Case Report
Volume 3 Issue 1 - 2019
Synovial Tuberculosis Masquerading As Monoarticular Inflammatory Arthritis
International Islamic University Medical Centre, Kuantan, Pahang
*Corresponding Author: DR Zamzuri Zakaria, International Islamic University Medical Centre, Kuantan, Pahang
Received: June 15, 2019; Published: June 26, 2019
Summary
We report a case of a young girl presented with history of swelling over right knee for a period of 3 years which clinical, laboratory investigations and initial radiographic features were suggestive of auto-immune arthritis. Subsequently an open biopsy was done, although cultures were negative for MTB or NTM, histopathological examination (HPE) reported a chronic granulomatous inflammation which was highly suggestive of Tuberculosis (TB). She received anti-tuberculosis treatment for a total of one year and noted marked improvement which was evidently shown clinically and radiograhically. Musculoskeletal TB is known to be a great mimicker of other pathology. A high index of suspicion is needed especially in a TB-prone area.
Case Report
This is a case of a 16 year old girl who presented to us on January 2018 with swelling over right knee for a period of 3 years associated with occasional pain but worsening a few weeks prior to our evaluation. She was able to perform daily activities prior to her referral from the district hospital. She had neither presentation of fever nor any constitutional symptoms. Noted swelling was spontaneous and there were no history of trauma to the knee. Further history taking, patient was noted to have morning joint stiffness.
On physical examination, she was healthy looking and not ill. She was afebrile. There was diffuse swelling of the right knee, non-erythematous and non-tender with no obvious skin changes. Patient was able to fully flexed and extend the knee without significant pain. Systemic examination was unremarkable. There were no significant lung findings. There was neither lymphadenopathy nor organomegaly.
Blood investigation showed no increment in leukocyte count, erythrocyte sedimentation rate (ESR) of 62mm/hr. Patient was positive for rheumatoid factor (RF) and antinuclear antibody (ANA) with titer 1:160 but anti-CCP was negative. Plain radiograph of the right knee revealed no bony or soft tissue abnormality.
Patient was referred to a rheumatologist for their expert opinion with the working diagnosis of rheumatoid arthritis as earlier clinical and laboratory findings were suggestive of it. After the patient’s review with the rheumatologist, she was referred back noting that it was unlikely to be rheumatoid arthritis.
A magnetic resonance imaging (MRI) was arranged for this patient and it showed marked synovial thickening, juxta-articular osseous and cartilaginous erosions with subchondral bone oedema at lateral femoral condyle. (Figure 1) The MRI concluded that it is suggestive of synovitis of right knee joint. Differentials are pigmented villonodular synovitis (PVNS) or inflammatory arthritis.
Subsequently she was scheduled for an open biopsy. An incision was made at suprapatellar pouch area and noted synovium hypertrophy which was fibrous in consistency and rice bodies. Synovial fluid was yellowish straw colored. No pus or blood noted. Synovial tissue was sent for histopathological examination and polymerase chain reaction (PCR) for DNA detection.
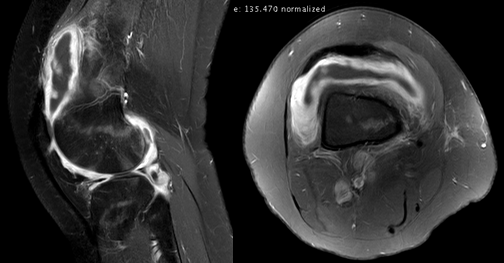
The pathologist has reported that PCR was negative for both MTB and NTM but histopathological examination reported a chronic granulamatous inflammation which was highly suggestive of Tuberculosis. Patient was then started on Antituberculosis drugs which consist of 2 months of intensive phase (EHRZ) and 10 months of continuation phase (HR). Patient was followed up on weekly basis for the first 1 month to assess for tolerance towards anti-TB drugs and subsequently was seen once a month. During follow ups, there was marked improvement in knee swelling and pain. A MRI was performed again post treatment of anti-TB and it showed a resolving synovial thickening and joint effusion which was suggestive of good response to treatment (Figure 2).

Figure 2: T2 weighted sagittal and axial view MRI of the left knee post anti-tuberculosis treatment.
Discussion
Tuberculosis (TB) is an ancient disease. Mummified remains of ancient Egyptians show evidence of tubercular disease, and the earliest documented case of tuberculosis spondylitis was written in Sanskrit dating back to 1500 BC(Lidder., et al. 2009). It is no longer confined to undeveloped or developing nations. An increased incidence of patients with TB has been observed even in developed countries due to pandemic human immunodeficiency virus infection, immigration from endemic areas, alcoholism, chronic kidney disorders, immuno-suppressive therapy, drug addiction, intraarticular steroid injection and systemic illness(Uboldi, Limonta, Ferrua, Manunta, & Pellegrini, n.d.). No age is exempted.
Mycobacterium tuberculosis is a nonmotile, strictly aerobic organism consisting of pleomorphic rods lacking an outer cell membrane. It is a slow-growing organism and humans are its only reservoir in nature. The particular virulence of the organism is, in part, a result of its ability to enter cells, to grow intracellularly, and to interfere with the effects of toxic oxygen intermediates. Transmission is via droplet spread.
Extra-pulmonary tuberculosis (TB) is reported in less than one in five cases with the knee affected in 8% after the spine and hip (Mah & Bux, 2006). Generally, TB knee is usually monoarticular, and is the 3rd most common site(Al-sayyad & Abumunaser, 2011). The large joints such as the hip and knee are most commonly involved. Diagnosis of tuberculosis arthritis is not an easy feat and often overlooked especially during early presentation of the disease.
TB arthritis presents usually as chronic pain, swelling, local tenderness, warmth and progressive loss of function. Cold abscesses, sinuses and constitutional symptoms are common features. Radiographs demonstrate changes only after three to four weeks of infection, and initially soft tissue swelling may be the predominant feature. Later, a classic triad of radiological findings, known as the “Phemister triad” are seen, which include juxta-articular osteopenia, joint space narrowing, and erosions (Gad, Ahmed, Nassar, & Ginawi, 2011). Laboratory investigations may yield the classical, although non-specific findings of raised ESR, a leukocytosis, and high C-reactive protein. Histological patterns in tissue specimens will show a central necrotic area surrounded by histiocytes and occasional giant cells with nuclei positioned at the margin of the cell (Sh., et al. 2011).
Options for treatment once the diagnosis is confirmed must involve antituberculous chemotherapy, but surgery may be indicated to improve symptoms and quality of life in patients affected by joint infection. Treatment for TB in the first instance revolves around four reserved drugs: isoniazid, rifampicin, Pyrazinamide and ethambutol. Second-line treatments also are available to combat the increasingly common variant of multi-drug resistant TB (MDR-TB). Unlike for pulmonary TB, the treatment for bone and joint disease is a lengthier process, often requiring twelve to eighteen months of chemotherapy(Lidder., et al. 2009). Surgical management options include debridement, synovectomy, arthrodesis, and amputation, and success has been shown with primary joint arthoplasty.
However, our case differs from those reported as it did not have a typical presentation of TB knee and our patient was very well with no constitutional symptoms. Initial workout pointed more in the direction of an auto-immune arthritis. Radiographical findings were unremarkable even though the symptom has progress for 3 years. Differential diagnosis that we considered was TB due to its high prevalence in Sabah. Besides imaging, a synovial biopsy is essential to identify the causative agent. Hussain Gad ElKarim Ahmed et al describes in his paper that histopathology remains one of the most important methods for diagnosing tuberculosis, and in a high TB prevalent area histopathology is the reliable and a gold standard (as otherwise is the culture). However, it cannot differentiate changes caused by Mycobacterium Tuberculosis, non tuberculoses mycobacterium, or other granulomatous diseases.
Musculoskeletal TB is known to be a great mimicker of other pathology. A high index of suspicion is needed especially in a TB-prone area.
References
- Al-sayyad, M. J., & Abumunaser, L. A. brief report, 31(August) (2011): 398–401.
- Gad, H., Ahmed, E., Nassar, A. S., & Ginawi, I. (2011). Screening for Tuberculosis and Its Histological Pattern in Patients with Enlarged Lymph Node, 2011.
- Lidder, S., et al. Tuberculosis of the knee er ci on co m m us e ly co m er al on 1 (2009): 7–10.
- Mah E L and Bux S. “Tuberculous synovitis of the knee with unusually thick synovial granulation tissue: A Case Report”. The Internet Journal of Orthopedic Surgery 6.2 (2006): 2–6.
- Sh T., et al. “The Great Mimic Again? A Case of Tuberculosis Knee”. Malaysian Orthopaedic Journal 5.3 (2011): 32–34.
- Uboldi FM., et al. "Tuberculosis of the Knee: A Case Report and Literature Review". Joints 5.3 (2017): 10–13.
Citation:
Dr Zamzuri Zakaria., et al. “Synovial Tuberculosis Masquerading As Monoarticular Inflammatory Arthritis”. Orthopaedic
Surgery and Traumatology 3.1 (2019): 12-15.
Copyright: © 2019 Dr Zamzuri Zakaria., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.



































 Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.
Scientia Ricerca is licensed and content of this site is available under a Creative Commons Attribution 4.0 International License.