Research Article
Volume 2 Issue 4 - 2018
Abnormal Movements
Department of Orthopedics, Founder and Director of the Unit Complex Spine Surgery Center and Scoliosis Surgery Section, Italy
*Corresponding Author: Pier Paolo Mura, Department of Orthopedics, Founder and Director of the Unit Complex Spine Surgery Center and Scoliosis Surgery Section, Italy.
Received: July 26, 2018; Published: September 15, 2018
Abstract
Study: The stability of the spine is defined as the possibility for the vertebrae to keep their physiological relationship and limit relative displacements during postures and whilst lifting loads. Degenerative joint processes and intervertebral facets influence the stability of the motion segment.
Instability is defined as "functional" when the ability of the spine to maintain the physical characteristics during the performance of normal activities ceases to exist. A pathological change can greatly influence the mechanics of the spine
Objectives: The reason for surgery is not to prevent the rapid aggravation of the deformity but to treat the pain and, in selected cases, to restore the physiological curves on the sagittal plane in order for the patient to return to a normal life.
Results: Age is not a contraindication to surgery. The study was carried out on 106 scoliosis patients aged between 60 and 85 treated in our operating unit from 2011 to 2015 with a maximum follow-up of six years and a minimum of three years. The study yielded good results in 87% of cases and complications in 13%.
Introduction
The spinal column is made of segments, called motion segments, made from two adjacent vertebrae and the soft interconnected tissue. In normal conditions this is capable of satisfying the essential functional requirements such as: strength, mobility and stability. The stability of the spine is defined as the possibility for the vertebrae to keep their physiological relationship and limit relative displacements during postures and whilst lifting loads. Degenerative joint processes and intervertebral facets influence the stability of the motion segment.
Instability is defined as "functional" when the ability of the spine to maintain the physical characteristics during the performance of normal activities ceases to exist. A pathological change can greatly influence the mechanics of the spine. The loss of rigidity of the motion segment, such that the application of forces on that motion segment produces more alterations compared to those that could occur in a normal structure, results in a painful condition and a progression of the deformity, causing instability.
In biomechanics, instability is defined as an anomalous response to the different loads applied, characterized by abnormal kinematic movements of the motion segment. It can be caused by structural failure as a consequence to an acute stress, from degenerative processes due to minimal stresses that persist over time and/or muscular dysfunction. The degenerative processes of the spine, in particular of the lumbar region, generally and primarily affect the intervertebral disc, leading to a modification of its physical properties of elasticity and mechanical resistance.
Materials and Methods
The degeneration of the disc can cause two adjacent discs to slip on one another. This causes laxity in the of the ligamentous network, which is responsible for the partial subluxation of the facet joints. The stresses on the facet joints cause osteoarthritis with osteophytosis, which in turn causes a narrowing of the lateral processes of the spinal canal and of the foramen. Osteoarthritis of the facet joints, with consequent loss of their normal structural support, plays a role of primary importance in the development of degenerative spondylolisthesis, which occurs at a higher percentage at the L4/L5 level for biomechanical reasons.
As the instability in the motion segments progresses, it can become cause for an imbalance in the coronal plane (degenerative adult scoliosis), in as much as the instability progressively deforms the structure of the disc, modifying its elasto-plastic properties causing an anomalous change in the ability to react and withstand loads. This instability causes an alteration of the geometrical relations between the individual vertebrae, resulting in subluxation (lateralisthesis) phenomena and rotation of the motion segments and consequently the deformity on the coronal plane is also associated with that on the sagittal plane.
In the various developmental stages of the degenerative process with consequent instability, an imbalance in the sagittal plane can be determined, where the spinal column is no longer able to withstand the loads to which it is subjected, in an upright position, with the search for a compensation of the hips and knees. Hence the loss of physiological lordosis with a tendency to progressive kyphosis. The alteration on the sagittal plane gives rise to an actual spinal deformity, characterized by variations in the sacral inclination, the dorsal-lumbar joint with subversion of the spino-pelvic parameters.
A stable and balanced spine without abnormal movements is a pain free spine. Pain appears following a biomechanical alteration with secondary instability. Pain is worsened when the instability is associated with an imbalance on the coronal plane and, especially, on the sagittal plane; in fact, in this case, pain is also caused by the muscular work necessary in the search of postural compensation. The intervertebral disc is composed of the annulus fibrosus and the nucleus pulposus. The nucleus pulposus of a healthy disk constitutes two thirds of the disk surface and supports more than 70% of the load.
Up until the third decade of life, the gel of the inner nucleus pulposus is made of 90% water, but this content decreases to about 65% in the next four decades of life. Repeated load forces and torsional forces can cause micro traumas to the detriment of the disc, resulting in a further loss of nutrition and hydration in the nucleus. All this can allow the material contained in the nucleus to migrate into the epidural space and cause nerve root compression or irritation.
The degenerated intervertebral disc which causes pain, has a lower pH when compared to a "normal" disc. The discopathy seems to show, in fact, an increase in the concentration of neuropeptides, such as the Substance P (SP), Calcitonine (CGRP) and Vasoactive Intestinal Peptide (VIP) in the dorsal root ganglion, implicating their possible role in the transmission or modulation of pain.
The SUBSTANCE P (SP) probably modulates the initial nociceptive signals received in the gray matter of the spinal cord marrow for the release of neuropeptides and this may occur in response to harmful biochemical forces and environmental factors (biomechanical stress, micro trauma..), stimulating the synthesis of inflammatory agents (cytokines, prostaglandin E2) and degrading enzymes (proteases, collagenesis).
Inflammatory factors are responsible for pain. Corticosteroids inhibit the production of arachidonic acid and its metabolites, inhibiting the activity of phospholipase A2 (PLA2). PLA2 levels, which play a role in the inflammatory process, may also incite degeneration of the disc and sensitization of nerve fibers. Neurotransmitters and biochemical factors can sensitize the neural elements in the motion segment so that normal biomechanical stresses induced by previously asymptomatic movements cause pain. Furthermore, the lesions and the subsequent neurochemical cascade can modify or prolong the pain stimulus and initiate degenerative and inflammatory changes, which lead to further biochemical and morphological changes.
It is not clear if the biochemical changes that occur with disc degeneration are the consequence or cause of these pain conditions, however the inflammatory factors can create the environmental substrate in which the biomechanical forces cause pain with various characteristics and in varying degrees.
Results
Our case study includes
A retrospective analysis of 106 scoliosis patients aged between 60 and 85 treated in our operating unit from 2011 to 2015 with a maximum follow-up of six years and a minimum of three years. They all suffered chronically with a severe limitation in their quality of life and had no relief from non-surgical treatment. For this reason, and after being appropriately informed about the surgery, completing preoperative assessment of their general state, as well as careful and detailed preoperative planning, the patients underwent surgery.
A retrospective analysis of 106 scoliosis patients aged between 60 and 85 treated in our operating unit from 2011 to 2015 with a maximum follow-up of six years and a minimum of three years. They all suffered chronically with a severe limitation in their quality of life and had no relief from non-surgical treatment. For this reason, and after being appropriately informed about the surgery, completing preoperative assessment of their general state, as well as careful and detailed preoperative planning, the patients underwent surgery.
Clinical, radiographic, MRI and, in some cases, CT study of peduncles. It was scoliosis with a Cobb angle of up to 30 degrees that in 70% of cases was associated with an imbalance on the sagittal plane with spino-pelvic parameters altered to varying degrees.
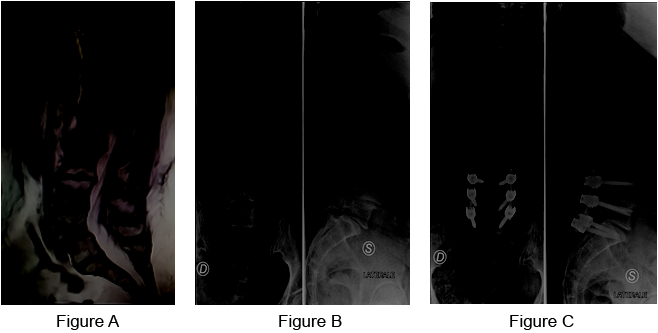
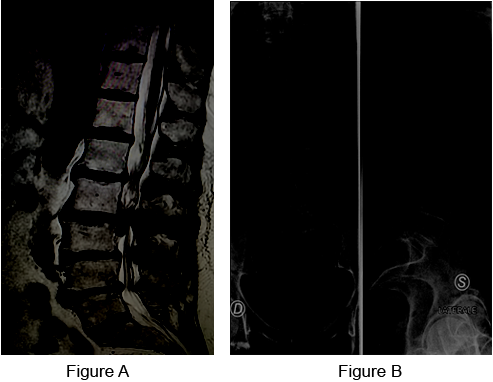
Case 1: Woman, 63 years old.
Figure a: Preoperative MRI.
Figure b: Preoperative RX: Multilevel degenerative disease L4L5, L5S1 with L4L5 listesi.
Figure c: Postoperative RX: Reduction of the listesi and arthrodesis instrumented on the L4L5S1 levels with the insertion of 6 Titanium screws.
Figure a: Preoperative MRI.
Figure b: Preoperative RX: Multilevel degenerative disease L4L5, L5S1 with L4L5 listesi.
Figure c: Postoperative RX: Reduction of the listesi and arthrodesis instrumented on the L4L5S1 levels with the insertion of 6 Titanium screws.
In 80% of cases the patients were ASA 2 whilst in 20% of cases they were ASA 3. In 70% of cases the surgical approach was posterior using screws and sub laminar strips. In the more elastic deformities a good correction was obtained with a rebalancing of about 80% on the coronal plane and with acceptable pelvic spinal parameters.
In the less elastic forms, a combined XLIF lateral approach has been associated with the insertion of cages one/two levels further back with Smith Petersen and/or Ponte osteotomies, screws and rods and sub laminar strips. Assumption of the standing position on the first or second day post-surgery with discharge on third/fourth or fifth day.
The study yielded good results in 87% of cases.
There were complications in 13% of cases.
There were complications in 13% of cases.
- Mainly mechanical
- Transient neurological
- No deaths
- No deep infections
- In two cases a fracture of the overlying vertebra needing another surgical intervention within three months of the original surgery.
- In three cases pull out of the screws
- In three cases broken rods
- One case of repositioning the screws
- In three cases transient radiculopathy
- In one case loosening of the screws in the proximal thoracic tract due to insufficient sagittal rebalancing. Two cases of superficial infection of the wound.
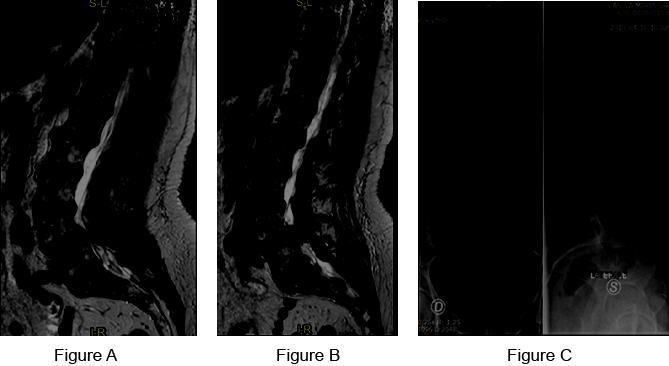
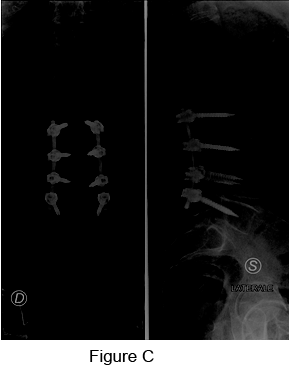
Case 2: Woman, 74 years old – Preoperative.
Figure a, b: Preoperative MRI.
Figure c: Preoperative RX: Severe degenerative disease of L4L5 with spondylolisthesis and discopathy, severely symptomatic.
Figure a, b: Preoperative MRI.
Figure c: Preoperative RX: Severe degenerative disease of L4L5 with spondylolisthesis and discopathy, severely symptomatic.

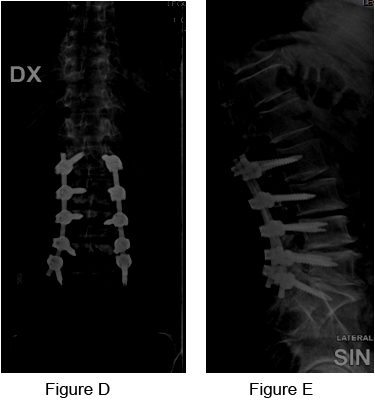
Case 2: Postoperative
Figure d, e: Postoperative RX: Reduction of the listesi and instrumented arthrodesis with the insertion of 4 Titanium screws.
Figure d, e: Postoperative RX: Reduction of the listesi and instrumented arthrodesis with the insertion of 4 Titanium screws.
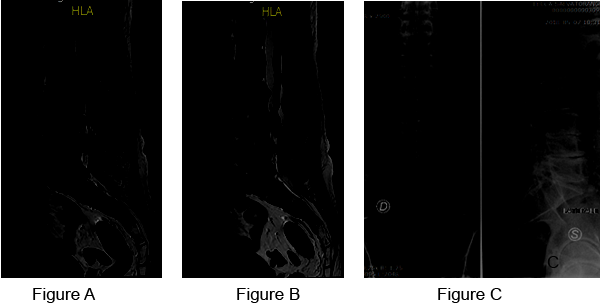
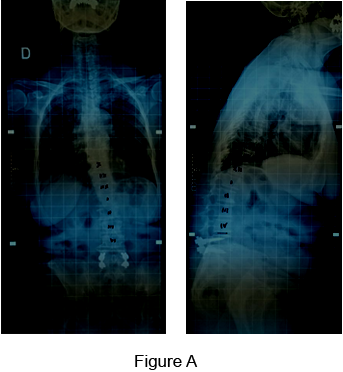
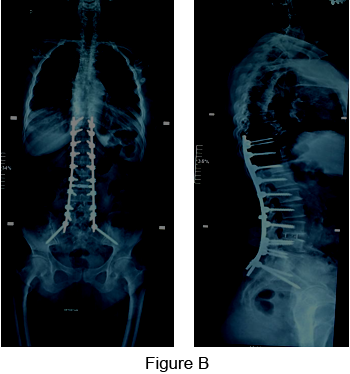
Case 3: Man, 60 years old – Preoperative.
Figure a, b: Preoperative MRI.
Figure c: Preoperative RX: Severe degenerative pathology of the lumbar spine, from L2 to S1, with sagittal imbalance, radiculopathy and ambulatory deficit.
Figure a, b: Preoperative MRI.
Figure c: Preoperative RX: Severe degenerative pathology of the lumbar spine, from L2 to S1, with sagittal imbalance, radiculopathy and ambulatory deficit.
Case 3: Postoperative.
Figure d, e: Postoperative RX: Decompression of nerve strings and arthrodesis instrumented by L2 to S1 with the insertion of 10 Titanium screws.
Figure d, e: Postoperative RX: Decompression of nerve strings and arthrodesis instrumented by L2 to S1 with the insertion of 10 Titanium screws.
Case 4: Woman, 80 years old – Preoperative.
Figure a: Preoperative MRI.
Figure b: Preoperative RX: Degenerative lumbar tract syndrome from L2 to L5, with L4L5 stenosis with severe ambulatory deficit.
Figure a: Preoperative MRI.
Figure b: Preoperative RX: Degenerative lumbar tract syndrome from L2 to L5, with L4L5 stenosis with severe ambulatory deficit.
Case 4: Postoperative.
Figure c: Postoperative RX: Decompression of nerve structures and arthrodesis instrumented by L2 to L5 with the insertion of 8 Titanium screw.
Figure c: Postoperative RX: Decompression of nerve structures and arthrodesis instrumented by L2 to L5 with the insertion of 8 Titanium screw.
Case 5: Woman, 75 years old – Preoperative.
Figure a: Preoperative RX: Patient already treated surgically for lumbar stabilization from L5 to S1. Degenerative pathology and serious sagittal imbalance and ambulatory deficit.
Figure a: Preoperative RX: Patient already treated surgically for lumbar stabilization from L5 to S1. Degenerative pathology and serious sagittal imbalance and ambulatory deficit.
Case 5: Postoperative.
Figure b: Postoperative RX: Double surgical approach with insertion of a cage between L4-L3. Correction and stabilization of the deformity.
Figure b: Postoperative RX: Double surgical approach with insertion of a cage between L4-L3. Correction and stabilization of the deformity.
Conclusions
The vertebral column that becomes pathological alters its stability, its alignment and balance and the movement becomes abnormal, all this translates into pain that is often chronic, disabling and does not benefit from common care. The surgeon is involved in dealing with difficult and delicate interventions to restore stability and normal balance, blocking the abnormal movement that causes pain.
The surgeon must have extensive knowledge of both the anatomy and the pathological anatomy of the spine, as well as the necessary techniques required to achieve all the goals needed in order to improve the quality of life of each patient.
The objective of surgical treatment is to obtain mechanical stability of the spine, which because cause of lumbar pain, fixing screws and rods in the sick vertebral segments, and to balance the spine in the sagittal and coronal plane and sometimes it's necessary to perform osteotomy and to put cage in the intervertebral space with posterior or combined approach and when necessary, to decompress nervous system. It's important to associate bone fusion opening joint and using in general autologous bone.
References
- Kong MH., et al. “Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology by using kinetic magnetic resonance imaging”. Spine (Phila Pa 1976) 34.23 (2009): 2537-2544.
- McGregor AH., et al. “Quantitative assessment of the motion of the lumbar spine in the low back pain population and the effect of different spinal pathologies of this motion”. European Spine Journal 6.5 (1997): 308-315.
- Miao J., et al. “Motion characteristics of the vertebral segments with lumbar degenerative spondylolisthesis in elderly patients”.European Spine Journal 22.2 (2013) 425-43.
- Paholpak P., et al. “An increase in height of spinous process is associated with decreased heights of intervertebral disc and vertebral body in the degenerative process of lumbar spine”. European Spine Journal 22.9 (2013): 2030-2034.
- Ruberté LM., et al. “Influence of single-level lumbar degenerative disc disease on the behavior of the adjacent segments – A finite element model study”. Journal of Biomechanics 42.3 (2009): 341-348.
- Seligman JV., et al. “Computer analysis of spinal segment motion in degenerative disc disease with and without axial loading”. Spine (Phila Pa 1976) 9.6 (1984): 566-573.
- Yao Q., et al. “Motion characteristics of the lumbar spinous processes with degenerative disc disease and degenerative spondylolisthesis”.European Spine Journal 22.12 (2013): 2702-2709.
Citation:
Pier Paolo Mura., et al. “Abnormal Movements”. Orthopaedic Surgery and Traumatology 2.4 (2018): 378-386.
Copyright: © 2018 Pier Paolo Mura., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.