots form in the axillary or subclavian veins. They have the potential to cause a pulmonary embolism. The syndrome is commoner in young people who are engaged in competitive sports. It is differentiated from secondary causes of upper extremity caused by intravascular catheters. Symptoms may include sudden onset of pain, warmth, redness, blueness and swelling in the arm (Figure 4).

Figure 4: A 41-year-old woman with a diagnosed Paget-Schroetter syndrome 6 weeks ago. Clinical pictures showing diffuse swelling and dilated prominent veins on the right side of the chest, shoulder, arm and breast.
Diagnosis is usually confirmed with an ultrasound. The evaluation of the vascular surgical team should always be asked to ensure that an early diagnosis is made so that prompt treatment can be initiated for a better overall outcome.
References
- Gilliatt RW., et al. “Wasting of the hand associated with a cervical rib or band”. Journal of Neurology, Neurosurgery, and Psychiatry 33.5 (1970): 615-624.
- Carroll RE and Hurst LC. “The relationship of thoracic outlet syndrome and carpal tunnel syndrome”. Clinical Orthopaedics and Related Research 164 (1982): 149-153.
- Daskalakis MK. “Thoracic outlet compression syndrome: current concepts and surgical experience”. International Journal of Surgery 68.4 (1983): 337-344.
- Palma A and Carini F. “Variation of the transverse apophysis of the 7th cervical vertebra: anatomo-radiological study of an isolated population”. Archivio Italiano Di Anatomia E Di Embriologia 95.1 (1990): 11-16.
- Campbell JN., et al. “Thoracic outlet syndrome. Neurosurgical perspective”. Neurosurgery Clinics of North America 2.1 (1991): 227-233.
- Melliere D., et al. “Thoracic outlet syndrome caused by tumor of the first rib”. Journal of Vascular Surgery 14.2 (1991): 235-240.
- Dellon AL. “The results of supraclavicular brachial plexus neurolysis (without first rib resection) in management of post-traumatic "thoracic outlet syndrome"”. Journal of Reconstructive Microsurgery 9.1 (1993): 11-17.
- Panegyres PK., et al. “Thoracic outlet syndromes and magnetic resonance imaging”. Brain 116.4 (1993): 823-841.
- Sell JJ., et al. “Rotational vertebrobasilar insufficiency as a component of thoracic outlet syndrome resulting in transient blindness. Case report”. Journal of Neurosurgery 81.4 (1994): 617-619.
- Ranney D. “Thoracic outlet: an anatomical redefinition that makes clinical sense”. Clinical Anatomy 9.1 (1996): 50-52.
- Atasoy E. “Thoracic outlet compression syndrome”. Orthopedic Clinics of North America 27.2 (1996): 265-303.
- Hicken GJ and Ameli FM. “Management of subclavian-axillary vein thrombosis: a review”. Canadian Journal of Surgery 41.1 (1998): 13-25.
- Jordan SE and Machleder HI. “Diagnosis of thoracic outlet syndrome using electro physiologically guided anterior scalene blocks”. Annals of Vascular Surgery 12.3 (1998): 260-264.
- Wilbourn AJ. “Thoracic outlet syndromes”. Neurologic Clinics 17.3 (1999): 477-497.
- Le Forestier N., et al. “True neurological thoracic outlet syndrome”. Revue Neurologique 156.1 (2000): 34-40.
- Parziale JR., et al. “Thoracic outlet syndrome”. American Journal of Orthopedics 29.5 (2000): 353-360.
- MackinnonSE, Novak CB. Washington University School of Medicine, St. Louis, Missouri March, 2001.
- Vercellio G., et al. “Thoracic outlet syndrome in pediatrics: clinical presentation, surgical treatment, and outcome in a series of eight children”. Journal of Pediatric Surgery 38.1 (2003): 58-61.
- Nannapaneni R and Marks SM. “Neurogenic thoracic outlet syndrome”. British Journal of Neurosurgery 17(2003): 144-148.
- Davidovic LB., et al. “Vascular thoracic outlet syndrome”. World Journal of Surgery 27.5 (2003): 545-550.
- Howard M., et al. “Documentation of brachial plexus compression (in the thoracic inlet) utilizing provocative neurosensory and muscular testing”. Journal of Reconstructive Microsurgery 19.5 (2003): 303-312.
- Crosby CA and Wehbé MA. “Conservative treatment for thoracic outlet syndrome”. Hand Clinics 20.1 (2004): 43-49.
- Brantigan CO and Roos DB. “Etiology of neurogenic thoracic outlet syndrome”. Hand Clinics 20(2004): 17-22.
- Atasoy E. “Thoracic outlet syndrome: anatomy”. Hand Clinics 20.1 (2004): 7-14.
- Tolson TD. “"EMG" for thoracic outlet syndrome”. Hand Clinics 20.1 (2004): 37-42.
- Ambrad-Chalela E., et al. “Recurrent neurogenic thoracic outlet syndrome”. The American Journal of Surgery 187.4 (2004): 505-510.
- Huang JH and Zager EL. “Thoracic outlet syndrome”. Neurosurgery 55.4 (2004): 897-903.
- Köknel Talu G. “Thoracic outlet syndrome”. Agriculture 17.2 (2005): 5-9.
- Becker MH and Lassner F. “The asymptomatic thoracic outlet compression syndrome”. Handchirurgie, Mikrochirurgie, Plastische Chirurgie 38.1 (2006): 51-55.
- Shebel ND and Marin A. “Effort thrombosis (Paget-Schroetter syndrome) in active young adults: current concepts in diagnosis and treatment”. Journal of Vascular Nursing 24.4 (2006): 116-126.
- Corwin HM. “Compression neuropathies of the upper extremity”. Clinics in Occupational and Environmental Medicine 5.2 (2006): 333-352.
- Demondion X., et al. “Imaging assessment of thoracic outlet syndrome”. Radiographics 26.6 (2006): 1735-1750.
- Singh D., et al. “Thoracic outlet syndrome: Presentation and management”. Indian Journal of Surgery 68 (2006): 93-96.
- Machanic BI and Sanders RJ. “Medial antebrachial cutaneous nerve measurements to diagnose neurogenic thoracic outlet syndrome”. Annals of Vascular Surgery 22.2 (2008): 248-254.
- Arthur LG., et al. “Pediatric thoracic outlet syndrome: a disorder with serious vascular complications”. Journal of Pediatric Surgery 43.6 (2008): 1089-1094.
- Flinterman LE., et al. “Current perspective of venous thrombosis in the upper extremity”. Journal of Thrombosis and Haemostasis 6.8 (2008): 1262-1266.
- Sanders RJ., et al. “Thoracic outlet syndrome: a review”. Neurologist 14.6 (2008): 365-373.
- Fugate MW., et al. “Current management of thoracic outlet syndrome”. Current Treatment Options in Cardiovascular Medicine 11.2 (2009): 176-183.
- Davidović LB., et al. “Arterial complications of thoracic outlet syndrome”. The American Surgeon 75.3 (2009): 235-239.
- Nichols AW. “Diagnosis and management of thoracic outlet syndrome”. Current Sports Medicine Reports 8.5 (2009): 240-249.
- Maru S., et al. “Thoracic outlet syndrome in children and young adults”. European Journal of Vascular and Endovascular Surgery 38.5 (2009): 560-564.
- Stansby G and Lambert D. “Thoracic outlet syndrome in children and young adults”. European Journal of Vascular and Endovascular Surgery 38.5 (2009): 565-566.
- Di Nisio M., et al. “Accuracy of diagnostic tests for clinically suspected upper extremity deep vein thrombosis: a systematic review”. Journal of Thrombosis and Haemostasis 8.4 (2010): 684-692.
- Illig KA and Doyle AJ. “A comprehensive review of Paget-Schroetter syndrome”. Journal of Vascular Surgery 51.6 (2010): 1538-1547.
- Hooper TL., et al. “Thoracic outlet syndrome: a controversial clinical condition. Part 1: anatomy, and clinical examination/diagnosis”. The Journal of Manual & Manipulative Therapy 18.2 (2010): 74-83.
- Vaught MS., et al. “Association of disturbances in the thoracic outlet in subjects with carpal tunnel syndrome: a case-control study”. Journal of Hand Therapy 24.1 (2011): 44-51.
- Mai C and Hunt D. “Upper-extremity deep venous thrombosis: a review”. The American Journal of Medicine 124.5 (2011): 402-427.
- Hooper TL., et al. “Thoracic outlet syndrome: a controversial clinical condition. Part 2: non-surgical and surgical management”. The Journal of Manual & Manipulative Therapy 18.3 (2010): 132-138.
- Chang K., et al. “Spectrum of thoracic outlet syndrome presentation in adolescents”. Archives of Surgery 146.12 (2011): 1383-1387.
- Bokhari RF., et al. “Prevalence of cervical ribs and elongated transverse processes in Saudi Arabia”. Saudi Medical Journal 33.1 (2012): 66-69.
- Kemp CD., et al. “Thoracic outlet syndrome caused by fibrous dysplasia of the first rib”. The Annals of Thoracic Surgery 93.3 (2012): 994-996.
- Dubuisson A., et al. “Post-traumatic thoracic outlet syndrome”. Acta Neurochirurgica (Wien) 154.3 (2012): 517-526.
- Chan KH., et al. “Clinical presentation of cervical ribs in the pediatric population”. The Journal of Pediatrics 162.3 (2013): 635-636.
- Chang KZ., et al. “The significance of cervical ribs in thoracic outlet syndrome”. Journal of Vascular Surgery57.3 (2013): 771-775.
- Walden MJ., et al. “Cervical ribs: identification on MRI and clinical relevance”. Clinical Imaging 37.5 (2013): 938-941.
- Sanders RJ and Annest SJ. “Thoracic outlet and pectoralis minor syndromes”. Seminars in Vascular Surgery 27.2 (2014): 86-117.
- Klaassen Z., et al. “Thoracic outlet syndrome: a neurological and vascular disorder”. Clinical Anatomy 27.5 (2014): 724-732.
- Sonoo M. “Thoracic outlet syndrome”. Brain Nerve 66.12 (2014): 1429-1439.
- Reidler JS., et al. “Thoracic outlet syndrome caused by synostosis of the first and second thoracic ribs: 2 case reports and review of the literature”. Journal of Hand Surgery 39.12 (2014): 2444-2447.
- Singh VK., et al. “Diagnostic value of magnetic resonance imaging in thoracic outlet syndrome”. Journal of Orthopaedic Surgery 22.2 (2014): 228-231.
- Rehemutula A., et al. “Managing pediatric thoracic outlet syndrome”. Italian Journal of Pediatrics 41 (2015): 22.
- Bhat MH., et al. “Prevalence of cervical ribs and elongated transverse processes in Kashmiri population”. International Journal of Research in Medical Sciences 3 (2015): 3763-3765.
- Kuhn JE., et al. “Thoracic outlet syndrome”. Journal of the American Academy of Orthopaedic Surgeons 23.4 (2015): 222-232.
- Palmer OP and Weaver FA. “Bilateral cervical ribs causing cerebellar stroke and arterial thoracic outlet syndrome: a case report and review of the literature”. Annals of Vascular Surgery 29.4 (2015): 840.e1-4.
- Lugo J., et al. “Acute Paget-Schroetter syndrome: does the first rib routinely need to be removed after thrombolysis?” Annals of Vascular Surgery 29.6 (2015): 1073-1077.
- Naeem M., et al. “Paget-Schroetter syndrome: A review and Algorithm (WASPS-IR)”. Phlebology 30.10 (2015): 675-686.
- Ijaopo R., et al. “A case of Paget-Schroetter syndrome (PSS) in a young judo tutor: a case report”. Journal of Medical Case Reports 10 (2016): 63.
- Higashihara M., et al. “Neurological Signs and Symptoms of True Neurogenic Thoracic Outlet Syndrome”. Brain Nerve 68.5 (2016): 521-529.
- Ferrante MA and Ferrante ND. “The thoracic outlet syndromes: Part 1. Overview of the thoracic outlet syndromes and review of true neurogenic thoracic outlet syndrome”. Muscle Nerve 55.6 (2017): 782-793.
- Ferrante MA and Ferrante ND. “The thoracic outlet syndromes: Part 2. The arterial, venous, neurovascular, and disputed thoracicoutlet syndromes”. Muscle Nerve 56.4 (2017): 663-673.
- https://en.wikipedia.org/wiki/Thoracic_outlet_syndrome
- https://en.wikipedia.org/wiki/Cervical_rib
- https://en.wikipedia.org/wiki/Paget%E2%80%93Schroetter_disease
Citation:
NK Sferopoulos. “Thoracic Outlet Syndrome in the Common Orthopaedic Practice: A Review”. Orthopaedic Surgery and
Traumatology 2.3 (2018): 322-329.
Copyright: © 2018 NK Sferopoulos. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.